Abstract
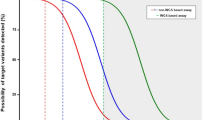
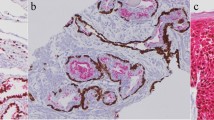
Lynch syndrome (LS) is associated with an increased lifetime risk of several cancers including colorectal (CRC), endometrial (EC), ovarian (OC), urinary (UT) and sebaceous tumors (ST). The benefit for universal screening in CRC and EC is well known. However, this benefit in other major lynch-associated tumors is unclear. We performed a systematic review of all published articles in the MEDLINE database between 2005 to 2017 to identify studies performing universal screening for LS in unselected CRC, EC, OC, UT and ST. All cases with MSI-H (instability in two or more markers) or missing one or more proteins on IHC testing were considered screening positive. Cases with MLH1 promoter hypermethylation or BRAF mutation positive were considered to have somatic mutations. A total of 3788 articles were identified in MEDLINE yielding 129 study arms from 113 studies. The overall pooled yield of universal LS screening and germline mismatch gene mutation was significantly different across the major LS-associated tumors (Mann Whitney test, p < 0.001). The pooled screening yield was highest in ST [52.5% (355/676), 95% CI 48.74–56.26%] followed by EC [22.65% (1142/5041), 95% CI 21.54–23.86%], CRC [11.9% (5649/47,545), 95% CI 11.61–12.19%], OC [11.29% (320/2833), 95% CI 10.13–12.47%] and UT [11.2% (31/276), 95% CI 7.48–14.92%]. ST also had the highest pooled germline positivity for mismatch repair gene mutation [18.8%, 33/176, 95%CI 13.03–24.57], followed by EC [2.6% (97/3765), 95% CI 2.09–3.11], CRC [1.8% (682/37,220), 95% CI 1.66–1.94%], UT [1.8%(3/164), 95% CI − 0.24–3.83%] and OC [0.83%(25/2983), 95% CI 0.48–1.12%]. LS screening in EC yielded significantly higher somatic mutations compared to CRC [pooled percentage 16.94% [(538/3176), 95%CI 15.60–18.20%] vs. 5.23% [(1639/26,152), 95% CI 4.93–5.47%], Mann Whitney test, p < 0.0001. Universal LS testing should be routinely performed in OC, UT and STs in addition to CRC and EC. Our findings also support consideration for IHC and somatic mutation testing before germline testing in EC due to higher prevalence of somatic mutations as well as germline testing in all patients with ST. Our results have implications for future design of LS screening programs and further studies are needed to assess the cost effectiveness and burden on genetic counselling services with expanded universal testing for LS.


Similar content being viewed by others
Abbreviations
- LS:
-
Lynch syndrome
- CRC:
-
Colorectal cancer
- EC:
-
Endometrial cancer
- OC:
-
Ovarian cancer
- UT:
-
Uterine cancer
- ST:
-
Sebaceous tumors
- MSI:
-
Microsatellite instability
- IHC:
-
Immunohistochemistry
- MMR:
-
Mismatch repair
References
Giardiello FM, Allen JI, Axilbund JE et al (2014) Guidelines on genetic evaluation and management of Lynch syndrome: a consensus statement by the US Multi-society Task Force on colorectal cancer. Am J Gastroenterol 109:1159–1179
Lynch HT, Lynch JF (2005) What the physician needs to know about Lynch syndrome: an update. Oncology (Williston Park) 19:455–463
Kanth P, Grimmett J, Champine M et al (2017) Hereditary colorectal polyposis and cancer syndromes: a primer on diagnosis and management. Am J Gastroenterol 112:1509–1525
Koeneman M, Kruse AJ, Gubbels CS et al (2013) Routine use of a screening questionnaire improves detection of individuals at possible risk of hereditary gynecologic cancer. Int J Gynecol Cancer 23:628
Akbari MR, Zhang S, Cragun D et al (2017) Correlation between germline mutations in MMR genes and microsatellite instability in ovarian cancer specimens. Fam Cancer 16:351–355
Roupret M, Coulet F, Azzouzi A-R et al (2005) Accuracy of the routine detection of mutation in mismatch repair genes in patients with susceptibility to hereditary upper urinary tract transitional cell carcinoma. BJU Int 96:149–151
Lynch HT, Lynch PM, Pester J et al (1981) The cancer family syndrome. Rare cutaneous phenotypic linkage of Torre’s syndrome. Arch Intern Med 141:607–611
Randall LM, Pothuri B, Swisher EM et al (2017) Multi-disciplinary summit on genetics services for women with gynecologic cancers: a Society of Gynecologic Oncology White Paper. GynecolOncol 146:217
Kunnackal John G, Das Villgran V, Caufield-Noll C et al (2020) Worldwide variation in lynch syndrome screening: case for universal screening in low colorectal cancer prevalence areas. Fam Cancer. https://doi.org/10.1007/s10689-020-00206-0
Lamba AR, Moore AY, Moore T et al (2015) Defective DNA mismatch repair activity is common in sebaceous neoplasms, and may be an ineffective approach to screen for Lynch syndrome. Fam Cancer 14:259–264
Plocharczyk EF, Frankel WL, Hampel H et al (2013) Mismatch repair protein deficiency is common in sebaceous neoplasms and suggests the importance of screening for Lynch syndrome. Am J Dermatopathol 35:191–195
Ward RL, Turner J, Williams R et al (2005) Routine testing for mismatch repair deficiency in sporadic colorectal cancer is justified. J Pathol 207:377–384
Hampel H, Frankel WL, Martin E et al (2005) Screening for the Lynch syndrome (hereditary nonpolyposis colorectal cancer). N Engl J Med 352:1851–1860
Lamberti C, Mangold E, Pagenstecher C et al (2006) Frequency of hereditary non-polyposis colorectal cancer among unselected patients with colorectal cancer in Germany. Digestion 74:58–67
Bishehsari F, Mahdavinia M, Malekzadeh R et al (2006) Patterns of K-ras mutation in colorectal carcinomas from Iran and Italy (a GruppoOncologicodell’ItaliaMeridionale study): influence of microsatellite instability status and country of origin. Ann Oncol 17:91–96
Shpitz B, Millman M, Ziv Y et al (2006) Predominance of younger age, advanced stage, poorly-differentiated and mucinous histology in Israeli Arab patients with colorectal cancer. Anticancer Res 26:533–537
Chang EY, Dorsey PB, Johnson N et al (2006) A prospective analysis of microsatellite instability as a molecular marker in colorectal cancer. Am J Surg 191:646–651
Yearsley M, Hampel H, Lehman A et al (2006) Histologic features distinguish microsatellite-high from microsatellite-low and microsatellite-stable colorectal carcinomas, but do not differentiate germline mutations from methylation of the MLH1 promoter. Hum Pathol 37:831–838
Jin H-Y, Ding Y-J, Liu X-F et al (2007) Screening the hereditary nonpolyposis colorectal cancer by revised Bethesda guideline: a cohort study of 110 cases. Chung-Hua Hsueh TsaChih 87:1445–1447
Tan LP, Ng BK, Balraj P et al (2007) No difference in the occurrence of mismatch repair defects and APC and CTNNB1 genes mutation in a multi-racial colorectal carcinoma patient cohort. Pathology 39:228–234
Deschoolmeester V, Baay M, Wuyts W et al (2008) Detection of microsatellite instability in colorectal cancer using an alternative multiplex assay of quasi-monomorphic mononucleotide markers. J MolDiagn 10:154–159
Yan H-L, Hao L-Q, Jin H-Y et al (2008) Clinical features and mismatch repair genes analyses of Chinese suspected hereditary non-polyposis colorectal cancer: a cost-effective screening strategy proposal. Cancer Sci 99:770–780
Julie C, Tresallet C, Brouquet A et al (2008) Identification in daily practice of patients with Lynch syndrome (hereditary nonpolyposis colorectal cancer): revised Bethesda guidelines-based approach versus molecular screening. Am J Gastroenterol 103:2825–2835
Balmaña J, Balaguer F, CastellvÃBel S et al (2008) Comparison of predictive models, clinical criteria and molecular tumour screening for the identification of patients with Lynch syndrome in a population-based cohort of colorectal cancer patients. J Med Genet 45:557–563
Hampel H, Frankel WL, Martin E et al (2008) Feasibility of screening for Lynch syndrome among patients with colorectal cancer. J ClinOncol 26:5783–5788
Green RC, Parfrey PS, Woods MO et al (2009) Prediction of Lynch syndrome in consecutive patients with colorectal cancer. J Natl Cancer Inst 101:331–340
Molaei M, Mansoori BK, Ghiasi S et al (2010) Colorectal cancer in Iran: immunohistochemical profiles of four mismatch repair proteins. Int J Colorectal Dis 25:63–69
Berginc G, Bracko M, Ravnik-Glavac M et al (2009) Screening for germline mutations of MLH1, MSH2, MSH6 and PMS2 genes in Slovenian colorectal cancer patients: implications for a population specific detection strategy of Lynch syndrome. Fam Cancer 8:421–429
Leite SMO, Gomes KB, Pardini VC et al (2010) Assessment of microsatellite instability in colorectal cancer patients from Brazil. MolBiol Rep 37:375–380
Woods MO, Younghusband HB, Parfrey PS et al (2010) The genetic basis of colorectal cancer in a population-based incident cohort with a high rate of familial disease. Gut 59:1369–1377
Jensen LH, Dysager L, Lindebjerg J et al (2010) Molecular biology from bench-to-bedside - which colorectal cancer patients should be referred for genetic counselling and risk assessment. Eur J Cancer 46:1823–1828
Trano G, Sjursen W, Wasmuth HH et al (2010) Performance of clinical guidelines compared with molecular tumour screening methods in identifying possible Lynch syndrome among colorectal cancer patients: a Norwegian population-based study. Br J Cancer 102:482–488
Minoo P, Zlobec I, Peterson M et al (2010) Characterization of rectal, proximal and distal colon cancers based on clinicopathological, molecular and protein profiles. Int J Oncol 37:707–718
Chang S-C, Lin P-C, Yang S-H et al (2010) Taiwan hospital-based detection of Lynch syndrome distinguishes 2 types of microsatellite instabilities in colorectal cancers. Surgery 147:720–728
Koehler-Santos P, Izetti P, Abud J et al (2011) Identification of patients at-risk for Lynch syndrome in a hospital-based colorectal surgery clinic. World J Gastroenterol 17:766–773
Kaur G, Masoud A, Raihan N et al (2011) Mismatch repair genes expression defects & association with clinicopathological characteristics in colorectal carcinoma. Indian J Med Res 134:186–192
Egoavil CM, Montenegro P, Soto JL et al (2011) Clinically important molecular features of Peruvian colorectal tumours: high prevalence of DNA mismatch repair deficiency and low incidence of KRAS mutations. Pathology 43:228–233
Morrison J, Bronner M, Leach BH et al (2011) Lynch syndrome screening in newly diagnosed colorectal cancer in general pathology practice: from the revised Bethesda guidelines to a universal approach. Scand J Gastroenterol 46:1340–1348
Mojtahed A, Schrijver I, Ford JM et al (2011) A two-antibody mismatch repair protein immunohistochemistry screening approach for colorectal carcinomas, skin sebaceous tumors, and gynecologic tract carcinomas. Mod Pathol 24:1004–1014
Moreira L, Balaguer F, Lindor N et al (2012) Identification of Lynch syndrome among patients with colorectal cancer. JAMA 308:1555–1565
Urso E, Agostini M, Pucciarelli S et al (2012) Clinical and molecular detection of inherited colorectal cancers in northeast Italy: a first prospective study of incidence of Lynch syndrome and MUTYH-related colorectal cancer in Italy. TumourBiol 33:857–864
Merok MA, Ahlquist T, Royrvik EC et al (2013) Microsatellite instability has a positive prognostic impact on stage II colorectal cancer after complete resection: results from a large, consecutive Norwegian series. Ann Oncol 24:1274–1282
Perez-Carbonell L, Ruiz-Ponte C, Guarinos C et al (2012) Comparison between universal molecular screening for Lynch syndrome and revised Bethesda guidelines in a large population-based cohort of patients with colorectal cancer. Gut 61:865–872
Fadhil W, Ibrahem S, Seth R et al (2012) The utility of diagnostic biopsy specimens for predictive molecular testing in colorectal cancer. Histopathology 61:1117–1124
Raskin L, Dakubo JCB, Palaski N et al (2013) Distinct molecular features of colorectal cancer in Ghana. Cancer Epidemiol 37:556–561
Kheirelseid EAH, Miller N, Chang KH et al (2013) Mismatch repair protein expression in colorectal cancer. Journal of Gastrointestinal Oncology 4:397–408
Terui H, Tachikawa T, Kakuta M et al (2013) Molecular and clinical characteristics of MSH6 germline variants detected in colorectal cancer patients. Oncol Rep 30:2909–2916
Vergouwe F, Boutall A, Stupart D et al (2013) Mismatch repair deficiency in colorectal cancer patients in a low-incidence area. S Afr J Surg 51:16–21
Aissi S, Buisine MP, Zerimech F et al (2013) Somatic molecular changes and histo-pathological features of colorectal cancer in Tunisia. World J Gastroenterol 19:5286–5294
Kamat N, Khidhir MA, Alashari MM et al (2013) Microsatellite instability and loss of heterozygosity detected in middle-aged patients with sporadic colon cancer: A retrospective study. Oncology Letters 6:1413–1420
Heald B, Plesec T, Liu X et al (2013) Implementation of universal microsatellite instability and immunohistochemistry screening for diagnosing lynch syndrome in a large academic medical center. J ClinOncol 31:1336–1340
Hartman DJ, Brand RE, Hu H et al (2013) Lynch syndrome-associated colorectal carcinoma: frequent involvement of the left colon and rectum and late-onset presentation supports a universal screening approach. Hum Pathol 44:2518–2528
Marquez E, Geng Z, Pass S et al (2013) Implementation of routine screening for Lynch syndrome in university and safety-net health system settings: successes and challenges. Genetics in Medicine 15:925–932
Aparicio T, Schischmanoff O, Poupardin C et al (2014) High prevalence of deficient mismatch repair phenotype and the V600E BRAF mutation in elderly patients with colorectal cancer. Journal of Geriatric Oncology 5:384–388
Kraus C, Rau TT, Lux P et al (2014) Comprehensive screening for mutations associated with colorectal cancer in unselected cases reveals penetrant and nonpenetrant mutations. Int J Cancer 136:E559
Raman R, Kotapalli V, Adduri R et al (2014) Evidence for possible non-canonical pathway(s) driven early-onset colorectal cancer in India. MolCarcinog 53:E181–E186
Mokarram P, Rismanchi M, AlizadehNaeeni M et al (2014) Microsatellite instability typing in serum and tissue of patients with colorectal cancer: comparing real time PCR with hybridization probe and high-performance liquid chromatography. MolBiol Rep 41:2835–2844
Choi YJ, Kim MS, An CH et al (2014) Regional bias of intratumoral genetic heterogeneity of nucleotide repeats in colon cancers with microsatellite instability. PatholOncol Res 20:965–971
Musulén E, Sanz C, Muñoz-Mármol AM et al (2014) Mismatch repair protein immunohistochemistry: a useful population screening strategy for Lynch syndrome. Hum Pathol 45:1388–1396
Waldmann E, Ferlitsch M, Binder N et al (2015) Tumor and patient characteristics of individuals with mismatch repair deficient colorectal cancer. Digestion 91:286–293
Siraj AK, Prabhakaran S, Bavi P et al (2015) Prevalence of Lynch syndrome in a Middle Eastern population with colorectal cancer. Cancer 121:1762–1771
Korphaisarn K, Pongpaibul A, Limwongse C et al (2015) Deficient DNA mismatch repair is associated with favorable prognosis in Thai patients with sporadic colorectal cancer. World J Gastroenterol 21:926–934
Colling R, Church DN, Carmichael J et al (2015) Screening for Lynch syndrome and referral to clinical genetics by selective mismatch repair protein immunohistochemistry testing: an audit and cost analysis. J ClinPathol 68:1036–1039
Hill AL, Sumra KK, Russell MM et al (2015) A single institution experience in compliance with universal screening for Lynch syndrome in colorectal cancer. J GastrointestSurg 19:543–550
Kidambi TD, Blanco A, Myers M et al (2015) Selective versus universal screening for Lynch syndrome: a six-year clinical experience. Dig Dis Sci 60:2463–2469
Kim YB, Lee S-Y, Kim JH et al (2016) Microsatellite instability of gastric and colorectal cancers as a predictor of synchronous gastric or colorectal neoplasms. Gut Liver 10:220–227
Zumstein V, Vinzens F, Zettl A et al (2016) Systematic immunohistochemical screening for Lynch syndrome in colorectal cancer: a single centre experience of 486 patients. Swiss Med Week 146:w14315
Berera S, Koru-Sengul T, Miao F et al (2016) Colorectal tumors from different racial and ethnic minorities have similar rates of mismatch repair deficiency. ClinGastroenterolHepatol 14:1163–1171
Erten MZ, Fernandez LP, Ng HK et al (2016) Universal versus targeted Sscreening for Lynch syndrome: comparing ascertainment and costs based on clinical experience. Dig Dis Sci 61:2887–2895
Brennan B, Hemmings CT, Clark I et al (2017) Universal molecular screening does not effectively detect Lynch syndrome in clinical practice. TherapeutAdvGastroenterol 10:361–371
Buchanan DD, Clendenning M, Rosty C et al (2017) Tumor testing to identify lynch syndrome in two Australian colorectal cancer cohorts. J GastroenterolHepatol 32:427–438
Haraldsdottir S, Rafnar T, Frankel WL et al (2017) Comprehensive population-wide analysis of Lynch syndrome in Iceland reveals founder mutations in MSH6 and PMS2. Nat Commun 8:14755
Gandhi JS, Goswami M, Sharma A et al (2017) Clinical impact of mismatch repair protein testing on outcome of early staged colorectal carcinomas. J Gastrointest Cancer 49:406
Goshayeshi L, Khooiee A, Ghaffarzadegan K et al (2017) Screening for Lynch syndrome in cases with colorectal carcinoma from Mashhad. Arch Iran Med 20:332–337
O’Kane GM, Ryan Ã, McVeigh TP et al (2017) Screening for mismatch repair deficiency in colorectal cancer: data from three academic medical centers. Cancer Med 6:1465–1472
Abu Freha N, LeiboviciWeissman Y, Fich A et al (2017) Constitutional mismatch repair deficiency and Lynch syndrome among consecutive Arab Bedouins with colorectal cancer in Israel. Fam Cancer 17:79
Fujiyoshi K, Yamaguchi T, Kakuta M et al (2017) Predictive model for high-frequency microsatellite instability in colorectal cancer patients over 50 years of age. Cancer Med 6:1255–1263
Chika N, Eguchi H, Kumamoto K et al (2017) Prevalence of Lynch syndrome and Lynch-like syndrome among patients with colorectal cancer in a Japanese hospital-based population. Jpn J ClinOncol 47:191
Irabor DO, Oluwasola OA, Ogunbiyi OJ et al (2017) Microsatellite instability is common in colorectal cancer in native Nigerians. Anticancer Res 37:2649–2654
Hashmi AA, Ali R, Hussain ZF et al (2017) Mismatch repair deficiency screening in colorectal carcinoma by a four-antibody immunohistochemical panel in Pakistani population and its correlation with histopathological parameters. World J SurgOncol 15:116
Yurgelun MB, Kulke MH, Fuchs CS et al (2017) Cancer susceptibility gene mutations in individuals with colorectal cancer. J ClinOncol 35:1086–1095
Hunter JE, Arnold KA, Cook JE et al (2017) Universal screening for Lynch syndrome among patients with colorectal cancer: patient perspectives on screening and sharing results with at-risk relatives. Fam Cancer 16:377–387
Adar T, Rodgers LH, Shannon KM et al (2017) A tailored approach to BRAF and MLH1 methylation testing in a universal screening program for Lynch syndrome. Mod Pathol 30:440–447
Black D, Soslow RA, Levine DA et al (2006) Clinicopathologic significance of defective DNA mismatch repair in endometrial carcinoma. J ClinOncol 24:1745–1753
Hampel H, Frankel W, Panescu J et al (2006) Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients. Can Res 66:7810–7817
Devlin LA, Graham CA, Price JH et al (2008) Germline MSH6 mutations are more prevalent in endometrial cancer patient cohorts than Hereditary Non Polyposis Colorectal Cancer cohorts. Ulster Med J 77:25–30
Choi YD, Choi J, Kim JH et al (2008) Microsatellite instability at a tetranucleotide repeat in type I endometrial carcinoma. J ExpClin Cancer Res 27:88
Backes FJ, Leon ME, Ivanov I et al (2009) Prospective evaluation of DNA mismatch repair protein expression in primary endometrial cancer. GynecolOncol 114:486–490
Djordjevic B, Barkoh BA, Luthra R et al (2013) Relationship between PTEN, DNA mismatch repair, and tumor histotype in endometrial carcinoma: retained positive expression of PTEN preferentially identifies sporadic non-endometrioid carcinomas. Mod Pathol 26:1401–1412
Egoavil C, Alenda C, Castillejo A et al (2013) Prevalence of Lynch syndrome among patients with newly diagnosed endometrial cancers. PLoS ONE 8:e79737
Batte BAL, Bruegl AS, Daniels MS et al (2014) Consequences of universal MSI/IHC in screening ENDOMETRIAL cancer patients for Lynch syndrome. GynecolOncol 134:319–325
Bruegl AS, Djordjevic B, Batte B et al (2014) Evaluation of clinical criteria for the identification of Lynch syndrome among unselected patients with endometrial cancer. CancerPrev Res 7:686–697
Ferguson SE, Aronson M, Pollett A et al (2014) Performance characteristics of screening strategies for Lynch syndrome in unselected women with newly diagnosed endometrial cancer who have undergone universal germline mutation testing. Cancer 120:3932–3939
Frolova AI, Babb SA, Zantow E et al (2015) Impact of an immunohistochemistry-based universal screening protocol for Lynch syndrome in endometrial cancer on genetic counseling and testing. GynecolOncol 137:7–13
Mills AM, Liou S, Ford JM et al (2014) Lynch syndrome screening should be considered for all patients with newly diagnosed endometrial cancer. Am J SurgPathol 38:1501–1509
McConechy MK, Talhouk A, Li-Chang HH et al (2015) Detection of DNA mismatch repair (MMR) deficiencies by immunohistochemistry can effectively diagnose the microsatellite instability (MSI) phenotype in endometrial carcinomas. GynecolOncol 137:306–310
Goverde A, Spaander MC, van Doorn HC et al (2016) Cost-effectiveness of routine screening for Lynch syndrome in endometrial cancer patients up to 70 years of age. GynecolOncol 143:453–459
Mills AM, Sloan EA, Thomas M et al (2016) Clinicopathologic comparison of Lynch syndrome-associated and “Lynch-like” endometrial carcinomas identified on universal screening using mismatch repair protein immunohistochemistry. Am J SurgPathol 40:155–165
Bruegl A, Daniels M, Broaddus RR (2017) Does universal tissue testing provide universal answers? Clinical challenges associated with tumor screening for lynch syndrome associated endometrial cancer. Lab Invest 97:277A
Cosgrove CM, Backes FJ, Hampel H et al (2017) A single institution pilot study for universal Lynch syndrome screening: a key step towards statewide screening and care. GynecolOncol 145:136
Crim AK, Perkins VB, Husain S et al (2017) Feasibility of two-antibody vs four-antibody mismatch repair protein immunohistochemistry as initial screening for Lynch syndrome in patients with endometrial adenocarcinoma. GynecolOncol 145:44
Najdawi F, Crook A, Maidens J et al (2017) Lessons learnt from implementation of a Lynch syndrome screening program for patients with gynaecological malignancy. Pathology 49:457
Watkins JC, Yang EJ, Muto MG et al (2017) Universal screening for mismatch-repair deficiency in endometrial cancers to identify patients with Lynch syndrome and Lynch-like syndrome. Int J GynecolPathol 36:115–127
Aysal A, Karnezis A, Medhi I et al (2012) Ovarian endometrioid adenocarcinoma: incidence and clinical significance of the morphologic and immunohistochemical markers of mismatch repair protein defects and tumor microsatellite instability. Am J SurgPathol 36:163–172
Pal T, Akbari MR, Sun P et al (2012) Frequency of mutations in mismatch repair genes in a population-based study of women with ovarian cancer. Br J Cancer 107:1783–1790
Chui MH, Ryan P, Radigan J et al (2014) The histomorphology of Lynch syndrome-associated ovarian carcinomas: toward a subtype-specific screening strategy. Am J SurgPathol 38:1173–1181
Lee J-H, Cragun D, Thompson Z et al (2014) Association between IHC and MSI testing to identify mismatch repair-deficient patients with ovarian cancer. Genet Test MolBiomark 18:229–235
Vierkoetter KR, Ayabe AR, VanDrunen M et al (2014) Lynch Syndrome in patients with clear cell and endometrioid cancers of the ovary. GynecolOncol 135:81–84
Rambau PF, Duggan MA, Ghatage P et al (2016) Significant frequency of MSH2/MSH6 abnormality in ovarian endometrioid carcinoma supports histotype-specific Lynch syndrome screening in ovarian carcinomas. Histopathology 69:288–297
Mongiat-Artus P, Miquel C, Van der Aa M et al (2006) Microsatellite instability and mutation analysis of candidate genes in urothelial cell carcinomas of upper urinary tract. Oncogene 25:2113–2118
Giedl J, Schneckenpointner R, Filbeck T et al (2014) Low frequency of HNPCC-associated microsatellite instability and aberrant MMR protein expression in early-onset bladder cancer. Am J ClinPathol 142:634–639
Morales-Burgos A, Sanchez JL, Figueroa LD et al (2008) MSH-2 and MLH-1 protein expression in Muir Torre syndrome-related and sporadic sebaceous neoplasms. P R Health Sci J 27:322–327
Archer-Dubon C, Alvarez-Zavala B, Reyes E et al (2008) Immunohistochemistry screening of sebaceous lesions for Muir-Torre syndrome in a 26-year period in a Mexican population. Dermatol Online J 14:1
Orta L, Klimstra DS, Qin J et al (2009) Towards identification of hereditary DNA mismatch repair deficiency: sebaceous neoplasm warrants routine immunohistochemical screening regardless of patient’s age or other clinical characteristics. Am J SurgPathol 33:934–944
Roberts ME, Riegert-Johnson DL, Thomas BC et al (2013) Screening for Muir-Torre syndrome using mismatch repair protein immunohistochemistry of sebaceous neoplasms. J Genet Counsel 22:393–405
Everett JN, Raymond VM, Dandapani M et al (2014) Screening for germline mismatch repair mutations following diagnosis of sebaceous neoplasm. JAMA Dermatol 150:1315–1321
Boennelycke M, Thomsen BM, Holck S (2015) Sebaceous neoplasms and the immunoprofile of mismatch-repair proteins as a screening target for syndromic cases. Pathol Res Pract 211:78–82
Jessup CJ, Redston M, Tilton E et al (2016) Importance of universal mismatch repair protein immunohistochemistry in patients with sebaceous neoplasia as an initial screening tool for Muir-Torre syndrome. Hum Pathol 49:1–9
Funding
Supported by NIH Grant P50CA62924.
Author information
Authors and Affiliations
Contributions
GKJ and FG were responsible for study concept. GKJ and CCN designed search strategy. GKJ and VV were responsible for screening manuscripts and extracting data. GKJ performed statistical analysis. All authors were involved in critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial, professional, or personal conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kunnackal John, G., Das Villgran, V., Caufield-Noll, C. et al. Comparison of universal screening in major lynch-associated tumors: a systematic review of literature. Familial Cancer 21, 57–67 (2022). https://doi.org/10.1007/s10689-020-00226-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-020-00226-w