Abstract
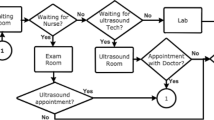
This paper presents an analysis of a residency primary care clinic whose majority of patients are underserved. The clinic is operated by the health system for Bexar County and staffed primarily with physicians in a three-year Family Medicine residency program at The University of Texas School of Medicine in San Antonio. The objective of the study was to obtain a better understanding of patient flow through the clinic and to investigate changes to current scheduling rules and operating procedures. Discrete event simulation was used to establish a baseline and to evaluate a variety of scenarios associated with appointment scheduling and managing early and late arrivals. The first steps in developing the model were to map the administrative and diagnostic processes and to collect time-stamped data and fit probability distributions to each. In conjunction with the initialization and validation steps, various regressions were performed to determine if any relationships existed between individual providers and patient types, length of stay, and the difference between discharge time and appointment time. The latter two statistics along with resource utilization and closing time were the primary metrics used to evaluate system performance.
The results showed that up to an 8.5 % reduction in patient length of stay is achievable without noticeably affecting the other metrics by carefully adjusting appointment times. Reducing the no-show rate from its current value of 21.8 % or overbooking, however, is likely to overwhelm the system’s resources and lead to excessive congestion and overtime. Another major finding was that the providers are the limiting factor in improving patient flow. With an average utilization rate above 90 % there is little prospect in shortening the total patient time in the clinic without reducing the providers’ average assessment time. Finally, several suggestions are offered to ensure fairness when dealing with out-of-order arrivals.




Similar content being viewed by others
References
Institute of Medicine (2001) Crossing the quality chasm: a new health system for the 21st century. National Academy Press, Washington DC
McCarthy K, McGee HM, O’Boyle CA (2000) Outpatient clinic waiting times and non-attendance as indicators of quality. Psychol Health Med 5:287–293
Rohleder TR, Lewkonia P, Bischak DP, Duffy P, Hendijani R (2011) Using simulation modeling to improve patient flow at an outpatient orthopedic clinic. Health Care Manag Sci 14:135–145
Savin S (2006) Managing patient appointments in primary care. In: Hall RW (ed) Patient flow: reducing delay in healthcare delivery. Springer, New York, pp 123–150, Chapter 5
O’Hare CD, Corlett J (2004) The outcomes of open-access scheduling. Fam Pract Manag 11(2):35–8
Cayirli T, Veral E (2003) Outpatient scheduling in health care: a review of literature. Prod Oper Manag 12(4):519–549
Nolan TW, Schall MW, Berwick DM, Roessner J (1996) Reducing delays and waiting times throughout the healthcare system. Institute for Healthcare Improvement, Cambridge
Murray M, Tantau C (2000) Same-day appointments: exploding the access paradigm. Fam Pract Manag 7–8:45–50
Forjuoh SN, Averitt WM, Cauthen DB, Symm B, Mitchell M (2001) Open-access appointment scheduling in family practice: comparison of a demand prediction grid with actual appointments. J Am Board Fam Pract 14(4):259–265
Murray M, Berwick DM (2003) Advance access: reducing waiting and delays in primary care. JAMA 289(8):1035–1039
Zamosky L (2014) What retail clinic growth can teach physicians about patient demand. Med Econ (January 8, 2014) http://medicaleconomics.modernmedicine.com
Dexter F, Traub RD (2002) How to schedule elective surgical cases into specific operating rooms to maximize the efficiency of use of operating room time. Anesth Analg 94:933–942
Gupta D, Denton B (2008) Appointment scheduling in health care: challenges and opportunities. IIE Trans Oper Eng 40(9):800–819
King DL, Ben-Tovim DI, Bassham J (2006) Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 18:391–397
Marmor YN, Golany B, Israelit S, Mandelbaum A (2012) Designing patient flow in emergency departments. IIE Trans Healthc Syst Eng 2(4):233–247
Zhang B, Murali P, Dessouky MM, Belson D (2009) A mixed integer programming approach for allocating operating room capacity. J Oper Res Soc 60(5):663–673
Jun J, Jacobson S, Swisher J (1999) Application of discrete-event simulation in health care clinics: a survey. J Oper Res Soc 50:109–123
Mahachek AR (1992) An introduction to patient flow simulation for health-care managers. J Soc Health Syst 3:73–81
Vanderby S, Carter MW (2010) An evaluation of the applicability of system dynamics to patient flow modeling. J Oper Res Soc 61(11):1572–1851
Coté MJ (1999) Patient flow and resource utilization in an outpatient clinic. Socioecon Plan Sci 33:231–245
Santibáñez P, Chow VS, French J, Puterman ML, Tyldesley S (2009) Reducing patient wait times and improving resource utilization at British Columbia Cancer Agency’s ambulatory care unit through simulation. Health Care Manag Sci 12:392–407
Berg B, Denton BT, Nelson H, Balasubramanian H, Rahman A, Bailey A, Lindor K (2010) A discrete event simulation model to evaluate operational performance of a colonoscopy suite. Med Decis Making 30(3):380–387
Klassen KJ, Rohleder TR (1996) Scheduling outpatient appointments in a dynamic environment. J Oper Manag 14:83–101
VanBerkel PT, Blake JT (2007) A comprehensive simulation for wait time reduction and capacity planning applied in general surgery. Health Care Manag Sci 10(4):373–385
Lane DC, Husemann E (2008) System dynamics mapping of acute patient flows. J Oper Res Soc 59(2):213–224
van Zon AH, Kommer GJ (1999) Patient flows and optimal health-care resource allocation at the macro-level: a dynamic linear programming approach. Health Care Manag Sci 2:87–96
Woodall JC, Gosselin T, Boswell A, Murr M, Denton BT (2013) Improving patient access to chemotherapy treatment at Duke Cancer Institute. Interfaces 43(5):449–461
Jenkins J, Gisler P (2012) Let my patients flow: lean diminishes gridlock at Central Baptist Hospital. Ind Eng 44(5):39–44
Proudlove N, Moxham C, Boaden R (2008) Lessons for lean in healthcare from using six sigma in the NHS. Public Money Manag 20(1):27–34
Kenney C (2011) Transforming health care: Virginia Mason Medical Center’s pursuit of the perfect patient experience. CRC Press, Boca Raton
Izard T (2005) Improving patient care: managing the habitual no-show patient. Fam Pract Manag 12(2):65–66
Noon CE, Hankins CT, Coté MJ (2003) Understanding the impact of variation in the delivery of healthcare services. J Healthc Manag 48:82–98
Millhiser WP, Veral EA, Valenti BC (2012) Assessing appointment systems’ operational performance with policy targets. IIE Trans Healthc Syst Eng 2:274–289
Muthuraman K, Lawley M (2008) A stochastic overbooking model for outpatient clinical scheduling with no-shows. IIE Trans Healthc Syst Eng 40(9):820–837
Chakraborty S, Muthuraman K, Lawley M (2010) Sequential clinical scheduling with patient no-shows and general service time distributions. IIE Trans Healthc Syst Eng 42(5):354–366
Chakraborty S, Muthuraman K, Lawley M (2013) Sequential clinical scheduling with patient no-show: the impact of pre-defined slot structures. Socioecon Plan Sci 47(3):205–219
LaGanga L, Lawrence S (2007) Clinic overbooking to improve patient access and increase provider productivity. Decis Sci 38:251–276
LaGanga L, Lawrence S (2012) Appointment overbooking in health care clinics to improve patient service and clinic performance. Prod Oper Manag 21(5):874–888
Robinson LW, Chen RR (2003) Scheduling doctors’ appointments: optimal and empirically-based heuristic policies. IIE Trans Healthc Syst Eng 35(3):295–307
Denton B, Gupta D (2003) A sequential bounding approach for optimal appointment scheduling. IIE Trans Healthc Syst Eng 35(11):1003–1016
Erdogan SA, Denton B (2013) Dynamic appointment scheduling of a stochastic server with uncertain demand. INFORMS J Comput 25(1):116–132
Mancilla C, Storer R (2012) A sample average approximation approach to stochastic appointment sequencing and scheduling. IIE Trans Healthc Syst Eng 44(8):655–670
Jiang L, Giachetti RE (2008) A queueing network model to analyze the impact of parallelization of care on patient cycle time. Health Care Manag Sci 11(3):248–261
Zonderland ME, Boer F, Boucherie RJ, de Roode A, van Kleef JW (2009) Redesign of a university hospital preanesthesia evaluation clinic using a queuing theory approach. Econ Educ Policy 109(5):1612–1621
Houck S (2004) What works: effective tools and case studies to improve clinical office practice. Health Press, Boulder
Alexopoulos C, Goldsman D, Fontanesi J, Kopald D, Wilson JR (2008) Modeling patient arrivals in community clinics. Omega 36(1):33–43
Oh H-J, Muriel A, Balasubramanian H, Atkinson K, Ptaszkiewicz T (2013) Guidelines for scheduling in primary care under different patient types and stochastic nurse and provider service times. IIE Trans Healthc Syst Eng 3(4):263–279
Dexter F, Ahn HS, Epstein RH (2013) Choosing which practitioner sees the next patient in the preanesthesia evaluation clinic based on the relative speeds of the practitioner. Anesth Analg 116(4):919–923
Sickinger S, Kolisch R (2009) The performance of a generalized Bailey–Welch rule for outpatient appointment scheduling under inpatient and emergency demand. Health Care Manag Sci 12(4):408–419
Sidak Z (1967) Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc 62:626–633
Green LV, Savin S, Wang B (2006) Managing patient service in a diagnostic medical facility. Oper Res 54(1):11–25
Kolisch R, Sickinger S (2008) Providing radiology health care services to stochastic demand of different customer classes. OR Spectr 30(2):375–395
Law AM, Kelton WD (2000) Simulation modeling and analysis 3rd edn. McGraw-Hill, New York
Acknowledgements
This work was supported by a grant from the University of Texas Office of the Executive Chancellor for Health Affairs. In addition, the authors would like to thank Poornachand Veerapaneni for his help in collecting data.
Author information
Authors and Affiliations
Corresponding author
Appendix A. Data collection form
Appendix A. Data collection form
Rights and permissions
About this article
Cite this article
Bard, J.F., Shu, Z., Morrice, D.J. et al. Improving patient flow at a family health clinic. Health Care Manag Sci 19, 170–191 (2016). https://doi.org/10.1007/s10729-014-9294-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-014-9294-y