Abstract
Germline genetic sequencing is now at the forefront of cancer treatment and preventative medicine. Cascade genetic testing, or the testing of at-risk relatives, is extremely promising as it offers genetic testing and potentially life-saving risk-reduction strategies to a population exponentially enriched for the risk of carrying a cancer-associated pathogenic variant. However, many relatives do not complete cascade testing due to barriers that span individual, relationship, healthcare community, and societal/policy domains. We have reviewed the published research on cascade testing. Our aim is to evaluate barriers to cascade genetic testing for hereditary cancer syndromes and explore strategies to mitigate these barriers, with the goal of promoting increased uptake of cascade genetic testing.

Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
Bibliography
Whitaker KD et al Cascade Genetic Testing for Hereditary Cancer Risk: An Underutilized Tool for Cancer Prevention. JCO Precision Oncol, 2021(5):1387–1396
Offit K et al (2020) Cascading after Peridiagnostic Cancer Genetic Testing: an alternative to Population-based screening. J Clin Oncol 38(13):1398–1408
Domchek SM et al (2010) Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 304(9):967–975
de Jong AE et al (2006) Decrease in mortality in Lynch syndrome families because of surveillance. Gastroenterology 130(3):665–671
Center for Disease Control and Prevention Tier 1 Genomic Applications Toolkit for Public Health Departments. [cited 2019 12/9/2019]; Available from: https://www.cdc.gov/genomics/implementation/toolkit/
Owens DK, Assessment R et al (2019) Genetic counseling, and genetic testing for BRCA-Related Cancer: US Preventive Services Task Force Recommendation Statement. JAMA 322(7):652–665
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Genetic/Familial High-Risk Assessment: Colorectal - Version 1.2023 — May 30 (2023)
NCCN Clinical Practice Guidelines in Oncology (2022) : Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic. 2022
Childers CP et al (2017) National Estimates of Genetic Testing in Women with a history of breast or ovarian Cancer. J Clin Oncol 35(34):3800–3806
Drohan B et al (2012) Hereditary breast and ovarian cancer and other hereditary syndromes: using technology to identify carriers. Ann Surg Oncol 19(6):1732–1737
Frey MK et al (2022) Cascade Testing for Hereditary Cancer syndromes: should we move toward direct relative contact? A systematic review and Meta-analysis. J Clin Oncol 40(35):4129–4143
Roberts MC et al (2018) Delivery of Cascade Screening for Hereditary conditions: a scoping review of the literature. Health Aff (Millwood) 37(5):801–808
Registry A (2015) f.T.S.a.D. Models and Frameworks for the Practice of Community Engagement. ; Available from: https://www.atsdr.cdc.gov/communityengagement/pce_models.html
Organization WH (1947) Constitution of the World Health Organization. Chron World Health Organ 1(1–2):29–43
Sallis JF, Owen N, Fisher EB (2008) Ecological models of health behavior. Health behavior and health education: theory, research, and practice, 4th edn. Jossey-Bass, San Francisco, CA, US, pp 465–485
Wallerstein N, D.B., The conceptual, historical and practice roots of community-based participatory research and related participatory traditions, in Community-based participatory research for health, Minkler WN (2003) M, Editor. Jossey-Bass: San Francisco. p. 27–52
Israel BA, Parker SA, Becker EA, Allen AB, Guzman AJ JR Critical issues in developing and following community-based participatory research principles, in Community-based participatory research for health, Minkler WN (2003) M, Editor. Jossey-Bass: San Francisco. p. 53–76
Aktan-Collan KI et al (2011) Sharing genetic risk with next generation: mutation-positive parents’ communication with their offspring in Lynch Syndrome. Fam Cancer 10(1):43–50
Alegre N et al (2019) Psychosocial and clinical factors of probands impacting intrafamilial disclosure and uptake of genetic testing among families with BRCA1/2 or MMR gene mutations. Psychooncology 28(8):1679–1686
Blandy C et al (2003) Testing participation in BRCA1/2-positive families: initiator role of index cases. Genet Test 7(3):225–233
Bruwer Z, Futter M, Ramesar R (2013) Communicating cancer risk within an African context: experiences, disclosure patterns and uptake rates following genetic testing for Lynch syndrome. Patient Educ Couns 92(1):53–60
Dilzell K et al (2014) Evaluating the utilization of educational materials in communicating about Lynch syndrome to at-risk relatives. Fam Cancer 13(3):381–389
Gaff CL et al (2005) Facilitating family communication about predictive genetic testing: probands’ perceptions. J Genet Couns 14(2):133–140
Griffin NE et al (2020) Low rates of cascade genetic testing among families with hereditary gynecologic cancer: an opportunity to improve cancer prevention. Gynecol Oncol 156(1):140–146
Healey E et al (2017) Quantifying family dissemination and identifying barriers to communication of risk information in Australian BRCA families. Genet Med 19(12):1323–1331
Hayat Roshanai A et al (2010) Disclosing cancer genetic information within families: perspectives of counselees and their at-risk relatives. Fam Cancer 9(4):669–679
Landsbergen K et al (2005) Genetic uptake in BRCA-mutation families is related to emotional and behavioral communication characteristics of index patients. Fam Cancer 4(2):115–119
Frey MK et al (2020) Prospective feasibility trial of a Novel Strategy of facilitated Cascade genetic testing using telephone counseling. J Clin Oncol 38(13):1389–1397
Finlay E et al (2008) Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genet Test 12(1):81–91
Wagner Costalas J et al (2003) Communication of BRCA1 and BRCA2 results to at-risk relatives: a cancer risk assessment program’s experience. Am J Med Genet C Semin Med Genet 119 C(1):11–18
McGivern B et al (2004) Family communication about positive BRCA1 and BRCA2 genetic test results. Genet Med 6(6):503–509
Forrest LE et al (2008) Increased genetic counseling support improves communication of genetic information in families. Genet Med 10(3):167–172
Srinivasan S et al (2020) Stakeholder perspectives on overcoming barriers to Cascade Testing in Lynch Syndrome: a qualitative study. Cancer Prev Res (Phila) 13(12):1037–1046
Montgomery SV et al (2013) Preparing individuals to communicate genetic test results to their relatives: report of a randomized control trial. Fam Cancer 12(3):537–546
Stoffel EM et al (2008) Sharing genetic test results in Lynch syndrome: communication with close and distant relatives. Clin Gastroenterol Hepatol 6(3):333–338
Cheung EL et al (2010) Communication of BRCA results and family testing in 1,103 high-risk women. Cancer Epidemiol Biomarkers Prev 19(9):2211–2219
Kardashian A et al (2012) A pilot study of the sharing Risk Information Tool (ShaRIT) for families with Hereditary breast and ovarian Cancer syndrome. Hered Cancer Clin Pract 10(1):4
Hall ET et al (2018) Pathogenic variants in Less Familiar Cancer susceptibility genes: what happens after genetic testing? JCO Precis Oncol. 2:1–10
Taber JM et al (2015) Prevalence and correlates of receiving and sharing high-penetrance cancer genetic test results: findings from the Health Information National Trends Survey. Public Health Genomics 18(2):67–77
Lerman C et al (1996) BRCA1 testing in families with hereditary breast-ovarian cancer. A prospective study of patient decision making and outcomes. JAMA 275(24):1885–1892
Hadley DW et al (2003) Genetic counseling and testing in families with hereditary nonpolyposis colorectal cancer. Arch Intern Med 163(5):573–582
Leenen CH et al (2016) Genetic testing for Lynch syndrome: family communication and motivation. Fam Cancer 15(1):63–73
Rauscher EA, Dean M, Campbell-Salome GM (2018) Uncertain about what my uncertainty even is: men’s uncertainty and Information Management of their BRCA-Related Cancer risks. J Genet Couns 27(6):1417–1427
Kahn RM et al (2023) Barriers to completion of cascade genetic testing: how can we improve the uptake of testing for hereditary breast and ovarian cancer syndrome? Fam Cancer 22(2):127–133
Aktan-Collan K et al (2000) Predictive genetic testing for hereditary non-polyposis colorectal cancer: uptake and long-term satisfaction. Int J Cancer 89(1):44–50
Ramsoekh D et al (2007) The use of genetic testing in hereditary colorectal cancer syndromes: genetic testing in HNPCC, (A)FAP and MAP. Clin Genet 72(6):562–567
Biesecker BB et al (2000) Psychosocial factors predicting BRCA1/BRCA2 testing decisions in members of hereditary breast and ovarian cancer families. Am J Med Genet 93(4):257–263
Courtney E et al (2019) Impact of free cancer predisposition cascade genetic testing on uptake in Singapore. NPJ Genom Med 4:22
Bodd TL et al (2003) Uptake of BRCA1 genetic testing in adult sisters and daughters of known mutation carriers in Norway. J Genet Couns 12(5):405–417
Lieberman S et al (2018) Familial communication and cascade testing among relatives of BRCA population screening participants. Genet Med 20(11):1446–1454
de Snoo FA et al (2008) Genetic testing in familial melanoma: uptake and implications. Psychooncology 17(8):790–796
de Ponz M et al (2004) Genetic testing among high-risk individuals in families with hereditary nonpolyposis colorectal cancer. Br J Cancer 90(4):882–887
Lammens CR et al (2010) Genetic testing in Li-Fraumeni syndrome: uptake and psychosocial consequences. J Clin Oncol 28(18):3008–3014
Donenberg T et al (2019) A clinically structured and partnered approach to genetic testing in Trinidadian women with breast cancer and their families. Breast Cancer Res Treat 174(2):469–477
Srinivasan S et al (2020) Barriers and facilitators for cascade testing in genetic conditions: a systematic review. Eur J Hum Genet 28(12):1631–1644
Petersen J et al (2018) Patterns of family communication and preferred resources for sharing information among families with a Lynch syndrome diagnosis. Patient Educ Couns 101(11):2011–2017
Peterson SK et al (2003) How families communicate about HNPCC genetic testing: findings from a qualitative study. Am J Med Genet C Semin Med Genet 119 C(1):78–86
Sanz J et al (2010) Uptake of predictive testing among relatives of BRCA1 and BRCA2 families: a multicenter study in northeastern Spain. Fam Cancer 9(3):297–304
Fehniger J et al (2013) Family communication of BRCA1/2 results and family uptake of BRCA1/2 testing in a diverse population of BRCA1/2 carriers. J Genet Couns 22(5):603–612
Dancyger C et al (2011) Communicating BRCA1/2 genetic test results within the family: a qualitative analysis. Psychol Health 26(8):1018–1035
Chanita Hughes HL, Durham C, Snyder C, Lemon S, Narod S, Fulmore C, Main D (1999) Caryn Lerman, communication of BRCAl/2 test results in hereditary breast cancer families. Cancer Res Therapy Control 8:51–59
Garcia C et al (2020) Mechanisms to increase cascade testing in hereditary breast and ovarian cancer: impact of introducing standardized communication aids into genetic counseling. J Obstet Gynaecol Res 46(9):1835–1841
Patenaude AF et al (2006) Sharing BRCA1/2 test results with first-degree relatives: factors predicting who women tell. J Clin Oncol 24(4):700–706
Elrick A et al (2017) Psychosocial and Clinical Factors Associated with Family Communication of Cancer Genetic Test results among women diagnosed with breast Cancer at a young age. J Genet Couns 26(1):173–181
Phillips KA et al (2018) Genetic test availability and spending: where are we now? Where are we going? Health Aff (Millwood) 37(5):710–716
Lin J et al (2021) Achieving universal genetic assessment for women with ovarian cancer: are we there yet? A systematic review and meta-analysis. Gynecol Oncol 162(2):506–516
Huang M et al (2019) Identifying disparities in germline and somatic testing for ovarian cancer. Gynecol Oncol 153(2):297–303
Mansur A, Zhang F, Lu CY (2022) Association between Health Insurance Type and genetic testing and/or counseling for breast and ovarian Cancer. J Pers Med, 12(8)
Doyle TA, Conboy E, Halverson CME (2023) Diagnostic deserts: community-level barriers to appropriate genetics services. Am J Med Genet A 191(1):296–298
Martins MF et al (2022) Direct-to-consumer genetic testing: an updated systematic review of healthcare professionals’ knowledge and views, and ethical and legal concerns. Eur J Hum Genet 30(12):1331–1343
Salloum RG et al (2018) Rural-urban and racial-ethnic differences in awareness of direct-to-consumer genetic testing. BMC Public Health 18(1):277
Levy DE et al (2011) Underutilization of BRCA1/2 testing to guide breast cancer treatment: black and hispanic women particularly at risk. Genet Med 13(4):349–355
Nikolaidis C et al (2019) Disparities in genetic services utilization in a random sample of young breast cancer survivors. Genet Med 21(6):1363–1370
Cragun D et al (2017) Racial disparities in BRCA testing and cancer risk management across a population-based sample of young breast cancer survivors. Cancer 123(13):2497–2505
McGuinness JE et al (2019) Uptake of genetic testing for germline BRCA1/2 pathogenic variants in a predominantly hispanic population. Cancer Genet, 235–236: p. 72–76
Chapman-Davis E et al (2021) Racial and ethnic disparities in genetic testing at a Hereditary breast and ovarian Cancer Center. J Gen Intern Med 36(1):35–42
Stamp MH et al (2019) Painting a portrait: analysis of national health survey data for cancer genetic counseling. Cancer Med 8(3):1306–1314
Green RF et al (2019) Evaluating the role of public health in implementation of genomics-related recommendations: a case study of hereditary cancers using the CDC Science Impact Framework. Genet Med 21(1):28–37
Hall MJ, Olopade OI (2006) Disparities in genetic testing: thinking outside the BRCA Box. J Clin Oncol 24(14):2197–2203
Shields AE, Burke W, Levy DE (2008) Differential use of available genetic tests among primary care physicians in the United States: results of a national survey. Genet Med 10(6):404–414
Vadaparampil ST, McIntyre J, Quinn GP (2010) Awareness, perceptions, and provider recommendation related to genetic testing for hereditary breast cancer risk among at-risk hispanic women: similarities and variations by sub-ethnicity. J Genet Couns 19(6):618–629
Armstrong J et al (2015) Utilization and outcomes of BRCA Genetic Testing and Counseling in a National Commercially Insured Population: the ABOUT Study. JAMA Oncol 1(9):1251–1260
Kassem NM et al (2023) Racial disparities in cascade testing for cancer predisposition genes. Prev Med 172:107539
Ahsan MD et al (2023) Underrepresentation of racial and ethnic minorities in cascade testing for hereditary cancer syndromes. Eur J Hum Genet 31(7):723–724
Medicine, N.U.S.N.L.o. Cascade Testing, Clinicaltrials.gov. 2023; Available from:https://classic.clinicaltrials.gov/ct2/results?term=cascade+testing&Search=Apply&recrs=a&age_v=&gndr=&type=&rslt=.
Dugueperoux I et al (2016) Highlighting the impact of cascade carrier testing in cystic fibrosis families. J Cyst Fibros 15(4):452–459
Whitaker KD et al (2021) Cascade Genetic Testing for Hereditary Cancer Risk: An Underutilized Tool for Cancer Prevention. JCO Precis Oncol 5:1387–1396
Campbell M, Humanki J, Zierhut H (2017) A novel approach to screening for familial hypercholesterolemia in a large public venue. J Community Genet 8(1):35–44
Henrikson NB et al (2020) What guidance does HIPAA offer to providers considering familial risk notification and cascade genetic testing? J Law Biosci 7(1):lsaa071
Office of the Secretary, Standards for Privacy of Individually Identifiable Health Information. § 67 Fed. Reg. 164.506 (2000)
Institute NHGR, GENETIC DISCRIMINATION (2023) ; Available from: https://www.genome.gov/genetics-glossary/Genetic-Discrimination
Hughes C et al (1999) Communication of BRCAl/2 test results in hereditary breast cancer families. Cancer Res Therapy Control 8(1–2):51–59
Yoon SY et al (2011) Genetic counseling for patients and families with hereditary breast and ovarian cancer in a developing Asian country: an observational descriptive study. Fam Cancer 10(2):199–205
Hughes C et al (2002) All in the family: evaluation of the process and content of sisters’ communication about BRCA1 and BRCA2 genetic test results. Am J Med Genet 107(2):143–150
The Genetic Information (2008) Nondiscrimination Act of 2008, U.S.E.E.O. Commission, Editor
Rothstein MA (2018) Time to end the use of genetic test results in Life Insurance underwriting. J Law Med Ethics 46(3):794–801
Tenenbaum JD, Goodman KW (2017) Beyond the genetic information nondiscrimination act: ethical and economic implications of the exclusion of disability, long-term care and life insurance. Per Med 14(2):153–157
Lapointe J et al (2013) Life events may contribute to family communication about cancer risk following BRCA1/2 testing. J Genet Couns 22(2):249–257
MacDonald DJ, Blazer KR, Weitzel JN (2010) Extending comprehensive cancer center expertise in clinical cancer genetics and genomics to diverse communities: the power of partnership. J Natl Compr Canc Netw 8(5):615–624
Kastner AM et al (2023) Distress, anxiety, and depression in persons with hereditary cancer syndromes: results from a nationwide cross-sectional study in Germany. Cancer Med 12(12):13701–13711
O’Neill SC et al (2021) Improving our model of cascade testing for hereditary cancer risk by leveraging patient peer support: a concept report. Hered Cancer Clin Pract 19(1):40
Tercyak KP et al (2015) Survey on addressing the information and support needs of jewish women at increased risk for or diagnosed with breast Cancer: the Sharsheret experience. Healthc (Basel) 3(2):324–337
Bhatnagar D et al (2000) Outcome of case finding among relatives of patients with known heterozygous familial hypercholesterolaemia. BMJ 321(7275):1497–1500
Wright C et al (2002) Comparison of genetic services with and without genetic registers: knowledge, adjustment, and attitudes about genetic counselling among probands referred to three genetic clinics. J Med Genet 39(12):e84
Schmidlen T et al (2022) Use of a chatbot to increase uptake of cascade genetic testing. J Genet Couns 31(5):1219–1230
Russo J et al (2021) Pretest Genetic Education Video Versus Genetic Counseling for men considering prostate Cancer germline testing: a patient-choice study to address urgent practice needs. JCO Precis Oncol, p 5
Athens BA et al (2017) A systematic review of Randomized controlled trials to assess outcomes of genetic counseling. J Genet Couns 26(5):902–933
Breen KE et al (2022) Factors influencing patient preferences for Telehealth Cancer Genetic Counseling during the COVID-19 pandemic. JCO Oncol Pract 18(4):e462–e471
Brown EG et al (2021) Videoconferencing to deliver genetics services: a systematic review of telegenetics in light of the COVID-19 pandemic. Genet Med 23(8):1438–1449
Swisher EM et al (2023) Remotely delivered Cancer Genetic Testing in the making genetic testing accessible (MAGENTA) trial: a Randomized Clinical Trial. JAMA Oncol vol 9(11):1547–1555. https://doi.org/10.1001/jamaoncol.2023.3748
Acknowledgements
Melissa K Frey was supported by the following grant: American Association of Obstetricians and Gynecologists Foundation/American Board of Obstetrics & Gynecology (AAOGF/ABOG) Career Development Award.
Author information
Authors and Affiliations
Contributions
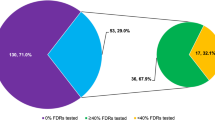
R.L., R.K. M.F, J.B. wrote the main manuscript text, J.B. prepared figure. L.P., S.R., X.L., E.Y. M.F. edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Levine, R., Kahn, R.M., Perez, L. et al. Cascade genetic testing for hereditary cancer syndromes: a review of barriers and breakthroughs. Familial Cancer (2024). https://doi.org/10.1007/s10689-024-00373-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10689-024-00373-4