Abstract
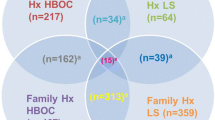
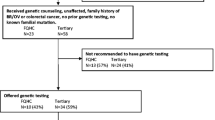
Genetic testing (GT) for inherited cancer predisposition is most informative when initiated in individuals with cancer, thus standard practice recommends GT start in an affected individual. This strategy can be frustrating for unaffected consultands and providers. Retrospective review of cases was performed to compare outcomes of testing the unaffected consultand and recommending that testing start in an affected relative. Records from cancer-free consultands (N = 101), presenting to the University of Michigan Cancer Genetics Clinic between 6/1/2011 and 12/30/2011 were reviewed. All genetics records for these consultands were reviewed through 3/31/2013 for GT recommendations (117 total). The unaffected consultand was offered testing in 14.5 % of cases, testing was completed in 64.7 % of these with one mutation identified. Of consultands tested initially, 70.5 % received cancer-screening recommendations based on family history and test results. Testing was recommended to start in an affected family member in 30.7 % of cases. Fifty percent returned to clinic with information on an affected family member; 83.3 % documented that their family member underwent GT with one mutation identified. Consultands reported the affected family member refused testing in 22.2 % and two of these consultands subsequently pursued GT, identifying one mutation. Fifty percent of cases where testing the family member first was recommended were lost to follow-up with 66.6 % of these never given cancer-screening recommendations. Cancer genetic risk evaluation of healthy consultands should consider the option of pursuing GT in the unaffected consultand and should implement a plan for tailored risk management in the absence of informative genetic evaluation within the family.

Similar content being viewed by others
References
Lindor NM, McMaster ML, Lindor CJ, Greene MH, National Cancer Institute, Division of Cancer Prevention, Community Oncology and Prevention Trials Research Group (2008) Concise handbook of familial cancer susceptibility syndromes—second edition. J Natl Cancer Inst Monogr 38:1–93. doi:10.1093/jncimonographs/lgn001
Robson ME, Storm CD, Weitzel J, Wollins DS, Offit K, American Society of Clinical Oncology (2010) American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol 28(5):893–901. doi:10.1200/JCO.2009.27.0660
Daly MB, Axilbund JE, Buys S, Crawford B, Farrell CD, Friedman S, Garber JE, Goorha S, Gruber SB, Hampel H, Kaklamani V, Kohlmann W, Kurian A, Litton J, Marcom PK, Nussbaum R, Offit K, Pal T, Pasche B, Pilarski R, Reiser G, Shannon KM, Smith JR, Swisher E, Weitzel JN, National Comprehensive Cancer Network (2010) Genetic/familial high-risk assessment: breast and ovarian. J Natl Compr Cancer Netw 8(5):562–594
American Thyroid Association Guidelines Task Force, Kloos RT, Eng C, Evans DB, Francis GL, Gagel RF, Gharib H, Moley JF, Pacini F, Ringel MD, Schlumberger M, Wells SA Jr (2009) Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 19(6):565–612. doi:10.1089/thy.2008.0403
Lindor NM, Peterson GM, Hadley DW, Kinney AY, Miesfeldt S, Lu KH, Lynch P, Burke W, Press N (2006) Recommendations for the care of individuals with an inherited predisposition to Lynch syndrome: a systemic review. JAMA 296(12):1507–1517
Kauff ND, Domcheck SM, Friebel TM, Robson ME, Lee J, Garber JE, Isaacs C, Evans DG, Lynch H, Eeles RA, Neuhausen SL, Daly MB, Matloff E, Blum JL, Sabbatini P, Barakat RR, Hudis C, Norton L, Offit K, Rebbeck TR (2008) Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2- associated breast and gynecologic cancer: a multicenter, prospective study. 26(8):1331–1337. doi:10.1200/JCO.2007.13.9626
Anderson K, Jacobson JS, Heitjan DF, Zivin JG, Hershman D, Neugut AI, Grann VR (2006) Cost-effectiveness of prevention strategies for women with a BRCA1 or a BRCA2 mutation. Ann Intern Med 144(6):397–406
Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group (2009) Recommendations from the EGAPP Working Group: genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives. Genet Med 11(1):35–41. doi:10.1097/GIM.0b013e31818fa2ff
Kontos EZ, Viswanath K (2011) Cancer-related direct-to-consumer advertising: a critical review. Nat Rev Cancer 11(2):142–150. doi:10.1038/nrc2999
Riley BD, Culver JO, Skrzynia C, Senter LA, Peters JA, Costalas JW, Callif-Daley F, Grumet SC, Hunt KS, Nagy RS, McKinnon WC, Petrucelli NM, Bennett RL, Trepanier AM (2012) Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. J Genet Couns 21(2):151–161. doi:10.1007/s10897-011-9462-x
Van Dijk S, Timmermans DR, Meijers-Heijboer H, Tibben A, van Asperen CJ, Otten W (2006) Clinical characteristics affect the impact of an uninformative DNA test result: the course of worry and distress experienced by women who apply for genetic testing for breast cancer. J Clin Oncol 24(22):3672–3677
Dancyger C, Wiseman M, Jacobs C, Smith JA, Wallace M, Michie S (2011) Communicating BRCA1/2 genetic test results within the family: a qualitative analysis. Psychol Health 26(8):1018–1035. doi:10.1080/08870446.2010.525640
Lynch HT, Riley BD, Weissman SM, Coronel SM, Kinarsky Y, Lynch JU, Shaw TG, Rubinstein WS (2004) Hereditary nonpolyposis colorectal carcinoma (HNPCC) and HNPCC-like families: problems in diagnosis, surveillance, and management. Cancer 100(1):53–64
Anderson B, McLosky J, Wasilevich E, Lyon-Callo S, Duquette D, Copeland G (2012) Barriers and facilitators for utilization of genetic counseling and risk assessment services in young female breast cancer survivors. J Cancer Epidemiol 2012:298745. doi:10.1155/2012/298745
O’Neill SM, Peters JA, Vogel VG, Feingold E, Rubinstein WS (2006) Referral to cancer genetic counseling: are there stages of readiness? Am J Med Genet C Semin Med Genet 142C(4):221–231
Cruger DG, Kruse TA, Gerdes AM (2005) ‘Indirect’ BRCA1/2 testing. A useful approach in hereditary breast and ovarian cancer families without a living relative. Clin Genet 68:228–233
Heiniger L, Butow PN, Price MA, Charles M (2013) Distress in unaffected individuals who decline, delay or remain ineligible for genetic testing for hereditary diseases: a systematic review. Psychooncology 22(9):1930–1945
Coates R, Williams M, Melillo S, Gudgeon J (2011) Genetic testing for lynch syndrome in individuals newly diagnosed with colorectal cancer to reduce morbidity and mortality from colorectal cancer in their relatives. PLoS Curr 3:RRN1246. doi:10.1371/currents.RRN1246
Jacobsen PB, Valdimarsdottier HB, Brown KL, Offit K (1997) Decision-making about genetic testing among women at familial risk for breast cancer. Psychosom Med 59(5):459–466
Loescher LJ (2003) Cancer worry in women with hereditary risk factors for breast cancer. Oncol Nurs Forum 30(5):767–772
Katapodi MC, Northouse L, Pierce P, Milliron KJ, Liu G, Merajver SD (2011) Differences between women who pursued genetic testing for hereditary breast and ovarian cancer and their at-risk relatives who did not. Oncol Nurs Forum 38(5):572–581. doi:10.1188/11.ONF.572-281
Van Dijk S, Otten W, Timmermans DR, van Asperen CJ, Meijers-Heijboer H, Tibben A, Breuning MH, Kievit J (2005) What’s the message? Interpretation of an uninformative BRCA1/2 test result for women at risk of familial breast cancer. Genet Med 7(4):239–245
Engel C, Rahner N, Schulmann K, Holinski-Feder E, Goecke TO, Schackert HK, Kloor M, Steinke V, Vogelsang H, Moslein G, Gorgens H, Dechants S, von Knebel Doeberitz M, Ruschoff J, Friedrichs N, Buttner R, Loeffler M, Propping P, Schmiegel W, German HNPCC Consortium (2010) Efficacy of annual colonoscopic surveillance in individuals with hereditary nonpolyposis colorectal cancer. Clin Gastroenterol Hepatol 8(2):174–182. doi:10.1016/j.cgh.2009.10.03
Cott Chubiz JE, Lee JM, Gilmore ME, Kong CY, Lowry KP, Halpern EF, McMahon PM, Ryan PD, Gazelle GC (2013) Cost-effectiveness of alternating magnetic resonance imaging and digital mammography screening in BRCA1 and BRCA2 gene mutation carriers. Cancer 119(6):1266–1276. doi:10.1002/cncr.27864
Acknowledgments
The authors would like to thank all of the patients who consented to participate in longitudinal research with the University of Michigan Cancer Genetics Clinic, especially those included in this assessment (University of Michigan IRB HUM00043440). The authors would also like to express gratitude to Dr. Stephen Gruber for reviewing this paper and contributing to the University of Michigan Cancer Genetics Clinic.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gustafson, S.L., Raymond, V.M., Marvin, M.L. et al. Outcomes of genetic evaluation for hereditary cancer syndromes in unaffected individuals. Familial Cancer 14, 167–174 (2015). https://doi.org/10.1007/s10689-014-9756-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-014-9756-x