Abstract
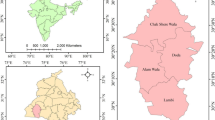
The city of Batna is currently experiencing major spatial disparities between the number of health facilities and their urban distribution. This situation has encouraged the re-evaluation of the functioning of the healthcare system and its spatial infrastructure deficit, especially regarding the proximity of healthcare facilities to the populations they cater to. This spatial deficit has resulted in a decrease in prevention program performance and the quality of healthcare. The aim of this paper is to measure the spatial healthcare inequalities in the city by quantifying the accessibility, delimiting the proximal service area, and detecting the distribution type based on a health-territory approach that integrates health dimension into a territorial master plan of the city using a geographic information system database developed for this purpose. The results confirm that accessibility is affected by the distribution of the health facilities as proposed by the urban master plan of the city. The proximity distances have increased, which provides an opportunity to maximise the service areas; however, it also creates a functional imbalance and overloads the health facilities.










Similar content being viewed by others
Notes
Plan Directeur d’Aménagement et d’Urbanisme.
In French: Zone habitat urbanisé nouvel.
La Grille théorique des equipement.
References
Abdelhalim, B., Hadda, D., Mahdi, K., & Baziz, N. (2016). Spatial analysis of typhoid fever vulnerability in the city of Batna (eastern Algeria). Environnement Risques & Santé, 15(3), 228–237. https://doi.org/10.1684/ers.2016.0861.
Apparicio, P., Abdelmajid, M., Riva, M., & Shearmur, R. (2008). Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. International Journal of Health Geographics, 7(1), 7. https://doi.org/10.1186/1476-072X-7-7.
Askari, M. H., Gupta, K., & Bengal, W. (2016). Conceptualising medical geography. Transactions, 38(1), 127.
Benachenhou, S. M., Benhabib, A., & Kessas, Z. (2011). L’influence de la qualité des soins sur la satisfaction des patients: Application de la méthode des équations structurelles. les cahiers du mecas, 7(1), 33–45.
Bensafi, A., & Djamel, E. H. (2017). Evaluation de la qualité à l’hôpital et satisfaction des patients. Horizons intellectuels, 3(7). Retrieved July 28, 2019, from https://www.univ-sba.dz/lrpia/images/revue_7/BENSAFI.ELHOUARI.pdf.
Bernia, H. Z. (2012). Préserver le foncier à haut rendement agricole, densifier le tissu urbain: cas d’el harrouch. Sciences & Technologie. D, Sciences de la terre 0(36), 45–50.
Billah, B. M., & Fatiha, B. (2014). La problématique du foncier à Constantine: cas des friches urbaines vierges. Sciences & technologie. D, Sciences de la terre, 40(4), 65–72.
Bouledroua, A. (2010). L’acces aux soins en Algérie Eléments pour une problématique sociologique du fait sanitaire. Revue Sciences Humaines, 21(1), 7–16.
Bouyoucef barr, D. (2015). L’organisation territoriale de l’offre de soins: quelles réalités en Algérie. La Revue des Sciences Commerciales, 14(1), 70–85.
Briney, A. (2014). Overview of public health and GIS. GIS Lounge. Retrieved August 4, 2019, from https://www.gislounge.com/overview-public-health-gis/.
Chachoua, P. L. (2014). Le système national de santé 1962 a nos jours. In Colloque International sur les Politiques de Santé Alger. Presented at the Colloque International sur les Politiques de Santé Alger, Alger: Ministère de la Santé, de la Population et de la Réforme Hospitalière en collaboration avec Ecole Nationale Supérieure en Sciences Politiques.
Chibani, K. (2015). Si BATNA m’était contee 1844–1962. A.Guerfi.
Cromley, E. K., & McLafferty, S. L. (2011). GIS and public health (2nd ed.). New York: Guilford Press.
Direction de l’Urbanisme de l’Architecture et de la Construction. (2012). Plan Directeur d’Aménagement et d’Urbanisme Inter-Commmunale. RGPH, commune de Batna: ONS.
Direction de la Programmation et du Suivi Budgétaires. (2017). Monograhie de Batna (Rapport annual) (p. 16). wilaya de Batna: Direction de la programmation et du suivi budgétaires Batna.
Elliott, S. (2014). Health geography. In A. C. Michalos (Ed.), Encyclopedia of quality of life and well-being research (pp. 2720–2725). Dordrecht: Springer. https://doi.org/10.1007/978-94-007-0753-5_1248.
Erickson, G. M., & Finkler, S. A. (1985). Determinants of market share for a hospital’s services. Medical Care, 23(8), 1003–1018.
Esri. (2019a). How average nearest neighbor works. Retrieved February 28, 2019, from http://desktop.arcgis.com/en/arcmap/10.3/tools/spatial-statistics-toolbox/h-how-average-nearest-neighbor-distance-spatial-st.htm.
Esri, H. | A. D. (2019b). How proximity tools calculate distance. Retrieved February 28, 2019, from https://pro.arcgis.com/en/pro-app/tool-reference/analysis/how-near-analysis-works.htm.
Evans, D. B., Hsu, J., & Boerma, T. (2013). Universal health coverage and universal access. Bulletin of the World Health Organization, 91(8), 546A. https://doi.org/10.2471/BLT.13.125450.
Garnick, D. W., Luft, H. S., Robinson, J. C., & Tetreault, J. (1987). Appropriate measures of hospital market areas. Health Services Research, 22(1), 69.
Guerrero, E. G., & Kao, D. (2013). Racial/ethnic minority and low-income hotspots and their geographic proximity to integrated care providers. Substance Abuse Treatment, Prevention, and Policy, 8(1), 34.
Hayette, H. (2017). Extension urbaine et consommation du foncier agricole; quelle responsabilité des instruments d’urbanisme? Cas de Skikda, Algérie. The Urban Planning and Construction Review, 1(4), 309–331.
Higgs, G. (2004). A literature review of the use of GIS-based measures of access to health care services. Health Services and Outcomes Research Methodology, 5(2), 119–139. https://doi.org/10.1007/s10742-005-4304-7.
Issam, K. M., & Said, G. M. (2017). Using geomatics for assessing vulnerability to cutaneous leishmanisais. Application to the Wilaya of Batna (Algeria). International Journal of GEOMATE, 13(40), 9–15. https://doi.org/10.21660/2017.40.25868.
Jonsson, F., Sebastian, M. S., Hammarström, A., & Gustafsson, P. E. (2018). Are neighbourhood inequalities in adult health explained by socio-economic and psychosocial determinants in adolescence and the subsequent life course in northern Sweden? A decomposition analysis. Health & Place, 52, 127–134. https://doi.org/10.1016/j.healthplace.2018.05.010.
Kiani, B., Bagheri, N., Tara, A., Hoseini, B., Hashtarkhani, S., & Tara, M. (2018). Comparing potential spatial access with self-reported travel times and cost analysis to haemodialysis facilities in North-eastern Iran. Geospatial Health. https://doi.org/10.4081/gh.2018.703.
Lin, Y., Wimberly, M. C., Da Rosa, P., Hoover, J., & Athas, W. F. (2018). Geographic access to radiation therapy facilities and disparities of early-stage breast cancer treatment. Geospatial Health. https://doi.org/10.4081/gh.2018.622.
Louhi, D. (2009). La ville algérienne, les prémices d’une gouvernance locale. Site de référence: Annaba. Sciences & Technologie. D, Sciences de la terre, 0(30), 53–70.
Lu, H., Zhang, X., Holt, J. B., Kanny, D., & Croft, J. B. (2018). Quantifying spatial accessibility in public health practice and research: An application to on-premise alcohol outlets, United States, 2013. International Journal of Health Geographics, 17(1), 23. https://doi.org/10.1186/s12942-018-0143-y.
Luo, W., & Wang, F. (2003). Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago Region. Environment and Planning B: Planning and Design, 30(6), 865–884. https://doi.org/10.1068/b29120.
Maron, J., Gomes de Matos, E., Piontek, D., Kraus, L., & Pogarell, O. (2019). Exploring socio-economic inequalities in the use of medicines: Is the relation mediated by health status? Public Health, 169, 1–9. https://doi.org/10.1016/j.puhe.2018.12.018.
Matthews, K. A., Gaglioti, A. H., Holt, J. B., Wheaton, A. G., & Croft, J. B. (2019). Using spatially adaptive floating catchments to measure the geographic availability of a health care service: Pulmonary rehabilitation in the southeastern United States. Health & Place, 56, 165–173. https://doi.org/10.1016/j.healthplace.2019.01.017.
McGrail, M. R., & Humphreys, J. S. (2014). Measuring spatial accessibility to primary health care services: Utilising dynamic catchment sizes. Applied Geography, 54, 182–188. https://doi.org/10.1016/j.apgeog.2014.08.005.
Mitchel, A. (2005). The ESRI Guide to GIS analysis: Spatial measurements and statistics (Vol. 2). Redlands: ESRI Press.
Mohamed, L., & Djamal, S.-M. (2018). Dynamiques d’urbanisation de la ville d’Alger: quelles opportunités pour le développement territorial? Dynamics of urbanization of the city of Algiers: What opportunities for territorial development? El-bahith review, 18(1), 665–678. https://doi.org/10.35156/0505-000-018-047.
Nasereddine, A. (2016a). The conditions of risk management in health facilities—Case study of public institutions nearby care of Algéria/EPSP. Ruʼá Iqtiṣadīyah, 6(10), 283–301. https://doi.org/10.12816/0034060.
Nasereddine, A. (2016b). Les déterminants de l’accessibilité aux services de soins en Algérie–le cas des services de soins de proximité. Journal of Financial Accounting and Managerial Studies, 3(1), 103–122.
Near—Help | ArcGIS for Desktop. (2019). Retrieved February 12, 2020, from https://desktop.arcgis.com/en/arcmap/10.3/tools/analysis-toolbox/near.htm.
Nemet, G. F., & Bailey, A. J. (2000). Distance and health care utilization among the rural elderly. Social Science and Medicine, 50(9), 1197–1208. https://doi.org/10.1016/s0277-9536(99)00365-2.
Office National des Statistiques. (2011). ARMATURE URBAIN (Série S: Statistiques Sociales No. Collections Statistiques N: 163/2011) (p. 72). Algeria: La Direction Technique Chargée des Statistiques Régionales, l’Agriculture et de la Cartographie. Retrieved January 1, 2020, from http://www.ons.dz/IMG/pdf/armature_urbaine_2008.pdf.
Okabe, A., Satoh, T., Furuta, T., Suzuki, A., & Okano, K. (2008). Generalized network Voronoi diagrams: Concepts, computational methods, and applications. International Journal of Geographical Information Science, 22(9), 965–994.
Oufriha, F. Z. (2006a). les reforme du systeme de sante en algerie. In F. Z. Oufriha (Ed.), De réforme en réforme: un système de santé à la croisée des chemins (pp. 103–116). Alger: Ed. CREAD.
Oufriha, F. Z. (2006b). Les depenses de sante dans le monde:de lexploitation a la maitrise. In F. Z. Oufriha (Ed.), De réforme en réforme: un système de santé à la croisée des chemins (pp. 13–32). Alger: Ed. CREAD.
Pan, J., Liu, H., Wang, X., Xie, H., & Delamater, P. L. (2015). Assessing the spatial accessibility of hospital care in Sichuan Province, China. Geospatial Health. https://doi.org/10.4081/gh.2015.384.
Peipins, L. A., Graham, S., Young, R., Lewis, B., & Flanagan, B. (2013). Racial disparities in travel time to radiotherapy facilities in the Atlanta metropolitan area. Social Science and Medicine, 89, 32–38.
Shin, K., & Lee, T. (2018). Improving the measurement of the Korean emergency medical System’s spatial accessibility. Applied Geography, 100, 30–38. https://doi.org/10.1016/j.apgeog.2018.08.009.
Swaminathan, H., Sharma, A., & Shah, N. G. (2019). Does the relationship between income and child health differ across income groups? Evidence from India. Economic Modelling, 79, 57–73. https://doi.org/10.1016/j.econmod.2018.10.001.
Winchester, M. S., & King, B. (2018). Decentralization, healthcare access, and inequality in Mpumalanga, South Africa. Health & Place, 51, 200–207. https://doi.org/10.1016/j.healthplace.2018.02.009.
World Health Organization (Ed.). (2010). Monitoring the building blocks of health systems: A handbook of indicators and their measurement strategies. Geneva: World Health Organization. Retrieved March 25, 2019, from https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf?ua=1.
Xia, T., Song, X., Zhang, H., Song, X., Kanasugi, H., & Shibasaki, R. (2019). Measuring spatio-temporal accessibility to emergency medical services through big GPS data. Health & Place, 56, 53–62. https://doi.org/10.1016/j.healthplace.2019.01.012.
Xiong, X., & Luo, L. (2017). Use of geographical information systems for delimiting health service areas in China. Geospatial Health. https://doi.org/10.4081/gh.2017.486.
Yang, D.-H., Goerge, R., & Mullner, R. (2006). Comparing GIS-based methods of measuring spatial accessibility to health services. Journal of Medical Systems, 30(1), 23–32. https://doi.org/10.1007/s10916-006-7400-5.
Yin, C., He, Q., Liu, Y., Chen, W., & Gao, Y. (2018). Inequality of public health and its role in spatial accessibility to medical facilities in China. Applied Geography, 92, 50–62. https://doi.org/10.1016/j.apgeog.2018.01.011.
Zehnati, A. (2017). Les évolutions récentes du système de santré algrérien. Alger: Ed. CREAD.
Zhang, Q., Northridge, M. E., Jin, Z., & Metcalf, S. S. (2018). Modeling accessibility of screening and treatment facilities for older adults using transportation networks. Applied Geography, 93, 64–75. https://doi.org/10.1016/j.apgeog.2018.02.013.
Funding
This study was not funded by any company or any person.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors (Dr. LAHMAR Belkacem, Pr. DRIDI Hadda and Dr. AKAKBA Ahmed) declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lahmar, B., Dridi, H. & Akakba, A. Territorial health approach outputs of geo-governance of health facilities: case study of Batna, Algeria. GeoJournal 86, 2305–2319 (2021). https://doi.org/10.1007/s10708-020-10189-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10708-020-10189-1