Abstract
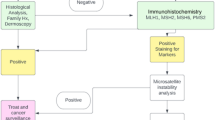
Muir–Torre syndrome (MTS) is clinically characterized by the occurrence of skin, usually sebaceous, and visceral tumors in the same individual. The most common underlying mechanism is a constitutional defect of the mismatch repair (MMR) genes that cause Lynch syndrome (LS). Herewithin we report on a 76 years-old male patient heterozygous for a pathogenic MSH2 missense substitution who presented with a striking cutaneous phenotype in the absence of typical LS visceral tumors. The patient developed 20 skin tumors, including sebaceous adenomas/carcinomas and keratoacanthomas. Two skin tumors showed immunohistochemical loss of MSH2 and MSH6 expression. There was no apparent family history of neoplasia. Based on the variable involvement of the skin and internal organs, we suggest that the definition of tumor associations that are often observed as variants of inherited tumor syndromes, such as MTS, should be guided by the underlying molecular bases. In addition, the presence of multiple sebaceous tumors, especially if showing MMR deficiency, appears to be a very strong indicator of a constitutional MMR gene defect. The reasons underlying the high phenotypic variability of cutaneous phenotypes associated with constitutional MMR defects are yet to be determined.



Similar content being viewed by others
References
Muir EG, Bell AJ, Barlow KA (1967) Multiple primary carcinomata of the colon, duodenum, and larynx associated with keratoacanthomata of the face. Br J Surg 54:191–195
Torre D (1968) Multiple sebaceous tumors. Arch Dermatol 98:549–551
Adan F, Crijns MB, Zandstra WSE, Bekkenk MW, Bleeker FE, Dekker E, van Leerdam ME (2018) Cumulative risk of skin tumours in patients with Lynch syndrome. Br J Dermatol 179(2):522–523. https://doi.org/10.1111/bjd.16552
Akhtar S, Oza KK, Khan SA, Wright J (1999) Muir-Torre syndrome: case report of a patient with concurrent jejunal and ureteral cancer and a review of the literature. J Am Acad Dermatol 41:681–686
Bhaijee F, Brown AS (2014) Muir-Torre syndrome. Arch Pathol Lab Med 138:1685–1689. https://doi.org/10.5858/arpa.2013-0301-RS
Cohen PR, Kohn SR, Kurzrock R (1991) Association of sebaceous gland tumors and internal malignancy: the Muir-Torre syndrome. Am J Med 90:606–613
Ponti G, Ponz de Leon M (2005) Muir-Torre syndrome. Lancet Oncol 6:980–987. https://doi.org/10.1016/S1470-2045(05)70465-4
John AM, Schwartz RA (2016) Muir-Torre syndrome (MTS): an update and approach to diagnosis and management. J Am Acad Dermatol 74:558–566. https://doi.org/10.1016/j.jaad.2015.09.074
South CD, Hampel H, Comeras I, Westman JA, Frankel WL, de la Chapelle A (2008) The frequency of Muir-Torre syndrome among Lynch Syndrome families. J Natl Cancer Inst 100:277–281. https://doi.org/10.1093/jnci/djm291
Schon K, Ritina E, Drummond J, Simmonds J, Anns S, Sandford R, Tischkowitz M (2018) Evaluation of universal immunohistochemical screening of sebaceous neoplasms in a service setting. Clin Exp Dermatol 43:410–415. https://doi.org/10.1111/ced.13359
Kruse R, Rütten A, Lamberti C, Hosseiny-Malayeri HR, Wang Y, Ruelfs C, Jungck M, Mathiak M, Ruzicka T, Hartschuh W, Bisceglia M, Friedl W, Propping P (1998) Muir-Torre phenotype has a frequency of DNA mismatch-repair-gene mutations similar to that in hereditary nonpolyposis colorectal cancer families defined by the Amsterdam criteria. Am J Hum Genet 63:63–70. https://doi.org/10.1086/301926
Plon SE, Eccles DM, Easton D, Foulkes WD, Genuardi M, Greenblatt MS, Hogervorst FB, Hoogerbrugge N, Spurdle AB, Tavtigian SV, IARC Unclassified Genetic Variants Working Group (2008) Sequence variant classification and reporting: recommendations for improving the interpretation of cancer susceptibility genetic test results. Hum Mutat 29:1282–1291. https://doi.org/10.1002/humu.20880
Ryan S, Jenkins MA, Win AK (2014) Risk of prostate cancer in Lynch syndrome: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev 23:437–449. https://doi.org/10.1158/1055-9965.EPI-13-1165
Dominguez-Valentin M, Joost P, Therkildsen C, Jonsson M, Rambech E, Nilbert M (2016) Frequent mismatch-repair defects link prostate cancer to Lynch syndrome. BMC Urol 16:15. https://doi.org/10.1186/s12894-016-0130-1
Haraldsdottir S, Hampel H, Wei L, Wu C, Frankel W, Bekaii-Saab T, de la Chapelle A, Goldberg RM (2014) Prostate cancer incidence in males with Lynch syndrome. Genet Med 16:553–557. https://doi.org/10.1038/gim.2013.193
Engel C, Loeffler M, Steinke V, Rahner N, Holinski-Feder E, Dietmaier W, Schackert HK, Goergens H, von Knebel Doeberitz M, Goecke TO, Schmiegel W, Buettner R, Moeslein G, Letteboer TG, Gómez García E, Hes FJ, Hoogerbrugge N, Menko FH, van Os TA, Sijmons RH, Wagner A, Kluijt I, Propping P, Vasen HF (2012) Risks of less common cancers in proven mutation carriers with Lynch syndrome. J Clin Oncol 30:4409–4415. https://doi.org/10.1200/JCO.2012.43.2278
Vasen HFA, Blanco I, Aktan-Collan K, Gopie JP, Alonso A, Aretz S, Bernstein I, Bertario L, Burn J, Capella G, Colas C, Engel C, Frayling IM, Genuardi M, Heinimann K, Hes FJ, Hodgson SV, Karagiannis JA, Lalloo F, Lindblom A, Mecklin JP, Møller P, Myrhoj T, Nagengast FM, Parc Y, Ponz de Leon M, Renkonen-Sinisalo L, Sampson JR, Stormorken A, Sijmons RH, Tejpar S, Thomas HJW, Rahner N, Wijnen JT, Järvinen HJ, Möslein G, the Mallorca Group (2013) Revised guidelines for the clinical management of Lynch syndrome (HNPCC): recommendations by a group of European experts. Gut 62:812–823. https://doi.org/10.1136/gutjnl-2012-304356
Thompson BA, Spurdle AB, Plazzer JP, Greenblatt MS, Akagi K, Al-Mulla F, Bapat B, Bernstein I, Capellá G, den Dunnen JT, du Sart D, Fabre A, Farrell MP, Farrington SM, Frayling IM, Frebourg T, Goldgar DE, Heinen CD, Holinski-Feder E, Kohonen-Corish M, Robinson KL, Leung SY, Martins A, Moller P, Morak M, Nystrom M, Peltomaki P, Pineda M, Qi M, Ramesar R, Rasmussen LJ, Royer-Pokora B, Scott RJ, Sijmons R, Tavtigian SV, Tops CM, Weber T, Wijnen J, Woods MO, Macrae F, Genuardi M (2014) Application of a 5-tiered scheme for standardized classification of 2,360 unique mismatch repair gene variants in the InSiGHT locus-specific database. Nat Genet 46:107–115. https://doi.org/10.1038/ng.2854
Thompson BA, Goldgar DE, Paterson C, Clendenning M, Walters R, Arnold S, Parsons MT, Michael DW, Gallinger S, Haile RW, Hopper JL, Jenkins MA, Lemarchand L, Lindor NM, Newcomb PA, Thibodeau SN, Registry Colon Cancer Family, Young JP, Buchanan DD, Tavtigian SV, Spurdle AB (2013) A multifactorial likelihood model for MMR gene variant classification incorporating probabilities based on sequence bioinformatics and tumor characteristics: a report from the Colon Cancer Family Registry. Hum Mutat 34:200–209. https://doi.org/10.1002/humu.22213
Roberts ME, Riegert-Johnson DL, Thomas BC, Rumilla KM, Thomas CS, Heckman MG, Purcell JU, Krishna M, Hanson NB, Leppig KA, Lim J, Cappel MA (2014) A clinical scoring system to identify patients with sebaceous neoplasms at risk for the Muir-Torre variant of Lynch syndrome. Genet Med 16:711716. https://doi.org/10.1038/gim.2014.19
Ponti G, Losi L, Pedroni M, Lucci-Cordisco E, Di Gregorio C, Pellacani G, Seidenari S (2006) Value of MLH1 and MSH2 mutations in the appearance of Muir-Torre syndrome phenotype in HNPCC patients presenting sebaceous gland tumors or keratoacanthomas. J Invest Dermatol 126:2302–2307. https://doi.org/10.1038/sj.jid.5700475
Everett MM, Raymond VM, Dandapani M, Marvin M, Kohlmann W, Chittenden A, Koeppe E, Gustafson SL, Else T, Fullen DR, Johnon RM, Syngal S, Gruber SB, Stoffel E (2014) Screening for germline mismatch repair mutations following diagnosis of sebaceous neoplasms. JAMA Dermatol 150:1315–1321. https://doi.org/10.1001/jamadermatol.2014.1217
Lamba AR, Moore AY, Moore T, Rhees J, Arnold MA, Boland CR (2015) Defective DNA mismatch repair activity is common in sebaceous neoplasms, and may be an ineffective approach to screen for Lynch syndrome. Fam Cancer 14:259–264. https://doi.org/10.1007/s10689-015-9782-3
Jessup CJ, Redton M, Tilton E, Reimann JDR (2016) Importance of universal mismatch repair protein immunohistochemistry in patients with sebaceous neoplasia as an initial screening tool for Muir-Torre syndrome. Hum Pathol 49:1–9. https://doi.org/10.1016/j.humpath.2015.10.005
Ponti G, Manfredini M, Tomasi A, Pellacani G (2015) Muir-Torre syndrome and founder mismatch repair gene mutations: a long gone historical genetic challenge. Gene 589:127–132. https://doi.org/10.1016/j.gene.2015.06.078
Ollila S, Sarantaus L, Kariola R, Chan P, Hampel H, Holinski-Feder E, Macrae F, Kohonen-Corish M, Gerdes AM, Peltomäki P, Mangold E, de la Chapelle A, Greenblatt M, Nyström M (2006) Pathogenicity of MSH2 missense mutations is typically associated with impaired repair capability of the mutated protein. Gastroenterology 131:1408–1417. https://doi.org/10.1053/j.gastro.2006.08.044
Rumelt S, Hogan NR, Rubin PA, Jakobiec FA (1998) Four-eyelid sebaceous cell carcinoma following irradiation. Arch Ophthalmol 116:1670–1672
Hood IC, Qizilbash AH, Salama SS, Young JE, Archibald SD (1986) Sebaceous carcinoma of the face following irradiation. Am J Dermatopathol 8:505–508
Lanoy E, Dores GM, Madeleine MM, Toro JR, Fraumeni JF Jr, Engels EA (2009) Epidemiology of nonkeratinocytic skin cancers among persons with AIDS in the United States. AIDS 23:385–393. https://doi.org/10.1097/QAD.0b013e3283213046
Landis MN, Davis CL, Bellus GA, Wolverton SE (2011) Immunosuppression and sebaceous tumors: a confirmed diagnosis of Muir-Torre syndrome unmasked by immunosuppressive therapy. J Am Acad Dermatol 65:1054–1058. https://doi.org/10.1016/j.jaad.2010.08.003
Harwood CA, McGregor JM, Swale VJ, Proby CM, Leigh IM, Newton R, Khorshid SM, Cerio R (2003) High frequency and diversity of cutaneous appendageal tumors in organ transplant recipients. J Am Acad Dermatol 48:401–408. https://doi.org/10.1067/mjd.2003.97
North JP, Golovato J, Vaske CJ, Sanborn JZ, Nuyen A, Wu W, Goode B, Stevers M, McMullen K, Perez White BE, Collisson EA, Bloomer M, Solomon DA, Benz SC, Cho RJ (2018) Cell of origin and mutation pattern define three clinically distinct classes of sebaceous carcinoma. Nat Commun 14:1894. https://doi.org/10.1038/s41467-018-04008-y
Paraf F, Jothy S, Van Meir EG (1997) Brain tumor-polyposis syndrome: two genetic diseases? J Clin Oncol 15:2744–2758
Lynch HT, Lynch PM, Pester J, Fusaro RM (1981) The cancer family syndrome. Rare cutaneous phenotypic linkage of Torre’s syndrome. Arch Intern Med 141:607–611
Acknowledgements
This work was supported by a grant from Università Cattolica del Sacro Cuore (Linea D1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
Informed consent for genetic testing was obtained from the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vaisfeld, A., Calicchia, M., Pomponi, M.G. et al. Lynch syndrome with exclusive skin involvement: time to consider a molecular definition?. Familial Cancer 18, 421–427 (2019). https://doi.org/10.1007/s10689-019-00139-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-019-00139-3