Abstract
Sudden cardiac death (SCD) is a pivotal health problem worldwide. The identification of subjects at increased risk of SCD is crucial for the accurate selection of candidates for implantable cardioverter defibrillator (ICD) therapy. Current strategies for arrhythmic stratification largely rely on left ventricular (LV) ejection fraction (EF), mostly measured by echocardiography, and New York Heart Association functional status for heart failure with reduced EF. For specific diseases, such as hypertrophic and arrhythmogenic cardiomyopathy, some risk scores have been proposed; however, these scores take into account some parameters that are a partial reflection of the global arrhythmic risk and show a suboptimal accuracy. Thanks to a more comprehensive evaluation, cardiac magnetic resonance (CMR) provides insights into the heart muscle (the so-called tissue characterization) identifying cardiac fibrosis as an arrhythmic substrate. Combining sequences before and after administration of contrast media and mapping techniques, CMR is able to characterize the myocardial tissue composition, shedding light on both intracellular and extracellular alterations. Over time, late gadolinium enhancement (LGE) emerged as solid prognostic marker, strongly associated with major arrhythmic events regardless of LVEF, adding incremental value over current strategy in ischemic heart disease and non-ischemic cardiomyopathies. The evidence on a potential prognostic role of mapping imaging is promising. However, mapping techniques require further investigation and standardization. Disclosing the arrhythmic substrate within the myocardium, CMR should be considered as part of a multiparametric approach to personalized arrhythmic stratification.


Similar content being viewed by others
Data availability
Not applicable.
References
Tan HL, Dagres N, Böttiger BW, Schwartz PJ (2018) European Sudden Cardiac Arrest network: towards Prevention, Education and New Effective Treatments (ESCAPE-NET). Eur Heart J 39:86–88. https://doi.org/10.1093/eurheartj/ehx758
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Bloma N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, Kirchhof P, Kjeldsen K, Kuck KH, Hernandez-Madrid A, Nikolaou N, Norekval TM, Spaulding C, Van Veldhuisen DJ, Kolh P, Lip GYH, Agewall S, Barón-Esquivias G, Boriani G, Budts W, Bueno H, Capodanno D, Carerj S, Crespo-Leiro MG, Czerny M, Deaton C, Dobrev D, Erol Ç, Galderisi M, Gorenek B, Kriebel T, Lambiase P, Lancellotti P, Lane DA, Lang I, Manolis AJ, Morais J, Moreno J, Piepoli MF, Rutten FH, Sredniawa B, Zamorano JL, Zannad F, Aboyans V, Achenbach S, Badimon L, Baumgartner H, Bax JJ, Dean V, Fitzsimons D, Gaemperli O, Nihoyannopoulos P, Ponikowski P, Roffi M, Torbicki A, Vaz Carneiro A, Windecker S, Piruzyan A, Roithinger FX, Mairesse GH, Goronja B, Shalganov T, Puljević D, Antoniades L, Kautzner J, Larsen JM, Aboulmaaty M, Kampus P, Hedman A, Kamcevska-Dobrkovic L, Piot O, Etsadashvili K, Eckardt L, Deftereos S, Gellér L, Gizurarson S, Keane D, Haim M, Della Bella P, Abdrakhmanov A, Mirrakhimov A, Kalejs O, Ben Lamin H, Marinskis G, Groben L, Sammut M, Raducan A, Chaib A, Tande PM, Lenarczyk R, Morgado FB, Vatasescu R, Mikhaylov EN, Hlivak P, Arenal A, Jensen-Urstad M, Sticherling C, Zeppenfeld K, Chettaoui R, Demir M, Duncan E, Parkhomenko A (2015) 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death the task force for the Management of Patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. https://doi.org/10.1093/eurheartj/ehv316
J.J. Goldberger, M.E. Cain, S.H. Hohnloser, A.H. Kadish, B.P. Knight, M.S. Lauer, B.J. Maron, R.L. Page, R.S. Passman, D. Siscovick, W.G. Stevenson, D.P. Zipes, American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the America, Circulation. (2008). doi:https://doi.org/10.1161/CIRCULATIONAHA.107.189375
Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G (2006) Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. J Am Med Assoc. https://doi.org/10.1001/jama.296.13.1593
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez-Juanatey JR, Harjola V-P, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J, Nihoyannopoulos P, Nistri S, Pieper PG, Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H (2014) European Society of Cardiology Guidelines on diagnosis and management of hypertrophic cardiomyopathy. Eur Heart J
Towbin JA, McKenna WJ, Abrams DJ, Ackerman MJ, Calkins H, Darrieux FCC, Daubert JP, de Chillou C, DePasquale EC, Desai MY, Estes NAM, Hua W, Indik JH, Ingles J, James CA, John RM, Judge DP, Keegan R, Krahn AD, Link MS, Marcus FI, McLeod CJ, Mestroni L, Priori SG, Saffitz JE, Sanatani S, Shimizu W, van Tintelen JP, Wilde AAM, Zareba W (2019) 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy. Hear, Rhythm. https://doi.org/10.1016/j.hrthm.2019.05.007
Lang RM, Badano LP, Victor MA, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Retzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2014.10.003
Pocock SJ, Ariti CA, McMurray JJV, Maggioni A, Køber L, Squire IB, Swedberg K, Dobson J, Poppe KK, Whalley GA, Doughty RN (2013) Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J. https://doi.org/10.1093/eurheartj/ehs337
Køber L, Thune JJ, Nielsen JC, Haarbo J, Videbæk L, Korup E, Jensen G, Hildebrandt P, Steffensen FH, Bruun NE, Eiskjær H, Brandes A, Thøgersen AM, Gustafsson F, Egstrup K, Videbæk R, Hassager C, Svendsen JH, Høfsten DE, Torp-Pedersen C, Pehrson S (2016) Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med 375:1221–1230. https://doi.org/10.1056/NEJMoa1608029
M. Merlo, P. Gentile, J. Artico, A. Cannatà, A. Paldino, G. De Angelis, G. Barbati, M. Alonge, M. Gigli, B. Pinamonti, F. Ramani, M. Zecchin, F. Pirozzi, D. Stolfo, G. Sinagra, Arrhythmic risk stratification in patients with dilated cardiomyopathy and intermediate left ventricular dysfunction, J. Cardiovasc. Med. (Hagerstown). (2019). doi:https://doi.org/10.2459/JCM.0000000000000792
Vaduganathan M, Michel A, Hall K, Mulligan C, Nodari S, Shah SJ, Senni M, Triggiani M, Butler J, Gheorghiade M (2016) Spectrum of epidemiological and clinical findings in patients with heart failure with preserved ejection fraction stratified by study design: a systematic review. Eur J Heart Fail. https://doi.org/10.1002/ejhf.442
M.R. Zile, W.H. Gaasch, I.S. Anand, M. Haass, W.C. Little, A.B. Miller, J. Lopez-Sendon, J.R. Teerlink, M. White, J.J. McMurray, M. Komajda, R. McKelvie, A. Ptaszynska, S.J. Hetzel, B.M. Massie, P.E. Carson, Mode of death in patients with heart failure and a preserved ejection fraction: results from the irbesartan in heart failure with preserved ejection fraction study (I-Preserve) Trial, Circulation. (2010). doi:https://doi.org/10.1161/CIRCULATIONAHA.109.909614
Mele D, Nardozza M, Ferrari R (2018) Left ventricular ejection fraction and heart failure: an indissoluble marriage? Eur J Heart Fail. https://doi.org/10.1002/ejhf.1071
M.A. Konstam, F.M. Abboud, Ejection fraction: misunderstood and overrated (changing the paradigm in categorizing heart failure), Circulation. (2017). doi:https://doi.org/10.1161/CIRCULATIONAHA.116.025795
G. Pontone, A.I. Guaricci, D. Andreini, A. Solbiati, M. Guglielmo, S. Mushtaq, A. Baggiano, V. Beltrama, L. Fusini, C. Rota, C. Segurini, E. Conte, P. Gripari, A. Dello Russo, M. Moltrasio, F. Tundo, F. Lombardi, G. Muscogiuri, V. Lorenzoni, C. Tondo, P. Agostoni, A.L. Bartorelli, M. Pepi, Prognostic benefit of cardiac magnetic resonance over transthoracic echocardiography for the assessment of ischemic and nonischemic dilated cardiomyopathy patients referred for the evaluation of primary prevention implantable cardioverter-defibrillator therapy, Circ. Cardiovasc. Imaging. (2016). doi:https://doi.org/10.1161/CIRCIMAGING.115.004956
Jenkins C, Moir S, Chan J, Rakhit D, Haluska B, Marwick TH (2009) Left ventricular volume measurement with echocardiography: a comparison of left ventricular opacification, three-dimensional echocardiography, or both with magnetic resonance imaging. Eur Heart J. https://doi.org/10.1093/eurheartj/ehn484
P.A. Pellikka, L. She, T.A. Holly, G. Lin, P. Varadarajan, R.G. Pai, R.O. Bonow, G.M. Pohost, J.A. Panza, D.S. Berman, D.L. Prior, F.M. Asch, S. Borges-Neto, P. Grayburn, H.R. Al-Khalidi, K. Miszalski-Jamka, P. Desvigne-Nickens, K.L. Lee, E.J. Velazquez, J.K. Oh, Variability in ejection fraction measured by echocardiography, gated single-photon emission computed tomography, and cardiac magnetic resonance in patients with coronary artery disease and left ventricular dysfunction, JAMA Netw. Open. (2018). doi:https://doi.org/10.1001/jamanetworkopen.2018.1456
de Haan S, de Boer K, Commandeur J, Beek AM, van Rossum AC, Allaart CP (2014) Assessment of left ventricular ejection fraction in patients eligible for ICD therapy: discrepancy between cardiac magnetic resonance imaging and 2D echocardiography. Netherlands Hear J. https://doi.org/10.1007/s12471-014-0594-0
Joshi SB, Connelly KA, Jimenez-Juan L, Hansen M, Kirpalani A, Dorian P, Mangat I, Al-Hesayen A, Crean AM, Wright GA, Yan AT, Leong-Poi H (2012) Potential clinical impact of cardiovascular magnetic resonance assessment of ejection fraction on eligibility for cardioverter defibrillator implantation. J Cardiovasc Magn Reson. https://doi.org/10.1186/1532-429X-14-69
F. Contijoch, K. Rogers, H. Rears, M. Shahid, P. Kellman, J. Gorman, R.C. Gorman, P. Yushkevich, E.S. Zado, G.E. Supple, F.E. Marchlinski, W.R.T. Witschey, Y. Han, Quantification of left ventricular function with premature ventricular complexes reveals variable hemodynamics, Circ. Arrhythmia Electrophysiol. 9 (2016). doi:https://doi.org/10.1161/CIRCEP.115.003520
Akhtari S, Chuang ML, Salton CJ, Berg S, Kissinger KV, Goddu B, O’Donnell CJ, Manning WJ (2018) Effect of isolated left bundle-branch block on biventricular volumes and ejection fraction: a cardiovascular magnetic resonance assessment. J Cardiovasc Magn Reson 20:66. https://doi.org/10.1186/s12968-018-0457-8
N.S. Peters, A.L. Wit, Myocardial architecture and ventricular arrhythmogenesis, Circulation. (1998). doi:https://doi.org/10.1161/01.CIR.97.17.1746
Di Marco A, Anguera I, Schmitt M, Klem I, Neilan TG, White JA, Sramko M, Masci PG, Barison A, Mckenna P, Mordi I, Haugaa KH, Leyva F, Rodriguez Capitán J, Satoh H, Nabeta T, Dallaglio PD, Campbell NG, Sabaté X, Cequier Á (2017) Late gadolinium enhancement and the risk for ventricular arrhythmias or sudden death in dilated cardiomyopathy. JACC Hear Fail 5:28–38. https://doi.org/10.1016/j.jchf.2016.09.017
Disertori M, Rigoni M, Pace N, Casolo G, Masè M, Gonzini L, Lucci D, Nollo G, Ravelli F (2016) Myocardial fibrosis assessment by LGE is a powerful predictor of ventricular tachyarrhythmias in ischemic and nonischemic LV dysfunction: a meta-analysis. JACC Cardiovasc, Imaging. https://doi.org/10.1016/j.jcmg.2016.01.033
Ganesan AN, Gunton J, Nucifora G, McGavigan AD, Selvanayagam JB (2018) Impact of late gadolinium enhancement on mortality, sudden death and major adverse cardiovascular events in ischemic and nonischemic cardiomyopathy: a systematic review and meta-analysis. Int J Cardiol. https://doi.org/10.1016/j.ijcard.2017.10.094
V.O. Puntmann, T. Voigt, Z. Chen, M. Mayr, R. Karim, K. Rhode, A. Pastor, G. Carr-White, R. Razavi, T. Schaeffter, E. Nagel, Native T1 mapping in differentiation of normal myocardium from diffuse disease in hypertrophic and dilated cardiomyopathy., JACC. Cardiovasc. Imaging. 6 (2013) 475–484. doi:https://doi.org/10.1016/j.jcmg.2012.08.019
D.R. Messroghli, J.C. Moon, V.M. Ferreira, L. Grosse-Wortmann, T. He, P. Kellman, J. Mascherbauer, R. Nezafat, M. Salerno, E.B. Schelbert, A.J. Taylor, R. Thompson, M. Ugander, R.B. Van Heeswijk, M.G. Friedrich, Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2 and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI), J. Cardiovasc. Magn. Reson. (2017). doi:https://doi.org/10.1186/s12968-017-0389-8
Iles LM, Ellims AH, Llewellyn H, Hare JL, Kaye DM, McLean CA, Taylor AJ (2015) Histological validation of cardiac magnetic resonance analysis of regional and diffuse interstitial myocardial fibrosis. Eur. Heart J. Cardiovasc, Imaging. https://doi.org/10.1093/ehjci/jeu182
P. Thavendiranathan, M. Walls, S. Giri, D. Verhaert, S. Rajagopalan, S. Moore, O.P. Simonetti, S. V Raman, Improved detection of myocardial involvement in acute inflammatory cardiomyopathies using T2 mapping., Circ. Cardiovasc. Imaging. 5 (2012) 102–110. doi:https://doi.org/10.1161/CIRCIMAGING.111.967836
Lurz JA, Luecke C, Lang D, Besler C, Rommel K-P, Klingel K, Kandolf R, Adams V, Schöne K, Hindricks G, Schuler G, Linke A, Thiele H, Gutberlet M, Lurz P (2018) CMR–derived extracellular volume fraction as a marker for myocardial fibrosis. JACC Cardiovasc Imaging 11:38–45. https://doi.org/10.1016/j.jcmg.2017.01.025
Vita T, Gräni C, Abbasi SA, Neilan TG, Rowin E, Kaneko K, Coelho-Filho O, Watanabe E, Mongeon F-P, Farhad H, Rassi CH, Choi YL, Cheng K, Givertz MM, Blankstein R, Steigner M, Aghayev A, Jerosch-Herold M, Kwong RY (2019) Comparing CMR mapping methods and myocardial patterns toward heart failure outcomes in nonischemic dilated cardiomyopathy. JACC Cardiovasc Imaging 12:1659–1669. https://doi.org/10.1016/j.jcmg.2018.08.021
Miller CA, Naish JH, Bishop P, Coutts G, Clark D, Zhao S, Ray SG, Yonan N, Williams SG, Flett AS, Moon JC, Greiser A, Parker GJM, Schmitt M (2013) Comprehensive validation of cardiovascular magnetic resonance techniques for the assessment of myocardial extracellular volume. Circ. Cardiovasc. Imaging. 6:373–383. https://doi.org/10.1161/CIRCIMAGING.112.000192
Barison A, Grigoratos C, Todiere G, Aquaro GD (2015) Myocardial interstitial remodelling in non-ischaemic dilated cardiomyopathy: insights from cardiovascular magnetic resonance. Heart Fail Rev 20:731–749. https://doi.org/10.1007/s10741-015-9509-4
Selvanayagam JB, Hartshorne T, Billot L, Grover S, Hillis GS, Jung W, Krum H, Prasad S, McGavigan AD (2017) Cardiovascular magnetic resonance-GUIDEd management of mild to moderate left ventricular systolic dysfunction (CMR GUIDE): study protocol for a randomized controlled trial. Ann Noninvasive Electrocardiol. https://doi.org/10.1111/anec.12420
McCrohon JA, Moon JCC, Prasad SK, McKenna WJ, Lorenz CH, Coats AJS, Pennell DJ (2003) Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation. 108:54–59. https://doi.org/10.1161/01.CIR.0000078641.19365.4C
Soriano CJ, Ridocci F, Estornell J, Jimenez J, Martinez V, De Velasco JA (2005) Noninvasive diagnosis of coronary artery disease in patients with heart failure and systolic dysfunction of uncertain etiology, using late gadolinium-enhanced cardiovascular magnetic resonance. J Am Coll Cardiol 45:743–748. https://doi.org/10.1016/j.jacc.2004.11.037
A.T. Yan, A.J. Shayne, K.A. Brown, S.N. Gupta, C.W. Chan, T.M. Luu, M.F. Di Carli, H.G. Reynolds, W.G. Stevenson, R.Y. Kwong, Characterization of the peri-infarct zone by contrast-enhanced cardiac magnetic resonance imaging is a powerful predictor of post-myocardial infarction mortality, Circulation. (2006). doi:https://doi.org/10.1161/CIRCULATIONAHA.106.613414
A. Schmidt, C.F. Azevedo, A. Cheng, S.N. Gupta, D.A. Bluemke, T.K. Foo, G. Gerstenblith, R.G. Weiss, E. Marbán, G.F. Tomaselli, J.A.C. Lima, K.C. Wu, Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction, Circulation. (2007). doi:https://doi.org/10.1161/CIRCULATIONAHA.106.653568
Jablonowski R, Chaudhry U, Van Der Pals J, Engblom H, Arheden H, Heiberg E, Wu KC, Borgquist R, Carlsson M (2017) Cardiovascular magnetic resonance to predict appropriate implantable cardioverter defibrillator therapy in ischemic and nonischemic cardiomyopathy patients using late gadolinium enhancement border zone comparison of four analysis methods. Circ. Cardiovasc, Imaging. https://doi.org/10.1161/CIRCIMAGING.116.006105
Watanabe E, Abbasi SA, Heydari B, Coelho-Filho OR, Shah R, Neilan TG, Murthy VL, Mongeon F-P, Barbhaiya C, Jerosch-Herold M, Blankstein R, Hatabu H, van der Geest RJ, Stevenson WG, Kwong RY (2014) Infarct tissue heterogeneity by contrast-enhanced magnetic resonance imaging is a novel predictor of mortality in patients with chronic coronary artery disease and left ventricular dysfunction. Circ Cardiovasc Imaging 7:887–894. https://doi.org/10.1161/CIRCIMAGING.113.001293
J. Acosta, J. Fernández-Armenta, R. Borràs, I. Anguera, F. Bisbal, J. Martí-Almor, J.M. Tolosana, D. Penela, D. Andreu, D. Soto-Iglesias, R. Evertz, M. Matiello, C. Alonso, R. Villuendas, T.M. de Caralt, R.J. Perea, J.T. Ortiz, X. Bosch, L. Serra, X. Planes, A. Greiser, O. Ekinci, L. Lasalvia, L. Mont, A. Berruezo, Scar characterization to predict life-threatening arrhythmic events and sudden cardiac death in patients with cardiac resynchronization therapy, JACC Cardiovasc. Imaging. 11 (2018) 561–572. doi:https://doi.org/10.1016/j.jcmg.2017.04.021
Z. Chen, M. Sohal, T. Voigt, E. Sammut, C. Tobon-Gomez, N. Child, T. Jackson, A. Shetty, J. Bostock, M. Cooklin, M. O’Neill, M. Wright, F. Murgatroyd, J. Gill, G. Carr-White, A. Chiribiri, T. Schaeffter, R. Razavi, C.A. Rinaldi, Myocardial tissue characterization by cardiac magnetic resonance imaging using T1 mapping predicts ventricular arrhythmia in ischemic and non-ischemic cardiomyopathy patients with implantable cardioverter-defibrillators, Hear. Rhythm. (2015). doi:https://doi.org/10.1016/j.hrthm.2014.12.020
G. Pontone, A.I. Guaricci, D. Andreini, G. Ferro, M. Guglielmo, A. Baggiano, L. Fusini, G. Muscogiuri, V. Lorenzoni, S. Mushtaq, E. Conte, A. Annoni, A. Formenti, M.E. Mancini, P. Carità, M. Verdecchia, S. Pica, F. Fazzari, N. Cosentino, G. Marenzi, M.G. Rabbat, P. Agostoni, A.L. Bartorelli, M. Pepi, P.G. Masci, Prognostic stratification of patients with ST-segment-elevation myocardial infarction (PROSPECT): a cardiac magnetic resonance study, Circ. Cardiovasc. Imaging. (2017). doi:https://doi.org/10.1161/CIRCIMAGING.117.006428
Stone GW, Selker HP, Thiele H, Patel MR, Udelson JE, Ohman EM, Maehara A, Eitel I, Granger CB, Jenkins PL, Nichols M, Ben-Yehuda O (2016) Relationship between infarct size and outcomes following primary PCI patient-level analysis from 10 randomized trials. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2016.01.069
Izquierdo M, Ruiz-Granell R, Bonanad C, Chaustre F, Gomez C, Ferrero A, Lopez-Lereu P, Monmeneu JV, Nuñez J, Chorro FJ, Bodi V (2013) Value of early cardiovascular magnetic resonance for the prediction of adverse arrhythmic cardiac events after a first noncomplicated ST-segment-elevation myocardial infarction. Circ. Cardiovasc, Imaging. https://doi.org/10.1161/CIRCIMAGING.113.000702
Carrick D, Haig C, Rauhalammi S, Ahmed N, Mordi I, McEntegart M, Petrie MC, Eteiba H, Hood S, Watkins S, Lindsay M, Mahrous A, Ford I, Tzemos N, Sattar N, Welsh P, Radjenovic A, Oldroyd KG, Berry C (2016) Prognostic significance of infarct core pathology revealed by quantitative non-contrast in comparison with contrast cardiac magnetic resonance imaging in reperfused ST-elevation myocardial infarction survivors. Eur Heart J. https://doi.org/10.1093/eurheartj/ehv372
Kidambi A, Motwani M, Uddin A, Ripley DP, McDiarmid AK, Swoboda PP, Broadbent DA, Al Musa T, Erhayiem B, Leader J, Croisille P, Clarysse P, Greenwood JP, Plein S (2017) Myocardial extracellular volume estimation by CMR predicts functional recovery following acute MI. JACC Cardiovasc, Imaging. https://doi.org/10.1016/j.jcmg.2016.06.015
Baroldi G, Silver MD, De Maria R, Parodi O, Pellegrini A (1997) Lipomatous metaplasia in left ventricular scar. Can J Cardiol 13:65–71 http://www.ncbi.nlm.nih.gov/pubmed/9039067
Mordi I, Radjenovic A, Stanton T, Gardner RS, McPhaden A, Carrick D, Berry C, Tzemos N (2015) Prevalence and prognostic significance of lipomatous metaplasia in patients with prior myocardial infarction. JACC Cardiovasc Imaging 8:1111–1112. https://doi.org/10.1016/j.jcmg.2014.07.024
Pouliopoulos J, Chik WWB, Kanthan A, Sivagangabalan G, Barry MA, Fahmy PNA, Midekin C, Lu J, Kizana E, Thomas SP, Thiagalingam A, Kovoor P (2013) Intramyocardial adiposity after myocardial infarction. Circulation. 128:2296–2308. https://doi.org/10.1161/CIRCULATIONAHA.113.002238
Merlo M, Cannata A, Gobbo M, Stolfo D, Elliott PM, Sinagra G (2018) Evolving concepts in dilated cardiomyopathy. Eur J Heart Fail 20:228–239. https://doi.org/10.1002/ejhf.1103
Merlo M, Caiffa T, Gobbo M, Adamo L, Sinagra G (2018) Reverse remodeling in dilated cardiomyopathy: insights and future perspectives. IJC Hear Vasc 18:52–57. https://doi.org/10.1016/j.ijcha.2018.02.005
Porcari A, De Angelis G, Romani S, Paldino A, Artico J, Cannatà A, Gentile P, Pinamonti B, Merlo M, Sinagra G (2019) Current diagnostic strategies for dilated cardiomyopathy: a comparison of imaging techniques. Expert Rev. Cardiovasc, Ther. https://doi.org/10.1080/14779072.2019.1550719
Zecchin M, Merlo M, Pivetta A, Barbati G, Lutman C, Gregori D, Serdoz LV, Bardari S, Magnani S, Di Lenarda A, Proclemer A, Sinagra G (2012) How can optimization of medical treatment avoid unnecessary implantable cardioverter-defibrillator implantations in patients with idiopathic dilated cardiomyopathy presenting with “sCD-HeFT Criteria?,”. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2011.10.033
Losurdo P, Stolfo D, Merlo M, Barbati G, Gobbo M, Gigli M, Ramani F, Pinamonti B, Zecchin M, Finocchiaro G, Mestroni L, Sinagra G (2016) Early arrhythmic events in idiopathic dilated cardiomyopathy. JACC Clin, Electrophysiol. https://doi.org/10.1016/j.jacep.2016.05.002
Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S, Morarji K, Brown TDH, Ismail NA, Dweck MR, Di Pietro E, Roughton M, Wage R, Daryani Y, O’Hanlon R, Sheppard MN, Alpendurada F, Lyon AR, Cook SA, Cowie MR, Assomull RG, Pennell DJ, Prasad SK (2013) Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA - J. Am. Med, Assoc. https://doi.org/10.1001/jama.2013.1363
Halliday BP, Cleland JGF, Goldberger JJ, Prasad SK (2017) Personalizing risk stratification for sudden death in dilated cardiomyopathy. Circulation. 136:215–231. https://doi.org/10.1161/CIRCULATIONAHA.116.027134
Iles L, Pfluger H, Lefkovits L, Butler MJ, Kistler PM, Kaye DM, Taylor AJ (2011) Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. J Am Coll Cardiol 57:821–828. https://doi.org/10.1016/j.jacc.2010.06.062
B.P. Halliday, A. Gulati, A. Ali, K. Guha, S. Newsome, M. Arzanauskaite, V.S. Vassiliou, A. Lota, C. Izgi, U. Tayal, Z. Khalique, C. Stirrat, D. Auger, N. Pareek, T.F. Ismail, S.D. Rosen, A. Vazir, F. Alpendurada, J. Gregson, M.P. Frenneaux, M.R. Cowie, J.G.F. Cleland, S.A. Cook, D.J. Pennell, S.K. Prasad, Association between midwall late gadolinium enhancement and sudden cardiac death in patients with dilated cardiomyopathy and mild and moderate left ventricular systolic dysfunction., Circulation. 135 (2017) 2106–2115. doi:https://doi.org/10.1161/CIRCULATIONAHA.116.026910
S. Nazarian, D.A. Bluemke, A.C. Lardo, M.M. Zviman, S.P. Watkins, T.L. Dickfeld, G.R. Meininger, A. Roguin, H. Calkins, G.F. Tomaselli, R.G. Weiss, R.D. Berger, J.A.C. Lima, H.R. Halperin, Magnetic resonance assessment of the substrate for inducible ventricular tachycardia in nonischemic cardiomyopathy, Circulation. (2005). doi:https://doi.org/10.1161/CIRCULATIONAHA.105.549659
Sasaki T, Miller CF, Hansford R, Zipunnikov V, Zviman MM, Marine JE, Spragg D, Cheng A, Tandri H, Sinha S, Kolandaivelu A, Zimmerman SL, Bluemke DA, Tomaselli GF, Berger RD, Halperin HR, Calkins H, Nazarian S (2013) Impact of nonischemic scar features on local ventricular electrograms and scar-related ventricular tachycardia circuits in patients with nonischemic cardiomyopathy. Circ, Arrhythmia Electrophysiol. https://doi.org/10.1161/CIRCEP.113.000159
Marume K, Noguchi T, Tateishi E, Morita Y, Kamakura T, Ishibashi K, Noda T, Miura H, Nishimura K, Nakai M, Yamada N, Tsujita K, Anzai T, Kusano K, Ogawa H, Yasuda S (2018) Mortality and sudden cardiac death risk stratification using the noninvasive combination of wide QRS duration and late gadolinium enhancement in idiopathic dilated cardiomyopathy. Circ, Arrhythmia Electrophysiol. https://doi.org/10.1161/CIRCEP.117.006233
Elming MB, Hammer-Hansen S, Voges I, Nyktari E, Raja AA, Svendsen JH, Pehrson S, Signorovitch J, Køber L, Prasad SK, Thune JJ (2019) Myocardial fibrosis and the effect of primary prophylactic defibrillator implantation in patients with non-ischemic systolic heart failure—DANISH-MRI. Am Heart J. https://doi.org/10.1016/j.ahj.2019.10.020
Kalra R, Shenoy C (2019) Identifying nonischemic cardiomyopathy patients who would benefit from an implantable cardioverter-defibrillator: can late gadolinium enhancement on cardiovascular magnetic resonance imaging help? Am Heart J. https://doi.org/10.1016/j.ahj.2019.12.010
Gutman SJ, Costello BT, Papapostolou S, Voskoboinik A, Iles L, Ja J, Hare JL, Ellims A, Kistler PM, Marwick TH, Taylor AJ (2019) Reduction in mortality from implantable cardioverter-defibrillators in non-ischaemic cardiomyopathy patients is dependent on the presence of left ventricular scar. Eur Heart J. https://doi.org/10.1093/eurheartj/ehy437
Halliday BP, Baksi AJ, Gulati A, Ali A, Newsome S, Izgi C, Arzanauskaite M, Lota A, Tayal U, Vassiliou VS, Gregson J, Alpendurada F, Frenneaux MP, Cook SA, Cleland JGF, Pennell DJ, Prasad SK (2018) Outcome in dilated cardiomyopathy related to the extent, location, and pattern of late gadolinium enhancement. JACC Cardiovasc, Imaging. https://doi.org/10.1016/j.jcmg.2018.07.015
Puntmann VO, Carr-White G, Jabbour A, Yu CY, Gebker R, Kelle S, Hinojar R, Doltra A, Varma N, Child N, Rogers T, Suna G, Arroyo Ucar E, Goodman B, Khan S, Dabir D, Herrmann E, Zeiher AM, Nagel E (2016) T1-mapping and outcome in nonischemic cardiomyopathy all-cause mortality and heart failure. JACC Cardiovasc, Imaging. https://doi.org/10.1016/j.jcmg.2015.12.001
Nakamori S, Bui AH, Jang J, El-Rewaidy HA, Kato S, Ngo LH, Josephson ME, Manning WJ, Nezafat R (2018) Increased myocardial native T1 relaxation time in patients with nonischemic dilated cardiomyopathy with complex ventricular arrhythmia. J Magn Reson Imaging. https://doi.org/10.1002/jmri.25811
Nakamori S, Dohi K, Ishida M, Goto Y, Imanaka-Yoshida K, Omori T, Goto I, Kumagai N, Fujimoto N, Ichikawa Y, Kitagawa K, Yamada N, Sakuma H, Ito M (2018) Native T1 mapping and extracellular volume mapping for the assessment of diffuse myocardial fibrosis in dilated cardiomyopathy. JACC Cardiovasc, Imaging. https://doi.org/10.1016/j.jcmg.2017.04.006
Paldino A, De Angelis G, Merlo M, Gigli M, Dal Ferro M, Severini GM, Mestroni L, Sinagra G (2018) Genetics of dilated cardiomyopathy: clinical implications. Curr Cardiol Rep. https://doi.org/10.1007/s11886-018-1030-7
A.L.P. Caforio, S. Pankuweit, E. Arbustini, C. Basso, J. Gimeno-Blanes, S.B. Felix, M. Fu, T. Helio, S. Heymans, R. Jahns, K. Klingel, A. Linhart, B. Maisch, W. McKenna, J. Mogensen, Y.M. Pinto, A. Ristic, H.-P. Schultheiss, H. Seggewiss, L. Tavazzi, G. Thiene, A. Yilmaz, P. Charron, P.M. Elliott, Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases., Eur. Heart J. 34 (2013) 2636–48, 2648a-2648d. doi:https://doi.org/10.1093/eurheartj/eht210
J.W. Mason, J.B. O’Connell, A. Herskowitz, N.R. Rose, B.M. McManus, M.E. Billingham, T.E. Moon, A clinical trial of immunosuppressive therapy for myocarditis. The Myocarditis Treatment Trial Investigators., N. Engl. J. Med. (1995). doi:https://doi.org/10.1056/NEJM199508033330501
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, Aletras A, Laissy J-P, Paterson I, Filipchuk NG, Kumar A, Pauschinger M, Liu P (2009) Cardiovascular magnetic resonance in myocarditis: a JACC White paper. J Am Coll Cardiol 53:1475–1487. https://doi.org/10.1016/j.jacc.2009.02.007
Grun S, Schumm J, Greulich S, Wagner A, Schneider S, Bruder O, Kispert E-M, Hill S, Ong P, Klingel K, Kandolf R, Sechtem U, Mahrholdt H (2012) Long-term follow-up of biopsy-proven viral myocarditis: predictors of mortality and incomplete recovery. J Am Coll Cardiol 59:1604–1615. https://doi.org/10.1016/j.jacc.2012.01.007
Gräni C, Eichhorn C, Bière L, Murthy VL, Agarwal V, Kaneko K, Cuddy S, Aghayev A, Steigner M, Blankstein R, Jerosch-Herold M, Kwong RY (2017) Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2017.08.050
G.D. Aquaro, M. Perfetti, G. Camastra, L. Monti, S. Dellegrottaglie, C. Moro, A. Pepe, G. Todiere, C. Lanzillo, A. Scatteia, M. Di Roma, G. Pontone, M. Perazzolo Marra, A. Barison, G. Di Bella, Cardiac MR with late gadolinium enhancement in acute myocarditis with preserved systolic function: ITAMY Study, J. Am. Coll. Cardiol. 70 (2017) 1977–1987. doi:https://doi.org/10.1016/j.jacc.2017.08.044
Sinagra G, Anzini M, Pereira NL, Bussani R, Finocchiaro G, Bartunek J, Merlo M (2016) Myocarditis in clinical practice. Mayo Clin Proc 91:1256–1266. https://doi.org/10.1016/j.mayocp.2016.05.013
Peretto G, Sala S, Rizzo S, Palmisano A, Esposito A, De Cobelli F, Campochiaro C, De Luca G, Foppoli L, Dagna L, Thiene G, Basso C, Della Bella P (2020) Ventricular arrhythmias in myocarditis. J Am Coll Cardiol 75:1046–1057. https://doi.org/10.1016/j.jacc.2020.01.036
Anzini M, Merlo M, Artico J, Sinagra G (2016) Arrhythmic risk prediction of acute myocarditis presenting with life-threatening ventricular tachyarrhythmias. Int J Cardiol 212:169–170. https://doi.org/10.1016/j.ijcard.2016.03.020
Francone M, Chimenti C, Galea N, Scopelliti F, Verardo R, Galea R, Carbone I, Catalano C, Fedele F, Frustaci A (2014) CMR sensitivity varies with clinical presentation and extent of cell necrosis in biopsy-proven acute myocarditis. JACC Cardiovasc Imaging 7:254–263. https://doi.org/10.1016/j.jcmg.2013.10.011
V.M. Ferreira, J. Schulz-Menger, G. Holmvang, C.M. Kramer, I. Carbone, U. Sechtem, I. Kindermann, M. Gutberlet, L.T. Cooper, P. Liu, M.G. Friedrich, Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations., J. Am. Coll. Cardiol. 72 (2018) 3158–3176. doi:https://doi.org/10.1016/j.jacc.2018.09.072
Spieker M, Haberkorn S, Gastl M, Behm P, Katsianos S, Horn P, Jacoby C, Schnackenburg B, Reinecke P, Kelm M, Westenfeld R, Bönner F (2017) Abnormal T2 mapping cardiovascular magnetic resonance correlates with adverse clinical outcome in patients with suspected acute myocarditis. J Cardiovasc Magn Reson. https://doi.org/10.1186/s12968-017-0350-x
J.A. Luetkens, R. Homsi, D. Dabir, D.L. Kuetting, C. Marx, J. Doerner, U. Schlesinger-Irsch, R. Andrié, A.M. Sprinkart, F.C. Schmeel, C. Stehning, R. Fimmers, J. Gieseke, C.P. Naehle, H.H. Schild, D.K. Thomas, Comprehensive cardiac magnetic resonance for short-term follow-up in acute myocarditis, J. Am. Heart Assoc. 5 (2016). doi:https://doi.org/10.1161/JAHA.116.003603
Anzini M, Merlo M, Sabbadini G, Barbati G, Finocchiaro G, Pinamonti B, Salvi A, Perkan A, Di Lenarda A, Bussani R, Bartunek J, Sinagra G (2013) Long-term evolution and prognostic stratification of biopsy-proven active myocarditis. Circulation. 128:2384–2394. https://doi.org/10.1161/CIRCULATIONAHA.113.003092
Gräni C, Bière L, Eichhorn C, Kaneko K, Agarwal V, Aghayev A, Steigner M, Blankstein R, Jerosch-Herold M, Kwong RY (2019) Incremental value of extracellular volume assessment by cardiovascular magnetic resonance imaging in risk stratifying patients with suspected myocarditis. Int. J. Cardiovasc, Imaging. https://doi.org/10.1007/s10554-019-01552-6
Moon JC, Messroghli DR, Kellman P, Piechnik SK, Robson MD, Ugander M, Gatehouse PD, Arai AE, Friedrich MG, Neubauer S, Schulz-Menger J, Schelbert EB (2013) Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J Cardiovasc Magn Reson 15:92. https://doi.org/10.1186/1532-429X-15-92
Aquaro GD, Ghebru Habtemicael Y, Camastra G, Monti L, Dellegrottaglie S, Moro C, Lanzillo C, Scatteia A, Di Roma M, Pontone G, Perazzolo Marra M, Barison A, Di Bella G (2019) Prognostic value of repeating cardiac magnetic resonance in patients with acute myocarditis. J Am Coll Cardiol 74:2439–2448. https://doi.org/10.1016/j.jacc.2019.08.1061
Birnie DH, Sauer WH, Bogun F, Cooper JM, Culver DA, Duvernoy CS, Judson MA, Kron J, Mehta D, Cosedis Nielsen J, Patel AR, Ohe T, Raatikainen P, Soejima K (2014) HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Hear. Rhythm. 11:1304–1323. https://doi.org/10.1016/j.hrthm.2014.03.043
Olivotto I, Maron MS, Autore C, Lesser JR, Rega L, Casolo G, De Santis M, Quarta G, Nistri S, Cecchi F, Salton CJ, Udelson JE, Manning WJ, Maron BJ (2008) Assessment and significance of left ventricular mass by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J Am Coll Cardiol 52:559–566. https://doi.org/10.1016/j.jacc.2008.04.047
Webb J, Villa A, Bekri I, Shome J, Teall T, Claridge S, Jackson T, Porter B, Ismail TF, Di Giovine G, Rinaldi CA, Carr-White G, Al-Fakih K, Razavi R, Chiribiri A (2017) Usefulness of cardiac magnetic resonance imaging to measure left ventricular wall thickness for determining risk scores for sudden cardiac death in patients with hypertrophic cardiomyopathy. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2017.01.021
M.S. Maron, J.J. Finley, J.M. Bos, T.H. Hauser, W.J. Manning, T.S. Haas, J.R. Lesser, J.E. Udelson, M.J. Ackerman, B.J. Maron, Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy, Circulation. (2008). doi:https://doi.org/10.1161/CIRCULATIONAHA.108.781401
X. Guo, C. Fan, L. Tian, Y. Liu, H. Wang, S. Zhao, F. Duan, X. Zhang, X. Zhao, F. Wang, H. Zhu, A. Lin, X. Wu, Y. Li, The clinical features, outcomes and genetic characteristics of hypertrophic cardiomyopathy patients with severe right ventricular hypertrophy, PLoS One. (2017). doi:https://doi.org/10.1371/journal.pone.0174118
Todiere G, Pisciella L, Barison A, Del Franco A, Zachara E, Piaggi P, Re F, Pingitore A, Emdin M, Lombardi M, Aquaro GD (2014) Abnormal T2-STIR magnetic resonance in hypertrophic cardiomyopathy: a marker of advanced disease and electrical myocardial instability. PLoS One 9:e111366. https://doi.org/10.1371/journal.pone.0111366
Melacini P, Corbetti F, Calore C, Pescatore V, Smaniotto G, Pavei A, Bobbo F, Cacciavillani L, Iliceto S (2008) Cardiovascular magnetic resonance signs of ischemia in hypertrophic cardiomyopathy. Int J Cardiol 128:364–373. https://doi.org/10.1016/j.ijcard.2007.06.023
Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG (2003) Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 349:1027–1035. https://doi.org/10.1056/NEJMoa025050
O’Mahony C, Jichi F, Ommen SR, Christiaans I, Arbustini E, Garcia-Pavia P, Cecchi F, Olivotto I, Kitaoka H, Gotsman I, Carr-White G, Mogensen J, Antoniades L, Mohiddin SA, Maurer MS, Tang HC, Geske JB, Siontis KC, Mahmoud KD, Vermeer A, Wilde A, Favalli V, Guttmann OP, Gallego-Delgado M, Dominguez F, Tanini I, Kubo T, Keren A, Bueser T, Waters S, Issa IF, Malcolmson J, Burns T, Sekhri N, Hoeger CW, Omar RZ, Elliott PM (2018) International External Validation Study of the 2014 European Society of Cardiology guidelines on sudden cardiac death prevention in hypertrophic cardiomyopathy (EVIDENCE-HCM). Circulation 137:1015–1023. https://doi.org/10.1161/CIRCULATIONAHA.117.030437
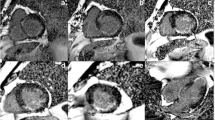
R.H. Chan, B.J. Maron, I. Olivotto, M.J. Pencina, G.E. Assenza, T. Haas, J.R. Lesser, C. Gruner, A.M. Crean, H. Rakowski, J.E. Udelson, E. Rowin, M. Lombardi, F. Cecchi, B. Tomberli, P. Spirito, F. Formisano, E. Biagini, C. Rapezzi, C.N. De Cecco, C. Autore, E.F. Cook, S.N. Hong, C.M. Gibson, W.J. Manning, E. Appelbaum, M.S. Maron, Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy, Circulation. 130 (2014) 484–495. doi:https://doi.org/10.1161/CIRCULATIONAHA.113.007094
Briasoulis A, Mallikethi-Reddy S, Palla M, Alesh I, Afonso L (2015) Myocardial fibrosis on cardiac magnetic resonance and cardiac outcomes in hypertrophic cardiomyopathy: a meta-analysis. Heart. 101:1406–1411. https://doi.org/10.1136/heartjnl-2015-307682
Weng Z, Yao J, Chan RH, He J, Yang X, Zhou Y, He Y (2016) Prognostic value of LGE-CMR in HCM. JACC Cardiovasc Imaging 9:1392–1402. https://doi.org/10.1016/j.jcmg.2016.02.031
Mentias A, Raeisi-Giglou P, Smedira NG, Feng K, Sato K, Wazni O, Kanj M, Flamm SD, Thamilarasan M, Popovic ZB, Lever HM, Desai MY (2018) Late gadolinium enhancement in patients with hypertrophic cardiomyopathy and preserved systolic function. J Am Coll Cardiol 72:857–870. https://doi.org/10.1016/j.jacc.2018.05.060
Todiere G, Nugara C, Gentile G, Negri F, Bianco F, Falletta C, Novo G, Di Bella G, De Caterina R, Zachara E, Re F, Clemenza F, Sinagra G, Emdin M, Aquaro GD (2019) Prognostic role of late gadolinium enhancement in patients with hypertrophic cardiomyopathy and low-to-intermediate sudden cardiac death risk score. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2019.07.023
Kozor R, Nordin S, Treibel TA, Rosmini S, Castelletti S, Fontana M, Captur G, Baig S, Steeds RP, Hughes D, Manisty C, Grieve SM, Figtree GA, Moon JC (2017) Insight into hypertrophied hearts: a cardiovascular magnetic resonance study of papillary muscle mass and T1 mapping. Eur Hear J - Cardiovasc Imaging 18:1034–1040. https://doi.org/10.1093/ehjci/jew187
Chu LC, Corona-Villalobos CP, Halushka MK, Zhang Y, Pozzessere C, Kamel IR, Pozios I, Van Der Geest RJ, Gai N, Abraham RM, Abraham TP, Bluemke DA, Zimmerman SL (2017) Structural and functional correlates of myocardial T1 mapping in 321 patients with hypertrophic cardiomyopathy. J Comput Assist Tomogr 41:653–660. https://doi.org/10.1097/RCT.0000000000000564
Kato S, Nakamori S, Bellm S, Jang J, Basha T, Maron M, Manning WJ, Nezafat R (2016) Myocardial native T1 time in patients with hypertrophic cardiomyopathy. Am J Cardiol 118:1057–1062. https://doi.org/10.1016/j.amjcard.2016.07.010
Kramer CM, Appelbaum E, Desai MY, Desvigne-Nickens P, DiMarco JP, Friedrich MG, Geller N, Heckler S, Ho CY, Jerosch-Herold M, Ivey EA, Keleti J, Kim D-Y, Kolm P, Kwong RY, Maron MS, Schulz-Menger J, Piechnik S, Watkins H, Weintraub WS, Wu P, Neubauer S (2015) Hypertrophic cardiomyopathy registry: the rationale and design of an international, observational study of hypertrophic cardiomyopathy. Am Heart J 170:223–230. https://doi.org/10.1016/j.ahj.2015.05.013
D. Dalal, K. Nasir, C. Bomma, K. Prakasa, H. Tandri, J. Piccini, A. Roguin, C. Tichnell, C. James, S.D. Russell, D.P. Judge, T. Abraham, P.J. Spevak, D.A. Bluemke, H. Calkins, Arrhythmogenic right ventricular dysplasia: a United States experience, Circulation. (2005). doi:https://doi.org/10.1161/CIRCULATIONAHA.105.542266
S. Sen-Chowdhry, P. Syrris, D. Ward, A. Asimaki, E. Sevdalis, W.J. McKenna, Clinical and genetic characterization of families with arrhythmogenic right ventricular dysplasia/cardiomyopathy provides novel insights into patterns of disease expression, Circulation. (2007). doi:https://doi.org/10.1161/CIRCULATIONAHA.106.660241
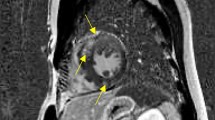
F.I. Marcus, W.J. McKenna, D. Sherrill, C. Basso, B. Bauce, D.A. Bluemke, H. Calkins, D. Corrado, M.G.P.J. Cox, J.P. Daubert, G. Fontaine, K. Gear, R. Hauer, A. Nava, M.H. Picard, N. Protonotarios, J.E. Saffitz, D.M.Y. Sanborn, J.S. Steinberg, H. Tandri, G. Thiene, J.A. Towbin, A. Tsatsopoulou, T. Wichter, W. Zareba, Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria., Eur. Heart J. 31 (2010) 806–814. doi:https://doi.org/10.1093/eurheartj/ehq025
Aquaro GD, Pingitore A, Di Bella G, Piaggi P, Gaeta R, Grigoratos C, Altinier A, Pantano A, Strata E, De Caterina R, Sinagra G, Emdin M (2018) Prognostic role of cardiac magnetic resonance in arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2018.08.007
Jain A, Tandri H, Calkis H, Bluemke DA (2008) Role of cardiovascular magnetic resonance imaging in arrhythmogenic right ventricular dysplasia. J Cardiovasc Magn Reson. https://doi.org/10.1186/1532-429X-10-32
Nucifora G, Muser D, Masci PG, Barison A, Rebellato L, Piccoli G, Daleffe E, Toniolo M, Zanuttini D, Facchin D, Lombardi M, Proclemer A (2014) Prevalence and prognostic value of concealed structural abnormalities in patients with apparently idiopathic ventricular arrhythmias of left versus right ventricular origin: a magnetic resonance imaging study. Circ, Arrhythmia Electrophysiol. https://doi.org/10.1161/CIRCEP.113.001172
Muser D, Santangeli P, Castro SA, Casado Arroyo R, Maeda S, Benhayon DA, Liuba I, Liang JJ, Sadek MM, Chahal A, Magnani S, Pieroni M, Santarossa E, Desjardins B, Dixit S, Garcia FC, Callans DJ, Frankel DS, Alavi A, Marchlinski FE, Selvanayagam JB, Nucifora G (2019) Risk stratification of patients with apparently idiopathic premature ventricular contractions. JACC Clin Electrophysiol 1040. https://doi.org/10.1016/j.jacep.2019.10.015
Aquaro GD, Barison A, Todiere G, Grigoratos C, Ait Ali L, Di Bella G, Emdin M, Festa P (2016) Usefulness of combined functional assessment by cardiac magnetic resonance and tissue characterization versus task force criteria for diagnosis of arrhythmogenic right ventricular cardiomyopathy. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2016.08.056
Negri F, De Luca A, Fabris E, Korcova R, Cernetti C, Grigoratos C, Aquaro GD, Nucifora G, Camici PG, Sinagra G (2019) Left ventricular noncompaction, morphological, and clinical features for an integrated diagnosis. Heart Fail Rev 24:315–323. https://doi.org/10.1007/s10741-018-9763-3
Arbustini E, Favalli V, Narula N, Serio A, Grasso M (2016) Left ventricular noncompaction: a distinct genetic cardiomyopathy? J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2016.05.096
Captur G, Muthurangu V, Cook C, Flett AS, Wilson R, Barison A, Sado DM, Anderson S, McKenna WJ, Mohun TJ, Elliott PM, Moon JC (2013) Quantification of left ventricular trabeculae using fractal analysis. J Cardiovasc Magn Reson 15:36. https://doi.org/10.1186/1532-429X-15-36
Grothoff M, Pachowsky M, Hoffmann J, Posch M, Klaassen S, Lehmkuhl L, Gutberlet M (2012) Value of cardiovascular MR in diagnosing left ventricular non-compaction cardiomyopathy and in discriminating between other cardiomyopathies. Eur Radiol 22:2699–2709. https://doi.org/10.1007/s00330-012-2554-7
Jacquier A, Thuny F, Jop B, Giorgi R, Cohen F, Gaubert JY, Vidal V, Bartoli JM, Habib G, Moulin G (2010) Measurement of trabeculated left ventricular mass using cardiac magnetic resonance imaging in the diagnosis of left ventricular non-compaction. Eur Heart J 31:1098–1104. https://doi.org/10.1093/eurheartj/ehp595
Petersen SE, Selvanayagam JB, Wiesmann F, Robson MD, Francis JM, Anderson RH, Watkins H, Neubauer S (2005) Left ventricular non-compaction. J Am Coll Cardiol 46:101–105. https://doi.org/10.1016/j.jacc.2005.03.045
R.E. Hershberger, J. Lindenfeld, L. Mestroni, C.E. Seidman, M.R.G. Taylor, J.A. Towbin, Heart Failure Society of America, Genetic evaluation of cardiomyopathy--a Heart Failure Society of America practice guideline., J. Card. Fail. 15 (2009) 83–97. doi:https://doi.org/10.1016/j.cardfail.2009.01.006
Nucifora G, Aquaro GD, Pingitore A, Masci PG, Lombardi M (2011) Myocardial fibrosis in isolated left ventricular non-compaction and its relation to disease severity. Eur J Heart Fail 13:170–176. https://doi.org/10.1093/eurjhf/hfq222
Mavrogeni S, Sfendouraki E, Theodorakis G, Kolovou G (2013) Diagnosis, severity grading and prognosis of left ventricular non-compaction using cardiovascular magnetic resonance. Int J Cardiol 167:598–599. https://doi.org/10.1016/j.ijcard.2012.09.234
Ashrith G, Gupta D, Hanmer J, Weiss RM (2014) Cardiovascular magnetic resonance characterization of left ventricular non-compaction provides independent prognostic information in patients with incident heart failure or suspected cardiomyopathy. J Cardiovasc Magn Reson. https://doi.org/10.1186/s12968-014-0064-2
Andreini D, Pontone G, Bogaert J, Roghi A, Barison A, Schwitter J, Mushtaq S, Vovas G, Sormani P, Aquaro GD, Monney P, Segurini C, Guglielmo M, Conte E, Fusini L, Dello Russo A, Lombardi M, Gripari P, Baggiano A, Fiorentini C, Lombardi F, Bartorelli AL, Pepi M, Masci PG (2016) Long-term prognostic value of cardiac magnetic resonance in left ventricle noncompaction. J Am Coll Cardiol 68:2166–2181. https://doi.org/10.1016/j.jacc.2016.08.053
A. Ivanov, D.S. Dabiesingh, G.P. Bhumireddy, A. Mohamed, A. Asfour, W.M. Briggs, J. Ho, S.A. Khan, A. Grossman, I. Klem, T.J. Sacchi, J.F. Heitner, Prevalence and prognostic significance of left ventricular noncompaction in patients referred for cardiac magnetic resonance imaging, Circ. Cardiovasc. Imaging. 10 (2017). doi:https://doi.org/10.1161/CIRCIMAGING.117.006174
Grigoratos C, Barison A, Ivanov A, Andreini D, Amzulescu M-S, Mazurkiewicz L, De Luca A, Grzybowski J, Masci PG, Marczak M, Heitner JF, Schwitter J, Gerber BL, Emdin M, Aquaro GD (2019) Meta-analysis of the prognostic role of late gadolinium enhancement and global systolic impairment in left ventricular noncompaction. JACC Cardiovasc Imaging 12:2141–2151. https://doi.org/10.1016/j.jcmg.2018.12.029
Zhou H, Lin X, Fang L, Zhao X, Ding H, Chen W, Xu R, Bai X, Wang Y, Fang Q (2016) Characterization of compacted myocardial abnormalities by cardiac magnetic resonance with native T1 mapping in left ventricular non-compaction patients: a comparison with late gadolinium enhancement. Circ J. https://doi.org/10.1253/circj.CJ-15-1269
Araujo-Filho JAB, Assuncao AN, Tavares de Melo MD, Bière L, Lima CR, Dantas RN, Nomura CH, Salemi VMC, Jerosch-Herold M, Parga JR (2018) Myocardial T1 mapping and extracellular volume quantification in patients with left ventricular non-compaction cardiomyopathy. Eur. Hear. J. - Cardiovasc. Imaging. 19:888–895. https://doi.org/10.1093/ehjci/jey022
Merlo M, Gobbo M, Stolfo D, Losurdo P, Ramani F, Barbati G, Pivetta A, Di Lenarda A, Anzini M, Gigli M, Pinamonti B, Sinagra G (2016) The prognostic impact of the evolution of RV function in idiopathic DCM. JACC Cardiovasc Imaging 9:1034–1042. https://doi.org/10.1016/j.jcmg.2016.01.027
Merlo M, Stolfo D, Gobbo M, Gabassi G, Barbati G, Naso P, Secoli G, Boscutti A, Ramani F, Gigli M, Pinamonti B, Sinagra G (2019) Prognostic impact of short-term changes of E/E’ ratio and left atrial size in dilated cardiomyopathy. Eur J Heart Fail 21:1294–1296. https://doi.org/10.1002/ejhf.1543
Stolfo D, De Luca A, Morea G, Merlo M, Vitrella G, Caiffa T, Barbati G, Rakar S, Korcova R, Perkan A, Pinamonti B, Pappalardo A, Berardini A, Biagini E, Saia F, Grigioni F, Rapezzi C, Sinagra G (2018) Predicting device failure after percutaneous repair of functional mitral regurgitation in advanced heart failure: implications for patient selection. Int J Cardiol 257:182–187. https://doi.org/10.1016/j.ijcard.2018.01.009
A. Porcari, M. Merlo, L. Crosera, D. Stolfo, G. Barbati, F. Biondi, G. De Angelis, A. Paldino, L. Pagnan, M. Belgrano, M.A. Cova, B. Pinamonti, G. Vitrella, G. Sinagra, Strain analysis reveals subtle systolic dysfunction in confirmed and suspected myocarditis with normal LVEF. A cardiac magnetic resonance study, Clin. Res. Cardiol. (2019). doi:https://doi.org/10.1007/s00392-019-01577-w
A. Cannatà, G. De Angelis, A. Boscutti, C. Normand, J. Artico, P. Gentile, M. Zecchin, S. Heymans, M. Merlo, G. Sinagra, Arrhythmic risk stratification in non-ischaemic dilated cardiomyopathy beyond ejection fraction, Heart. (2020). doi:https://doi.org/10.1136/heartjnl-2019-315942
Zeidan-Shwiri T, Yang Y, Lashevsky I, Kadmon E, Kagal D, Dick A, Laish Farkash A, Paul G, Gao D, Shurrab M, Newman D, Wright G, Crystal E (2015) Magnetic resonance estimates of the extent and heterogeneity of scar tissue in ICD patients with ischemic cardiomyopathy predict ventricular arrhythmia. Hear. Rhythm. 12:802–808. https://doi.org/10.1016/j.hrthm.2015.01.007
Alexandre J, Saloux E, Dugué AE, Lebon A, Lemaitre A, Roule V, Labombarda F, Provost N, Gomes S, Scanu P, Milliez P (2013) Scar extent evaluated by late gadolinium enhancement CMR: a powerful predictor of long term appropriate ICD therapy in patients with coronary artery disease. J Cardiovasc Magn Reson 15:12. https://doi.org/10.1186/1532-429X-15-12
Krittayaphong R, Saiviroonporn P, Boonyasirinant T, Udompunturak S (2011) Prevalence and prognosis of myocardial scar in patients with known or suspected coronary artery disease and normal wall motion. J Cardiovasc Magn Reson 13:2. https://doi.org/10.1186/1532-429X-13-2
Scott PA, Morgan JM, Carroll N, Murday DC, Roberts PR, Peebles CR, Harden SP, Curzen NP (2011) The extent of left ventricular scar quantified by late gadolinium enhancement MRI is associated with spontaneous ventricular arrhythmias in patients with coronary artery disease and implantable cardioverter-defibrillators. Circ Arrhythmia Electrophysiol 4:324–330. https://doi.org/10.1161/CIRCEP.110.959544
Kwon DH, Halley CM, Carrigan TP, Zysek V, Popovic ZB, Setser R, Schoenhagen P, Starling RC, Flamm SD, Desai MY (2009) Extent of left ventricular scar predicts outcomes in ischemic cardiomyopathy patients with significantly reduced systolic function. JACC Cardiovasc Imaging 2:34–44. https://doi.org/10.1016/j.jcmg.2008.09.010
Piers SRD, Everaerts K, van der Geest RJ, Hazebroek MR, Siebelink H-M, Pison LAFG, Schalij MJ, Bekkers SCAM, Heymans S, Zeppenfeld K (2015) Myocardial scar predicts monomorphic ventricular tachycardia but not polymorphic ventricular tachycardia or ventricular fibrillation in nonischemic dilated cardiomyopathy. Hear Rhythm 12:2106–2114. https://doi.org/10.1016/j.hrthm.2015.05.026
Masci PG, Doulaptsis C, Bertella E, Del Torto A, Symons R, Pontone G, Barison A, Droogné W, Andreini D, Lorenzoni V, Gripari P, Mushtaq S, Emdin M, Bogaert J, Lombardi M (2014) Incremental prognostic value of myocardial fibrosis in patients with non-ischemic cardiomyopathy without congestive heart failure. Circ Hear Fail 7:448–456. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000996
Assomull RG, Prasad SK, Lyne J, Smith G, Burman ED, Khan M, Sheppard MN, Poole-Wilson PA, Pennell DJ (2006) Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48:1977–1985. https://doi.org/10.1016/j.jacc.2006.07.049
Imazio M, Angelico G, Andriani M, Lobetti-Bodoni L, Davini O, Giustetto C, Rinaldi M (2018) Prevalence and prognostic impact of septal late gadolinium enhancement in acute myocarditis with or without preserved left ventricular function. Am J Cardiol 122:1955–1958. https://doi.org/10.1016/j.amjcard.2018.08.038
Maron MS, Appelbaum E, Harrigan CJ, Buros J, Gibson CM, Hanna C, Lesser JR, Udelson JE, Manning WJ, Maron BJ (2008) Clinical profile and significance of delayed enhancement in hypertrophic cardiomyopathy. Circ. Hear. Fail. 1:184–191. https://doi.org/10.1161/CIRCHEARTFAILURE.108.768119
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Porcari, A., De Luca, A., Grigoratos, C. et al. Arrhythmic risk stratification by cardiac magnetic resonance tissue characterization: disclosing the arrhythmic substrate within the heart muscle. Heart Fail Rev 27, 49–69 (2022). https://doi.org/10.1007/s10741-020-09986-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-020-09986-0