Abstract
The human immunodeficiency virus (HIV) has altered the epidemiology, clinical manifestations, treatment considerations and natural history of tuberculous (TB) pericarditis with significant implications for clinicians. The caseload of TB pericarditis has risen sharply in TB endemic areas of the world where co-infection with HIV is common. Furthermore, TB is the cause in greater than 85 % of cases of pericardial effusion in HIV-infected cohorts. In the absence of HIV, the morbidity of TB pericarditis is primarily related to the ferocity of the immune response to TB antigens within the pericardium. In patients with HIV, because TB pericarditis more often occurs as part of a disseminated process, the infection itself has a greater impact on the morbidity and mortality. HIV-associated TB pericarditis is a more aggressive disease with a greater degree of myocardial involvement. Patients have larger pericardial effusions with more frequent hemodynamic compromise and more significant ST segment changes in the electrocardiogram. HIV alters the natural history and outcomes of TB pericarditis. Immunocompromised participants appear less likely to develop constrictive pericarditis and have a significantly higher mortality compared with their immunocompetent counterparts. Finally co-infection with HIV has resulted in a number of areas of uncertainty. The mechanisms of myocardial dysfunction are unclear, new methods of improving the yield of TB culture and establishing a rapid bacterial diagnosis remain a major challenge, the optimal duration of anti-TB therapy has yet to be established, and the role of corticosteroids has yet to be resolved.
Similar content being viewed by others
Introduction
Tuberculous (TB) pericarditis has a caseload of approximately 80,000–160,000 per year and is the most common cause of pericarditis in Africa and other regions of the world where Mycobacterium tuberculosis (Mtb) is endemic. In a large single-center study from South Africa, 69.5 % of patients undergoing pericardiocentesis were found to have TB and over 50 % of the participants were infected with the human immunodeficiency virus (HIV) [1]. By contrast, TB accounts for only 4 % of cases in developed countries [2] where immigrants from TB endemic areas and people with HIV are at highest risk [3].
There have been numerous well-written manuscripts, reviews and chapters devoted to TB pericarditis. However, most do not make more than a passing reference to the impact of HIV. The emergence of HIV in sub-Saharan Africa in the 1990s and its current state as a global pandemic has altered the epidemiology, clinical manifestations, treatment considerations and natural history of TB pericarditis with significant implications for clinicians. This chapter will review TB pericarditis, emphasizing areas where there are significant differences between the disease in HIV-infected and uninfected hosts and areas where HIV has created uncertainty.
Epidemiology of TB pericarditis and the impact of HIV
Autopsy studies conducted before the advent of HIV suggest that the pericardium is involved in 1 % of patients with TB [4]. By contrast, autopsy data from patients who died with advanced HIV reveal that extra-pulmonary disease with multi-organ involvement is frequent [5, 6]. In HIV-infected cohorts with a pericardial effusion, TB is the cause in greater than 85 % of cases [7]. Furthermore, the incidence and caseload of TB pericarditis has risen sharply in TB endemic areas of the world where co-infection with HIV is common [8–10]. This is explained in part by the fact that the lifetime risk of TB in hosts with a competent immune system is 10 % [11], which rises to an annual risk of 10 % early following infection with HIV and is as high 30 % annual risk in those with advanced immunosuppression [12].
The immune response and pathogenesis of tuberculous pericarditis in patients with and without HIV
Tuberculosis spreads to the pericardium via three main mechanisms. It can spread retrograde from mediastinal, peritracheal and peribronchial lymph nodes, via the hematogenous route during primary tuberculosis and by direct spread from lung parenchyma or pleural involvement [13, 14]. In immune-competent hosts, this spread is predominantly via lymph nodes, whereas HIV-related immune suppression is associated with more hematogenous spread [15].
Among HIV-uninfected hosts, TB pericarditis is frequently a paucibacillary condition in which the morbidity is related to the ferocity of the immune response it evokes and not to the virulence of the pathogen itself [2, 13, 16]. In patients with HIV, on the other hand, because extra-pulmonary TB such as pericarditis occurs more frequently as part of a disseminated process associated with TB bacteremia, the infection itself may have a greater impact on the morbidity and mortal outcomes [11, 17]. Once in the pericardium, viable mycobacterial protein antigens presented by macrophages to CD4+ T lymphocytes trigger activation of lymphocytes, macrophages and complement-fixing antibodies. This leads to pericardial inflammation, granuloma formation, cytolysis and the production of a fibrinous exudate rich with inflammatory cytokines [16, 18–20]. HIV interferes with almost all of these critical cellular processes [17] as evidenced by findings of a relative CD4+ T-cell depletion and diminished granuloma formation systemically and within the pericardium [20, 21]. Furthermore, there is evidence that HIV alters the phenotype and function of CD4+ memory T cells within the pericardium [22]. These important differences may contribute to both the increased risk of developing TB pericarditis and the altered clinical manifestations in HIV.
The clinical manifestations of TB pericarditis and the impact of HIV
There are four recognized stages of TB pericarditis and two general modes of clinical presentation (Table 1). The stages include: a dry stage, an effusive stage, an adsorptive phase and a constrictive phase [13, 14, 23]. In the first mode of presentation, pericardial involvement is asymptomatic and is an incidental finding in patients who have evidence of active tuberculosis elsewhere in the body [14]. Evidence for this stems from autopsy findings, which suggest that the pericardium is involved in 1–2 % of HIV-uninfected patients known to have pulmonary TB [4]. Among HIV-infected patients, the proportion of asymptomatic involvement of the pericardium may be much higher. Both autopsy and observational studies show that HIV is associated with a higher prevalence of widespread, multi-site, extra-pulmonary TB [6, 24, 25]. Among such patients, often the dominant symptoms are those of sepsis and TB, while presumably the pericardial and other specific site involvement is clinically silent [17].
In the second mode of presentation, inflammation and compression from inflammatory fluid, the diseased pericardium itself, or both, cause the typical constellation of symptoms that are associated with pericardial effusion and constrictive pericarditis [14, 15, 26, 27]. Patients can present for the first time with any one of these stages [23]. HIV may alter both the clinical manifestation of these recognized syndromes and the progression through the various stages [7, 28].
The dry stage of TB pericarditis presents clinically with the syndrome of acute pericarditis without effusion and is least common [2]. Symptomatic effusive TB pericarditis presents clinically with evidence of cardiac compression manifest as either heart failure or tamponade [29]. It can also present as effusive constrictive pericarditis, a syndrome first described by Hancock in the 1970s, which is characterized by the simultaneous occurrence of compressive pericardial fluid and visceral pericardial constriction [30, 31].
The adsorptive phase of TB pericarditis presents in a manner very similar to constrictive pericarditis; however, there is radiological and imaging evidence of persistent thick fibrinous fluid surrounding the heart [13, 26]. Differentiating effusive constrictive pericarditis and adsorptive fibrinous pericarditis can be difficult. The important difference is the initial presenting clinical picture. In the former, compressive hemodynamics attributable to fluid around the heart dominate the clinical picture, and only after relief of the compression does the physiology resemble that of constrictive pericarditis [32]. In the latter stage, despite the presence of residual inflammatory fluid, the clinical and hemodynamic presentation is consistent with constrictive pericarditis from the onset [13, 23].
In the constrictive phase of TB pericarditis, there is no residual pericardial fluid. Post-inflammatory scarring, thickening, fibrosis and calcification result in progressive loss of pericardial elasticity and compliance and impaired cardiac filling. Progressive fluid retention and symptoms of heart failure in the absence of pulmonary congestion are typical [26, 33]. Constrictive pericarditis is one of the most serious sequelae of TB pericarditis and is the outcome in between 17 and 60 % of patients despite appropriate anti-tuberculous therapy [2]. Perimyocarditis and other forms of myocardial involvement in patients with TB pericarditis are distinctly unusual in patients in the absence of HIV [15]. One exception is patients with constrictive pericarditis where a small but significant proportion of patients may have evidence of depressed myocardial function, which is the result of a complex array of mechanisms [33, 34].
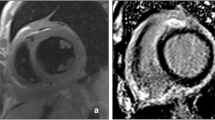
The Investigation of the Management of Africa (IMPI Africa) registry is the largest and only multicenter prospective study of patients with suspected TB pericarditis in African countries with a high prevalence with HIV [31]. Just fewer than 95 % of the 185 participants presented with effusive TB pericarditis, and 40 % had clinical signs of advanced immune suppression. The registry data showed that HIV-associated TB pericarditis may be a more aggressive disease with a greater degree of myocardial involvement resulting in much sicker patients at first presentation [35]. There was radiological and echocardiographic evidence of larger pericardial effusions with more frequent hemodynamic compromise, and more significant ST segment changes in the electrocardiogram [35].
Figures 1 and 2 provide examples of a CXR and echocardiograph, respectively, from an HIV-infected patient with a large tuberculous pericardial effusion.
These registry results corroborated findings from a retrospective review of case records from West Africa, in which the prevalence of myocardial dysfunction in patients with TB pericarditis was as high as 40 % [36]. The mechanism of depressed left ventricular (LV) function in HIV-associated TB pericarditis is likely to be multi-factorial. Contending possibilities include but are not limited to: perimyocarditis with significant myocardial injury [37, 38], cytokine-induced myocardial dysfunction related to TB bacteremia and dissemination [39], and possibly pre-existing HIV-associated cardiomyopathy [40].
HIV may also alter progression through the various stages of TB pericarditis. In a further analysis of data from the IMPI registry, participants with clinical and/or serological evidence of HIV were less likely to develop clinical evidence of constrictive pericarditis at 6 months of follow-up compared with their immunocompetent counterparts [28]. This observation has been noted previously [34], but needs to be corroborated with more robust evidence from larger well-designed studies.
Finally, HIV is an important determinant of mortality in patients with TB pericarditis. In the IMPI registry, immunocompromised patients had a 6-month mortality rate of 40 % compared with 17 % in those without [35]. This is consistent with the impact of HIV on TB-related mortality across the spectrum of TB-related disease [17]. However, it is important to note that only a small minority of patients in this registry were on antiretroviral therapy (ART). Early aggressive immune functional restoration may have had a significant positive difference in mortality [41].
Diagnostic considerations in patients with and without HIV
The definitive diagnosis of a tuberculous etiology in patients with pericarditis rests on demonstrating the presence of tubercle bacilli in stained smear or culture of pericardial fluid or caseating granulomata on pericardial histology [2]. The yield of these direct methods ranges from 0 to 75 %, which has led to the use of more indirect methods. These include looking for microbiological evidence of TB elsewhere in the body and the use biomarkers like adenosine deaminase (ADA) in patients with an inflammatory pericardial exudate [2, 42]. DNA-based techniques such as polymerase chain reaction (PCR) have proved to be very disappointing. The sensitivity is well below 30 % and is particularly poor where pericardial tissue is not available, as is most often the case [15, 43].
The presence of HIV infection may alter the diagnostic yield of these direct methods. Microbiological confirmation of the diagnosis of TB in several studies of TB pericarditis conducted in presumed HIV-seronegative cohorts [44, 45] was much higher than it has been in studies of participants with known HIV [46, 47]. Furthermore, granuloma formation within the pericardium is poor in patients with HIV [21] and the yield from TB culture is much lower in HIV-infected patients in general [48]. Despite this, the diagnostic yield from indirect methods such as ADA appears to be unaffected by HIV. In one study from South Africa, the positive and negative predictive value of these indirect tests was not diminished by HIV status [43].
Given that TB is the cause of pericarditis in the overwhelming majority of participants with HIV, the question of whether there is a need to conduct any diagnostic testing at all often arises. A major reason to pursue a thorough diagnostic workup is that treatable alternative causes of pericarditis such as purulent pericarditis, malignancy and uremia are well described in patients with HIV [43, 49] and need to be actively excluded because these alternative diagnoses carry a much higher mortality than TB pericarditis. Empiric treatment for TB alone for such patients has morbid implications and is associated with worse outcomes [35].
Treatment considerations
Prior to the introduction of effective chemotherapy for TB pericarditis, confirmation of the diagnosis was a virtual death sentence with mortality rates as high as 90 % [50] (Fig. 3). Modern anti-tuberculosis regimens with a rifampicin and isoniazid backbone have decreased mortality dramatically. In HIV-uninfected patients mortality rates dropped to 8–17 % [2], whereas in HIV-infected patients this rate is higher at 17–40 % [2, 35]. The mainstay of therapy remains the 6-month short course used for HIV-uninfected hosts despite the lack of randomized evidence to support an optimal duration of treatment for TB pericarditis in HIV-infected patients [17, 42, 51].
While there is no specific data for patients with TB pericarditis, extra-pulmonary TB is now regarded as an absolute indication of the introduction of anti-retroviral therapy (ART) regardless of CD4 count [17]. Concern about the potential for the development of toxicities, side effects, the immune reconstitution syndrome (IRIS) and complex drug–drug interactions if ART is introduced early during therapy for TB often led to long delays [7, 17]. Based on available evidence, it is now considered reasonable to defer treatment with ART until after completion of anti-TB therapy in those with CD4 cell count >350 cells/μl, to commence after 2 months in patients with cell counts between 100 and 350 cells/μl and to commence immediately where there is evidence of advanced CD 4 cell depletion [17, 52].
The role of corticosteroids in the management of TB pericarditis in both HIV-infected and uninfected hosts remains unresolved [53]. Several randomized controlled trials in both HIV-uninfected [44, 45] and HIV-infected cohorts [46] have attempted to address the question of the efficacy of adjuvant steroids in TB pericarditis. All the trials were limited by problems related to methodology, design and small numbers. A systematic review suggests that while there is no benefit on the important hard endpoints of mortality and constriction, there may be faster resolution of symptoms and there is no evidence of harm [53]. A possible explanation for the absence of the anticipated benefit of corticosteroids in these trials is that the cytochrome P-450 enzyme-inducing effect of Rifampicin and its impact on the bioavailability of corticosteroids was not considered in the relatively low doses used in the trials [54]. The efficacy of corticosteroids in TB pericarditis is currently the subject of an ongoing randomized controlled trial (clinicaltrials.gov/ct2/show/NCT00810849).
Areas of uncertainty and future considerations
Despite the global magnitude of the problem of HIV-associated TB pericarditis, there are a number of areas of uncertainty. The difficulty in establishing a rapid bacteriologic or histologic diagnosis; the optimal therapeutic strategy with regard to duration of anti-TB therapy; use of corticosteroids and role of invasive interventions such as pericardiocentesis, pericardial windows and/or pericardiectomy have all not been adequately explored. Furthermore, the frequency pathogenesis and impact on survival of left ventricular dysfunction remains a mystery.
Summary and conclusions
TB pericarditis is a serious extra-pulmonary manifestation of TB that has increased in frequency due to the HIV pandemic. HIV-associated TB pericarditis appears to be a more aggressive disease, which is harder to diagnose, and is more often associated with dissemination of TB, larger effusions, myocardial involvement and a higher mortality rate. Major gaps in knowledge about the disease remain, which need to be addressed through well-designed prospective studies.
References
Reuter H, Burgess LJ, Doubell AF (2005) Epidemiology of pericardial effusions at a large academic hospital in South Africa. Epidemiol Infect 133(3):393–399
Mayosi BM, Burgess LJ, Doubell AF (2005) Tuberculous pericarditis. Circulation 112(23):3608–3616
Imazio M, Brucato A, Maestroni S, Cumetti D, Belli R, Trinchero R, Adler Y (2011) Risk of constrictive pericarditis after acute pericarditis. Circulation 124(11):1270–1275
Fowler NO (1991) Tuberculous pericarditis. JAMA 266:99–103
Lucas SB, Hounnou A, Peacock C, Beaumel A, Djomand G, N’Gbichi JM, Yeboue K, Honde M, Diomande M, Giordano C et al (1993) The mortality and pathology of HIV infection in a west African city. AIDS 7(12):1569–1579
Rana F, Hawken MP, Meme HK, Chakaya JM, Githui WA, Odhiambo JA, Porter JD, McAdam KP, Lucas SJ (1997) Autopsy findings in HIV-1-infected adults in Kenya. J Acquir Immune Defic Syndr Hum Retrovirol 14(1):83–85
Ntsekhe M, Hakim J (2005) Impact of human immunodeficiency virus infection on cardiovascular disease in Africa. Circulation 112(23):3602–3607
Maher D, Harries AD (1997) Tuberculous pericardial effusion: a prospective clinical study in a low-resource setting–Blantyre, Malawi. Int J Tuberc Lung Dis 1(4):358–364
Cegielski JP, Lwakatare J, Dukes CS, Lema LE, Lallinger GJ, Kitinya J, Reller LB, Sheriff F (1994) Tuberculous pericarditis in Tanzanian patients with and without HIV infection. Tuber Lung Dis 75(6):429–434
Cegielski JP, Ramiya K, Lallinger GJ, Mtulia IA, Mbaga IM (1990) Pericardial disease and human immunodeficiency virus in Dar es Salaam, Tanzania. Lancet 335(8683):209–212
Lawn SD, Zumla AI (2011) Tuberculosis. Lancet 378(9785):57–72
Maartens G, Wilkinson RJ (2007) Tuberculosis. Lancet 370(9604):2030–2043
Heimann HL, Binder S (1940) Tuberculous pericarditis. Br Heart J 2(3):165–176
Peel AA (1948) Tuberculous pericarditis. Br Heart J 10(3):195–207
Syed FF, Mayosi BM (2007) A modern approach to tuberculous pericarditis. Prog Cardiovasc Dis 50(3):218–236
Commerford PJ, Strang JIG (1991) Tuberculous pericarditis. In: Coovadia HM, Benatar SR (eds) A century of tuberculosis. South African perspectives, vol 1, 1st edn. Oxford University Press, Capetown, pp 123–137
Schutz C, Meintjes G, Almajid F, Wilkinson RJ, Pozniak A (2010) Clinical management of tuberculosis and HIV-1 co-infection. Eur Respir J 36(6):1460–1481
Maisch B, Maisch S, Kochsiek K (1982) Immune reactions in tuberculous and chronic constrictive pericarditis. Clinical data and diagnostic significance of antimyocardial antibodies. Am J Cardiol 50(5):1007–1013
Dannenberg AM Jr (1991) Delayed-type hypersensitivity and cell-mediated immunity in the pathogenesis of tuberculosis. Immunol Today 12(7):228–233
Reuter H, Burgess LJ, Carstens ME, Doubell AF (2006) Characterization of the immunological features of tuberculous pericardial effusions in HIV positive and HIV negative patients in contrast with non-tuberculous effusions. Tuberculosis (Edinb) 86(2):125–133
Reuter H, Burgess LJ, Schneider J, Van Vuuren W, Doubell AF (2006) The role of histopathology in establishing the diagnosis of tuberculous pericardial effusions in the presence of HIV. Histopathology 48(3):295–302
Matthews K, Ntsekhe M, Syed F, Scriba T, Russell J, Tibazarwa K, Deffur A, Hanekom W, Mayosi BM, Wilkinson RJ, Wilkinson KA (2012) HIV-1 infection alters CD4+ memory T-cell phenotype at the site of disease in extrapulmonary tuberculosis. Eur J Immunol 42(1):147–157
Kreinin S (1960) Tuberculous pericarditis observed from the stage of effusion to pericardial calcification. Am Rev Respir Dis 81:585–587
Pozniak AL, Weinberg J, Mahari M, Neill P, Houston S, Latif A (1994) Tuberculous pericardial effusion associated with HIV infection: a sign of disseminated disease. Tuber Lung Dis 75(4):297–300
Shafer RW, Kim DS, Weiss JP, Quale JM (1991) Extrapulmonary tuberculosis in patients with human immunodeficiency virus infection. Medicine (Baltimore) 70(6):384–397
Myers RB, Spodick DH (1999) Constrictive pericarditis: clinical and pathophysiologic characteristics. Am Heart J 138(2 Pt 1):219–232
Little WC, Freeman GL (2006) Pericardial disease. Circulation 113(12):1622–1632
Ntsekhe M, Wiysonge CS, Gumedze F, Maartens G, Commerford PJ, Volmink JA, Mayosi BM (2008) HIV infection is associated with a lower incidence of constriction in presumed tuberculous pericarditis: a prospective observational study. PLoS ONE 3(6):e2253
Strang JI (1984) Tuberculous pericarditis in Transkei. Clin Cardiol 7:667–670
Hancock EW (1971) Subacute effusive-constrictive pericarditis. Circulation 43(2):183–192
Mayosi BM, Wiysonge CS, Ntsekhe M, Volmink JA, Gumedze F, Maartens G, Aje A, Thomas BM, Thomas KM, Awotedu AA, Thembela B, Mntla P, Maritz F, Ngu Blackett K, Nkouonlack DC, Burch VC, Rebe K, Parish A, Sliwa K, Vezi BZ, Alam N, Brown BG, Gould T, Visser T, Shey MS, Magula NP, Commerford PJ (2006) Clinical characteristics and initial management of patients with tuberculous pericarditis in the HIV era: the Investigation of the Management of Pericarditis in Africa (IMPI Africa) registry. BMC Infect Dis 6:2
Hancock EW (2004) A clearer view of effusive-constrictive pericarditis. N Engl J Med 350(5):435–437
Evans W, Jackson F (1952) Constrictive pericarditis. Br Heart J 14(1):53–59
Cinar B, Enc Y, Goksel O, Cimen S, Ketenci B, Teskin O, Kutlu H, Eren E (2006) Chronic constrictive tuberculous pericarditis: risk factors and outcome of pericardiectomy. Int J Tuberc Lung Dis 10(6):701–706
Mayosi BM, Wiysonge CS, Ntsekhe M, Gumedze F, Volmink JA, Maartens G, Aje A, Thomas BM, Thomas KM, Awotedu AA, Thembela B, Mntla P, Maritz F, Blackett KN, Nkouonlack DC, Burch VC, Rebe K, Parrish A, Sliwa K, Vezi BZ, Alam N, Brown BG, Gould T, Visser T, Magula NP, Commerford PJ (2008) Mortality in patients treated for tuberculous pericarditis in sub-Saharan Africa. S Afr Med J 98(1):36–40
Niakara A, Kambire Y, Drabo YJ (2001) Pericarditis in HIV infected patients: retrospective study of 40 cases in Ouagadougou, Burkina Faso. Sante 11(3):167–172
Teraoka K, Hirano M, Yannbe M, Ohtaki Y, Ohkubo T, Abe K, Yamashina A (2005) Delayed contrast enhancement in a patient with perimyocarditis on contrast-enhanced cardiac MRI: case report. Int J Cardiovasc Imaging 21(2–3):325–329
Roubille F, Gahide G, Granier M, Cornillet L, Vernhet-Kovacsik H, Moore-Morris T, Macia JC, Piot C (2008) Likely tuberculous myocarditis mimicking an acute coronary syndrome. Intern Med 47(19):1699–1701
Merx MW, Weber C (2007) Sepsis and the heart. Circulation 116(7):793–802
Ntsekhe M, Mayosi BM (2009) Cardiac manifestations of HIV infection: an African perspective. Nat Clin Pract Cardiovasc Med 6(2):120–127
Lawn SD, Harries AD (2011) Reducing tuberculosis-associated early mortality in antiretroviral treatment programmes in sub-Saharan Africa. AIDS 25(12):1554–1555; author reply 1556
Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH (2004) Guidelines on the diagnosis and management of pericardial diseases executive summary; the task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J 25(7):587–610
Reuter H, Burgess L, van Vuuren W, Doubell A (2006) Diagnosing tuberculous pericarditis. QJM 99(1460-2725 (Print) VI-99 IP-12 DP-2006 Dec):827–39
Strang JI, Kakaza HH, Gibson DG, Allen BW, Mitchison DA, Evans DJ, Girling DJ, Nunn AJ, Fox W (1988) Controlled clinical trial of complete open surgical drainage and of prednisolone in treatment of tuberculous pericardial effusion in Transkei. Lancet 2(8614):759–766
Strang JI, Kakaza HH, Gibson DG, Girling DJ, Nunn AJ, Fox W (1987) Controlled trial of prednisolone as adjuvant in treatment of tuberculous constrictive pericarditis in Transkei. Lancet 2(8573):1418–1422
Hakim JG, Ternouth I, Mushangi E, Siziya S, Robertson V, Malin A (2000) Double blind randomised placebo controlled trial of adjunctive prednisolone in the treatment of effusive tuberculous pericarditis in HIV seropositive patients. Heart 84(2):183–188. doi:10.1136/heart.84.2.183
Reuter H, Burgess LJ, Louw VJ, Doubell AF (2007) The management of tuberculous pericardial effusion: experience in 233 consecutive patients. Cardiovasc J S Afr 18(1):20–25
Wallis RS, Pai M, Menzies D, Doherty TM, Walzl G, Perkins MD, Zumla A (2010) Biomarkers and diagnostics for tuberculosis: progress, needs, and translation into practice. Lancet 375(9729):1920–1937
Louw A, Tikly M (2007) Purulent pericarditis due to co-infection with Streptococcus pneumoniae and Mycobacterium tuberculosis in a patient with features of advanced HIV infection. BMC Infect Dis 7:12
Harvey AM, Whitehill MR (1937) Tuberculous pericarditis. Medicine 16:45–94
Maher D, Uplekar M, Blanc L, Raviglione M (2003) Treatment of tuberculosis. BMJ 327(7419):822–823
Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray A, Gengiah T, Nair G, Bamber S, Singh A, Khan M, Pienaar J, El-Sadr W, Friedland G, Abdool Karim Q (2010) Timing of initiation of antiretroviral drugs during tuberculosis therapy. N Engl J Med 362(8):697–706
Ntsekhe M, Wiysonge C, Volmink JA, Commerford PJ, Mayosi BM (2003) Adjuvant corticosteroids for tuberculous pericarditis: promising, but not proven. QJM 96(8):593–599
Baciewicz AM, Chrisman CR, Finch CK, Self TH (2008) Update on rifampin and rifabutin drug interactions. Am J Med Sci 335(2):126–136
Acknowledgments
The authors would like to acknowledge the Investigation of the Management of PericarditIs (IMPI) in Africa team for their hard work and contributions to our current understanding of TB pericarditis and the impact of HIV.
Conflict of interest
Drs Bongani M Mayosi and Mpiko Ntsekhe have no conflict of interest, relation with industry or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ntsekhe, M., Mayosi, B.M. Tuberculous pericarditis with and without HIV. Heart Fail Rev 18, 367–373 (2013). https://doi.org/10.1007/s10741-012-9310-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-012-9310-6