Abstract
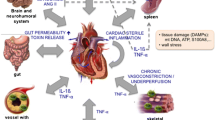
Cardiac injuries, like heart attacks, drive the secondary pathology with advanced heart failure. In this process, non-resolving inflammation is a prime component of accelerated cardiovascular disease and subsequent fatal events associated with imbalanced diet, physical inactivity, disrupted circadian rhythms, neuro-hormonal stress, and poly- or co-medication. Laboratory rodents have established that splenic leukocyte–directed resolution mechanisms are essential for cardiac repair after injury. Here, we discuss the impact of three lifestyle-related factors that are prime causes of derailed cardiac healing, putative non-resolving inflammation-resolution mechanisms in cardiovascular diseases, and progressive heart failure after cardiac injury. The presented review resurfaces the lifestyle-related risks and future research directions required to understand the molecular and cellular mechanisms between the causes of cardiovascular disease and their related consequences of non-resolving inflammation.


Similar content being viewed by others
References
Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, Jaarsma T, Krum H, Rastogi V, Rohde LE, Samal UC, Shimokawa H, Budi Siswanto B, Sliwa K, Filippatos G (2014) Heart failure: preventing disease and death worldwide. ESC Heart Fail 1(1):4–25
Nabeebaccus A, Zheng S, Shah AM (2016) Heart failure—potential new targets for therapy. Br Med Bull 119(1):99–110
Driscoll A, Meagher S, Kennedy R, Hay M, Banerji J, Campbell D, Cox N, Gascard D, Hare D, Page K, Nadurata V, Sanders R, Patsamanis H (2016) What is the impact of systems of care for heart failure on patients diagnosed with heart failure: a systematic review. BMC Cardiovasc Disord 16:195
A AO, Shah SJ (2015) Diagnosis and management of heart failure with preserved ejection frac-tion: 10 key lessons. Curr Cardiol Rev 11(1):42–52
Inamdar AA, Inamdar AC (2016) Heart failure: diagnosis, management and utilization. J Clin Med 5(7):62
Delp MD, Charvat JM, Limoli CL, Globus RK, Ghosh P (2016) Apollo lunar astronauts show higher cardiovascular disease mortality: possible deep space radiation effects on the vascular endothelium. Sci Rep 6:29901
Ade CJ et al (2017) Incidence rate of cardiovascular disease end points in the National Aeronautics and Space Administration Astronaut Corps. J Am Heart Assoc 6(8):e005564
Ross R (1986) The pathogenesis of atherosclerosis--an update. N Engl J Med 314(8):488–500
Tromp J, MacDonald MR, Tay WT, Teng THK, Hung CL, Narasimhan C, Shimizu W, Ling LH, Ng TP, Yap J, McMurray JJV, Zile MR, Richards AM, Anand IS, Lam CSP (2018) Heart failure with preserved ejection fraction in the young. Circulation 138(24):2763–2773
Halade GV, Kain V (2017) Obesity and cardiometabolic defects in heart failure pathology. Compr Physiol 7(4):1463–1477
Tourki B, Halade GV (2018) The failing of the obesity paradox in the failing heart. Am J Physiol Heart Circ Physiol 315:H1353–H1355
Westphal JG, Rigopoulos AG, Bakogiannis C, Ludwig SE, Mavrogeni S, Bigalke B, Doenst T, Pauschinger M, Tschöpe C, Schulze PC, Noutsias M (2017) The MOGE(S) classification for cardiomyopathies: current status and future outlook. Heart Fail Rev 22(6):743–752
Arbustini E, Narula N, Dec GW, Reddy KS, Greenberg B, Kushwaha S, Marwick T, Pinney S, Bellazzi R, Favalli V, Kramer C, Roberts R, Zoghbi WA, Bonow R, Tavazzi L, Fuster V, Narula J (2013) The MOGE(S) classification for a phenotype-genotype nomenclature of cardiomyopathy: endorsed by the World Heart Federation. J Am Coll Cardiol 62(22):2046–2072
Segovia Cubero J et al (2004) Heart failure: etiology and approach to diagnosis. Rev Esp Cardiol (English Edition) 57(03):250–259
Follath F (2001) Ischemic versus non-ischemic heart failure: should the etiology be determined? Heart Fail Monit 1(4):122–125
Van Linthout S, Tschöpe C (2017) Inflammation – cause or consequence of heart failure or both? Curr Heart Fail Rep 14(4):251–265
Westman PC, Lipinski MJ, Luger D, Waksman R, Bonow RO, Wu E, Epstein SE (2016) Inflammation as a driver of adverse left ventricular remodeling after acute myocardial infarction. J Am Coll Cardiol 67(17):2050–2060
Dick SA, Epelman S (2016) Chronic heart failure and inflammation: what do we really know? Circ Res 119(1):159–176
Yndestad A, Kristian Damås J, Øie E, Ueland T, Gullestad L, Aukrust P (2006) Systemic inflammation in heart failure--the whys and wherefores. Heart Fail Rev 11(1):83–92
Sansbury BE, Spite M (2016) Resolution of acute inflammation and the role of resolvins in immunity, thrombosis and vascular biology. Circ Res 119(1):113–130
Kain V, Prabhu SD, Halade GV (2014) Inflammation revisited: inflammation versus resolution of inflammation following myocardial infarction. Basic Res Cardiol 109(6):444
Hotamisligil GS (2017) Inflammation, metaflammation and immunometabolic disorders. Nature 542:177–185
Lopez EF, Kabarowski JH, Ingle KA, Kain V, Barnes S, Crossman DK, Lindsey ML, Halade GV (2015) Obesity superimposed on aging magnifies inflammation and delays the resolving response after myocardial infarction. Am J Physiol Heart Circ Physiol 308(4):H269–H280
Soehnlein O, Lindbom L (2010) Phagocyte partnership during the onset and resolution of inflammation. Nat Rev Immunol 10:427–439
Auffray C, Fogg D, Garfa M, Elain G, Join-Lambert O, Kayal S, Sarnacki S, Cumano A, Lauvau G, Geissmann F (2007) Monitoring of blood vessels and tissues by a population of monocytes with patrolling behavior. Science 317(5838):666–670
Kono H, Rock KL (2008) How dying cells alert the immune system to danger. Nat Rev Immunol 8(4):279–289
Maddox JF, Hachicha M, Takano T, Petasis NA, Fokin VV, Serhan CN (1997) Lipoxin A4 stable analogs are potent mimetics that stimulate human monocytes and THP-1 cells via a G-protein-linked lipoxin A4 receptor. J Biol Chem 272(11):6972–6978
Shih H et al (2010) The aging heart and post-infarction left ventricular remodeling. J Am Coll Cardiol 57(1):9–17
Woulfe KC, Bruns DR (2018) From pediatrics to geriatrics: mechanisms of heart failure across the life-course. J Mol Cell Cardiol 126:70–76
Halade GV, Kain V, Black LM, Prabhu SD, Ingle KA (2016) Aging dysregulates D- and E-series resolvins to modulate cardiosplenic and cardiorenal network following myocardial infarction. Aging 8(11):2611–2634
Dzau V, Braunwald E (1991) Resolved and unresolved issues in the prevention and treatment of coronary artery disease: a workshop consensus statement. Am Heart J 121(4 Pt 1):1244–1263
Halade GV, Kain V, Ingle KA (2018) Heart functional and structural compendium of cardiosplenic and cardiorenal networks in acute and chronic heart failure pathology. Am J Physiol Heart Circ Physiol 314(2):H255–h267
Halade GV et al (2018) Splenic leukocytes define the resolution of inflammation in heart failure. Sci Signal 11(520):eaao1818
Kain V, Ingle KA, Colas RA, Dalli J, Prabhu SD, Serhan CN, Joshi M, Halade GV (2015) Resolvin D1 activates the inflammation resolving response at splenic and ventricular site following myocardial infarction leading to improved ventricular function. J Mol Cell Cardiol 84:24–35
Halade GV, Kain V, Serhan CN (2018) Immune responsive resolvin D1 programs myocardial infarction-induced cardiorenal syndrome in heart failure. FASEB J 32(7):3717–3729
Jadapalli JK, Halade GV (2018) Unified nexus of macrophages and maresins in cardiac reparative mechanisms. FASEB J 32(10):5227–5237
Halade GV, Kain V, Tourki B, Jadapalli JK (2019) Lipoxygenase drives Lipidomic and metabolic reprogramming in ischemic heart failure. Metabolism 96:22–32
Kain V, Ingle KA, Kabarowski J, Barnes S, Limdi NA, Prabhu SD, Halade GV (2018) Genetic deletion of 12/15 lipoxygenase promotes effective resolution of inflammation following myocardial infarction. J Mol Cell Cardiol 118:70–80
Halade GV, Kain V, Ingle KA, Prabhu SD (2017) Interaction of 12/15-lipoxygenase with fatty acids alters the leukocyte kinetics leading to improved postmyocardial infarction healing. Am J Physiol Heart Circ Physiol 313(1):H89–h102
Neckar J et al (2019) Epoxyeicosatrienoic acid analog EET-B attenuates post-myocardial infarction remodeling in spontaneously hypertensive rats. Clin Sci (Lond) 133(8):939–951
Neckar J et al (2018) Infarct size-limiting effect of epoxyeicosatrienoic acid analog EET-B is mediated by hypoxia-inducible factor-1alpha via downregulation of prolyl hydroxylase 3. Am J Physiol Heart Circ Physiol 315(5):H1148–h1158
Brake R, Jones ID (2017) Chronic heart failure part 1: pathophysiology, signs and symptoms. Nurs Stand 31(19):54–63
Heymans S, Hirsch E, Anker SD, Aukrust P, Balligand JL, Cohen-Tervaert JW, Drexler H, Filippatos G, Felix SB, Gullestad L, Hilfiker-Kleiner D, Janssens S, Latini R, Neubauer G, Paulus WJ, Pieske B, Ponikowski P, Schroen B, Schultheiss HP, Tschöpe C, van Bilsen M, Zannad F, McMurray J, Shah AM (2009) Inflammation as a therapeutic target in heart failure? A scientific statement from the translational research Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 11(2):119–129
Frantz S, Bauersachs J, Ertl G (2009) Post-infarct remodelling: contribution of wound healing and inflammation. Cardiovasc Res 81(3):474–481
Altabas V (2015) Diabetes, endothelial dysfunction, and vascular repair: what should a diabetologist keep his eye on? Int J Endocrinol 2015:14
Burr, G.O. and M.M. Burr, Nutrition classics from The Journal of Biological Chemistry 82:345-67, 1929. A new deficiency disease produced by the rigid exclusion of fat from the diet. Nutr Rev, 1973 31(8): p. 248–249
Hu S et al (2018) Dietary fat, but not protein or carbohydrate, regulates energy intake and causes adiposity in mice. Cell Metab 28(3):415–431.e4
Kain V et al (2019) Obesogenic diet in aging mice disrupts gut microbe composition and alters neutrophil:lymphocyte ratio, leading to inflamed milieu in acute heart failure. Faseb j:fj201802477R
Kain V, Ingle KA, Kachman M, Baum H, Shanmugam G, Rajasekaran NS, Young ME, Halade GV (2018) Excess omega-6 fatty acids influx in aging drives metabolic dysregulation, electrocardiographic alterations, and low-grade chronic inflammation. Am J Physiol Heart Circ Physiol 314(2):H160–h169
Halade GV, el Jamali A, Williams PJ, Fajardo RJ, Fernandes G (2011) Obesity-mediated inflammatory microenvironment stimulates osteoclastogenesis and bone loss in mice. Exp Gerontol 46(1):43–52
Kain V, Halade GV (2017) Metabolic and biochemical stressors in diabetic cardiomyopathy. Front Cardiovasc Med 4:31
Nuttall FQ (2015) Body mass index: obesity, BMI, and health a critical review. Nutr Today 50(3):117–128
Lai M, Chandrasekera PC, Barnard ND (2014) You are what you eat, or are you? The challenges of translating high-fat-fed rodents to human obesity and diabetes. Nutr Diabetes 4(9):e135
Obesity and overweight. 2016 [Cited 2018; World Health Organization (WHO)]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 24 March 2019
International Diabetes Federation. 2012 [cited 2018; 5th Edition]. Available from: http://www.idf.org/diabetesatlas. Accessed 24 March 2019
DiNicolantonio JJ, O’Keefe JH (2017) Good fats versus bad fats: a comparison of fatty acids in the promotion of insulin resistance, inflammation, and obesity. Mo Med 114(4):303–307
Russo, L. and C.N. Lumeng, Properties and functions of adipose tissue macrophages in obesity. Immunology. 0(ja)
Dadvar S, Ferreira DMS, Cervenka I, Ruas JL (2018) The weight of nutrients: kynurenine metabolites in obesity and exercise. J Intern Med 284(5):519–533
Westerterp KR, Speakman JR (2008) Physical activity energy expenditure has not declined since the 1980s and matches energy expenditures of wild mammals. Int J Obes 32:1256–1263
Haslam DW, James WPT (2005) Obesity. Lancet 366(9492):1197–1209
Carvalheira JBC, Qiu Y, Chawla A (2013) Blood spotlight on leukocytes and obesity. Blood 122(19):3263–3267
Hower IM, Harper SA, Buford TW (2018) Circadian rhythms, exercise, and cardiovascular health. J Circadian Rhythms 16:7
Lavie CJ, Arena R, Swift DL, Johannsen NM, Sui X, Lee DC, Earnest CP, Church TS, O’Keefe JH, Milani RV, Blair SN (2015) Exercise and the cardiovascular system: clinical science and cardiovascular outcomes. Circ Res 117(2):207–219
O’Keefe JH, O’Keefe EL, Lavie CJ (2018) The Goldilocks Zone for exercise: not too little, Not Too Much. Mo Med 115(2):98–105
Díaz BB, González DA, Gannar F, Pérez MCR, de León AC (2018) Myokines, physical activity, insulin resistance and autoimmune diseases. Immunol Lett 203:1–5
Eijsvogels TMH, Thompson PD, Franklin BA (2018) The “extreme exercise hypothesis”: recent findings and cardiovascular health implications. Curr Treat Options Cardiovasc Med 20(10):84
Pedersen BK, Febbraio MA (2012) Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol 8:457–465
Lavie CJ, Johannsen N, Swift D, Sénéchal M, Earnest C, Church T, Hutber A, Sallis R, Blair SN (2014) Exercise is medicine – the importance of physical activity, exercise training, cardiorespiratory fitness and obesity in the prevention and treatment of type 2 diabetes. Eur Endocrinol 10(1):18–22
Fletcher GF, Landolfo C, Niebauer J, Ozemek C, Arena R, Lavie CJ (2018) Promoting physical activity and exercise: JACC health promotion series. J Am Coll Cardiol 72(14):1622–1639
Cattadori G et al (2017) Exercise and heart failure: an update. ESC Heart Fail 5(2):222–232
Brinker SK et al (2014) Association of cardiorespiratory fitness with left ventricular remodeling and diastolic function: the Cooper Center Longitudinal Study. JACC Heart Fail 2(3):238–246
León-Latre M et al (2014) Sedentary lifestyle and its relation to cardiovascular risk factors, insulin resistance and inflammatory profile. Rev Esp Cardiol (English Edition) 67(06):449–455
Morrison BN, McKinney J, Isserow S, Lithwick D, Taunton J, Nazzari H, de Souza AM, Heilbron B, Cater C, MacDonald M, Hives BA, Warburton DER (2018) Assessment of cardiovascular risk and preparticipation screening protocols in masters athletes: the Masters Athlete Screening Study (MASS): a cross-sectional study. BMJ Open Sport Exerc Med 4(1):e000370
Peake JM, Neubauer O, Walsh NP, Simpson RJ (2017) Recovery of the immune system after exercise. J Appl Physiol 122(5):1077–1087
Jamurtas AZ, Fatouros IG, Deli CK, Georgakouli K, Poulios A, Draganidis D, Papanikolaou K, Tsimeas P, Chatzinikolaou A, Avloniti A, Tsiokanos A, Koutedakis Y (2018) The effects of acute low-volume HIIT and aerobic exercise on leukocyte count and redox status. J Sports Sci Med 17(3):501–508
Young ME, Brewer RA, Peliciari-Garcia RA, Collins HE, He L, Birky TL, Peden BW, Thompson EG, Ammons BJ, Bray MS, Chatham JC, Wende AR, Yang Q, Chow CW, Martino TA, Gamble KL (2014) Cardiomyocyte-specific BMAL1 plays critical roles in metabolism, signaling, and maintenance of contractile function of the heart. J Biol Rhythm 29(4):257–276
Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH, Ivanova G, Omura C, Mo S, Vitaterna MH, Lopez JP, Philipson LH, Bradfield CA, Crosby SD, JeBailey L, Wang X, Takahashi JS, Bass J (2010) Disruption of the CLOCK components CLOCK and BMAL1 leads to hypoinsulinemia and diabetes. Nature 466(7306):627–631
Wang XS et al (2011) Shift work and chronic disease: the epidemiological evidence. Occup Med (Oxford, England) 61(2):78–89
Ingle KA, Kain V, Goel M, Prabhu SD, Young ME, Halade GV (2015) Cardiomyocyte-specific Bmal1 deletion in mice triggers diastolic dysfunction, extracellular matrix response, and impaired resolution of inflammation. Am J Physiol Heart Circ Physiol 309(11):H1827–H1836
Colas RA, Souza PR, Walker ME, Burton M, Zasłona Z, Curtis AM, Marques RM, Dalli J (2018) Impaired production and diurnal regulation of vascular RvDn-3 DPA increase systemic inflammation and cardiovascular disease. Circ Res 122(6):855–863
Scheer FAJL, Hilton MF, Mantzoros CS, Shea SA (2009) Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci U S A 106(11):4453–4458
Hermansson J, Hallqvist J, Karlsson B, Knutsson A, Gillander Gådin K (2018) Shift work, parental cardiovascular disease and myocardial infarction in males. Occup Med 68(2):120–125
Sato S, Sakurai T, Ogasawara J, Takahashi M, Izawa T, Imaizumi K, Taniguchi N, Ohno H, Kizaki T (2014) A circadian Clock gene, Rev-erbα, modulates the inflammatory function of macrophages through the negative regulation of <em>Ccl2</em> expression. J Immunol 192(1):407–417
Scheiermann C, Kunisaki Y, Frenette PS (2013) Circadian control of the immune system. Nat Rev Immunol 13:190–198
Turek FW et al (2005) Obesity and Metabolic Syndrome in Circadian Clock Mutant Mice. Science (New York, N.Y.) 308(5724):1043–1045
Abu Farha R (2018) And E. Alefishat, Shift work and the risk of cardiovascular diseases and metabolic syndrome among Jordanian employees. Oman Med J 33(3):235–242
Poggiogalle E, Jamshed H, Peterson CM (2018) Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 84:11–27
Wirtz PH, von Känel R (2017) Psychological stress, inflammation, and coronary heart disease. Curr Cardiol Rep 19(11):111
(CSHS), C.f.S.o.H.S. Acute vs Chronic Stress. 2017 [05/17/2019]; Available from: https://humanstress.ca/stress/understand-your-stress/acute-vs-chronic-stress/. Accessed 24 March 2019
Lagraauw HM, Kuiper J, Bot I (2015) Acute and chronic psychological stress as risk factors for cardiovascular disease: insights gained from epidemiological, clinical and experimental studies. Brain Behav Immun 50:18–30
Dimsdale JE (2008) Psychological stress and cardiovascular disease. J Am Coll Cardiol 51(13):1237–1246
Slopen N, Glynn RJ, Buring JE, Lewis TT, Williams DR, Albert MA (2012) Job strain, job insecurity, and incident cardiovascular disease in the Women’s Health Study: results from a 10-year prospective study. PLoS One 7(7):e40512–e40512
Kivimäki M, Kawachi I (2015) Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep 17(9):630–630
Cohen BE, Edmondson D, Kronish IM (2015) State of the art review: depression, stress, anxiety, and cardiovascular disease. Am J Hypertens 28(11):1295–1302
Zhang L, Piña IL (2019) Stress-induced cardiomyopathy. Heart Fail Clin 15(1):41–53
Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA, Seifert B, Hellermann J, Schwyzer M, Eisenhardt K, Jenewein J, Franke J, Katus HA, Burgdorf C, Schunkert H, Moeller C, Thiele H, Bauersachs J, Tschöpe C, Schultheiss HP, Laney CA, Rajan L, Michels G, Pfister R, Ukena C, Böhm M, Erbel R, Cuneo A, Kuck KH, Jacobshagen C, Hasenfuss G, Karakas M, Koenig W, Rottbauer W, Said SM, Braun-Dullaeus RC, Cuculi F, Banning A, Fischer TA, Vasankari T, Airaksinen KEJ, Fijalkowski M, Rynkiewicz A, Pawlak M, Opolski G, Dworakowski R, MacCarthy P, Kaiser C, Osswald S, Galiuto L, Crea F, Dichtl W, Franz WM, Empen K, Felix SB, Delmas C, Lairez O, Erne P, Bax JJ, Ford I, Ruschitzka F, Prasad A, Lüscher TF (2015) Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. N Engl J Med 373(10):929–938
Fullerton JN, Gilroy DW (2016) Resolution of inflammation: a new therapeutic frontier. Nat Rev Drug Discov 15(8):551–567
Heinz J, Marinello M, Fredman G (2017) Pro-resolution therapeutics for cardiovascular diseases. Prostaglandins Other Lipid Mediat 132:12–16
Serhan CN (2014) Pro-resolving lipid mediators are leads for resolution physiology. Nature 510(7503):92–101
Serhan CN, Brain SD, Buckley CD, Gilroy DW, Haslett C, O’Neill LAJ, Perretti M, Rossi AG, Wallace JL (2007) Resolution of inflammation: state of the art, definitions and terms. FASEB J 21(2):325–332
Serhan CN (2017) Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms. FASEB J 31(4):1273–1288
Serhan CN, Chiang N, Van Dyke TE (2008) Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol 8(5):349–361
Bronzato S, Durante A (2018) Dietary supplements and cardiovascular diseases. Int J Prev Med 9:80–80
Goel A, Pothineni N, Singhal M, Paydak H, Saldeen T, Mehta J (2018) Fish, fish oils and cardioprotection: promise or fish tale? Int J Mol Sci 19(12):3703
Halade GV, Williams PJ, Lindsey ML, Fernandes G (2011) Fish oil decreases inflammation and reduces cardiac remodeling in rosiglitazone treated aging mice. Pharmacol Res 63(4):300–307
Kain V, Halade GV (2019) Immune responsive resolvin D1 programs peritoneal macrophages and cardiac fibroblast phenotypes in diversified metabolic microenvironment. J Cell Physiol 234(4):3910–3920
Aggarwal M, Bozkurt B, Panjrath G, Aggarwal B, Ostfeld RJ, Barnard ND, Gaggin H, Freeman AM, Allen K, Madan S, Massera D, Litwin SE, American College of Cardiology’s Nutrition and Lifestyle Committee of the Prevention of Cardiovascular Disease Council (2018) Lifestyle modifications for preventing and treating heart failure. J Am Coll Cardiol 72(19):2391–2405
Salive ME (2013) Multimorbidity in older adults. Epidemiol Rev 35:75–83
Forman DE, Maurer MS, Boyd C, Brindis R, Salive ME, Horne FMF, Bell SP, Fulmer T, Reuben DB, Zieman S, Rich MW (2018) Multimorbidity in older adults with cardiovascular disease. J Am Coll Cardiol 71(19):2149–2161
Leelakanok N et al (2017) Association between polypharmacy and death: a systematic review and meta-analysis. J Am Pharm Assoc (2003) 57(6):729–738.e10
Arfè A et al (2016) Non-steroidal anti-inflammatory drugs and risk of heart failure in four European countries: nested case-control study. BMJ 354
Huang SP et al (2018) Nonsteroidal anti-inflammatory drugs and risk of first hospitalization for heart failure in patients with no history of heart failure: a population-based case-crossover study. Drug Saf
Rotunno R et al (2018) NSAIDs and heart failure: a dangerous relationship. Monaldi Arch Chest Dis 88(2):950
Halade GV, Kain V, Wright GM, Jadapalli JK (2018) Subacute treatment of carprofen facilitate splenocardiac resolution deficit in cardiac injury. J Leukoc Biol 104:1173–1186
Ridker PM, Everett BM, Thuren T, MacFadyen J, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ, CANTOS Trial Group (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med 377(12):1119–1131
McNeil JJ et al (2018) Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 379(16):1509–1518
Dong J, Chen H (2018) Cardiotoxicity of anticancer therapeutics. Front Cardiovasc Med 5:9
Jadapalli JK et al (2018) Doxorubicin triggers splenic contraction and irreversible dysregulation of COX and LOX that alters inflammation-resolution program in the myocardium. Am J Physiol Heart Circ Physiol
Linhart A, Belohlavek J Type 2 diabetes mellitus and heart failure. Vnitr Lek 62(7–8):592–597
Waksman J, Taylor RN Jr, Bodor GS, Daly FFS, Jolliff HA, Dart RC (2001) Acute myocardial infarction associated with amphetamine use. Mayo Clin Proc 76(3):323–326
Smedra A, Szustowski S, Berent J (2015) Amphetamine-related myocardial infarction in a 42-year old man. Arch Med Sadowej Kryminol 65(3):173–181
Valgimigli, M. 2018. The remarkable story of a wonder drug, which now comes to an end in the primary prevention setting: say bye-bye to aspirin!. Eur Heart J
McNeil, J.J., et al. 2018. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med
Funding
This work was supported by National Institutes of Health (AT006704 and HL132989) and The University of Alabama at Birmingham (UAB) Pittman scholar award to G.V.H.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pullen, A.B., Jadapalli, J.K., Rhourri-Frih, B. et al. Re-evaluating the causes and consequences of non-resolving inflammation in chronic cardiovascular disease. Heart Fail Rev 25, 381–391 (2020). https://doi.org/10.1007/s10741-019-09817-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-019-09817-x