Abstract
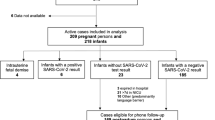
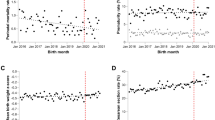
Infections in the first trimester of pregnancy can be teratogenic, but the possibility that Covid-19 could lead to birth defects is unclear. We examined whether SARS-CoV-2 infection during pregnancy or exposure to pandemic conditions were associated with the risk of congenital anomalies. We carried out a retrospective study of 420,222 neonates born in Quebec, Canada in two time periods: prepandemic (January 1, 2017 to March 12, 2020) vs. pandemic (March 13, 2020 to March 31, 2022). We classified pandemic births as early (first trimester completed before the pandemic) or late (first trimester during the pandemic), and identified patients with SARS-CoV-2 infections during pregnancy. We applied (1) adjusted log-binomial regression models to assess the association between SARS-CoV-2 infection and congenital anomalies, and (2) autoregressive interrupted time series regression to analyze temporal trends in the monthly number of defects in all patients regardless of infection. In total, 29,263 newborns (7.0%) had a congenital anomaly. First trimester SARS-CoV-2 infections were not associated with a greater risk of birth defects compared with no infection (RR 1.07, 95% CI 0.59–1.95). However, births during the late pandemic period were more likely to be diagnosed with congenital microcephaly compared with prepandemic births (RR 1.44, 95% CI 1.21–1.71). Interrupted time series analysis confirmed that the frequency of microcephaly increased during the late pandemic period, whereas other anomalies did not. We conclude that Covid-19 is likely not teratogenic, but enhanced surveillance of anomalies among late pandemic births may have heightened the detection of infants with microcephaly.

Similar content being viewed by others
References
Zhang L, Wang X, Liu M, Feng G, Zeng Y, Wang R, et al. The epidemiology and disease burden of congenital TORCH infections among hospitalized children in China: a national cross-sectional study. PLoS Negl Trop Dis. 2022;16:e0010861.
Neu N, Duchon J, Zachariah P. TORCH infections. Clin Perinatol. 2015;42:77–103. viii.
Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects–reviewing the evidence for causality. N Engl J Med. 2016;374:1981–7.
Morris SK, Farrar DS, Miller SP, Ofner M, Bitnun A, Nelson CRM, et al. Population-based surveillance of severe microcephaly and congenital Zika syndrome in Canada. Arch Dis Child. 2021;106:855–61.
Nunez C, Morris A, Jones CA, Badawi N, Baynam G, Hansen M, et al. Microcephaly in Australian children, 2016–2018: national surveillance study. Arch Dis Child. 2021;106:849–54.
Knowles RL, Solebo AL, Sampaio MA, Brown CR, Sargent J, Oluonye N, et al. Incidence, aetiology and neurodisability associated with severe microcephaly: a national surveillance study. Arch Dis Child. 2023;108:211–7.
Khan MSI, Nabeka H, Akbar SMF, Al Mahtab M, Shimokawa T, Islam F, et al. Risk of congenital birth defects during COVID-19 pandemic: draw attention to the physicians and policymakers. J Glob Health. 2020;10:020378.
Heidarzadeh M, Taheri M, Mazaheripour Z, Abbasi-Khameneh F. The incidence of congenital anomalies in newborns before and during the Covid-19 pandemic. Ital J Pediatr. 2022;48:1–5.
Hernández-Díaz S, Smith LH, Wyszynski DF, Rasmussen SA. First trimester COVID-19 and the risk of major congenital malformations-international registry of coronavirus exposure in pregnancy. Birth Defects Res. 2022;114:906–14.
Calvert C, Carruthers J, Denny C, Donaghy J, Hopcroft LEM, Hopkins L, et al. A population-based matched cohort study of major congenital anomalies following COVID-19 vaccination and SARS-CoV-2 infection. Nat Commun. 2023;14:107.
Ministry of Health and Social Services. Med-Echo System Normative Framework - Maintenance and Use of Data for the Study of Hospital Clientele [Internet]. Quebec: Government of Quebec. 2021. https://publications.msss.gouv.qc.ca/msss/fichiers/2000/00-601.pdf.
Auger N, Marcoux S, Bégin P, Lewin A, Lee GE, Healy-Profitós J, et al. Matched cohort study of hospitalization in children who have siblings with cancer. Cancer. 2022;128:1684–91.
Institut national de santé publique du Québec. Timeline of COVID-19 in Quebec [Internet]. [cited 2023 Feb 24]. https://www.inspq.qc.ca/covid-19/donnees/ligne-du-temps.
Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193:E540–8.
DeSilva M, Munoz FM, Mcmillan M, Kawai AT, Marshall H, Macartney KK, et al. Congenital anomalies: case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2016;34:6015–26.
Margulis AV, Setoguchi S, Mittleman MA, Glynn RJ, Dormuth CR, Hernández-Díaz S. Algorithms to estimate the beginning of pregnancy in administrative databases. Pharmacoepidemiol Drug Saf. 2013;22:16–24.
Canadian Institute for Health Information. International statistical classification of diseases and related health problems, tenth revision, Canada (ICD-10-CA): alphabetical index and tabular list. Ottawa, ON: CIHI; 2022.
Auger N, Wei SQ, Dayan N, Ukah UV, Quach C, Lewin A, et al. Impact of Covid-19 on rates of gestational diabetes in a North American pandemic epicenter. Acta Diabetol. 2023;60:257–64.
Sattolo M-L, Arbour L, Bilodeau-Bertrand M, Lee GE, Nelson C, Auger N. Association of birth defects with child mortality before age 14 years. JAMA Netw Open. 2022;5:e226739.
Pampalon R, Hamel D, Gamache P, Simpson A, Philibert MD. Validation of a deprivation index for public health: a complex exercise illustrated by the Quebec index. Chronic Dis Inj Can. 2014;34:12–22.
Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13:S38–44.
Petersen LR, Jamieson DJ, Powers AM, Honein MA. Zika virus. N Engl J Med. 2016;374:1552–63.
Harris SR. Measuring head circumference: update on infant microcephaly. Can Fam Physician. 2015;61:680–4.
Harville EW, Buekens PM, Cafferata ML, Gilboa S, Tomasso G, Tong V. Measurement error, microcephaly prevalence and implications for Zika: an analysis of Uruguay perinatal data. Arch Dis Child. 2020;105:428–32.
Auger N, Quach C, Healy-Profitós J, Lowe A-M, Arbour L. Congenital microcephaly in Quebec: baseline prevalence, risk factors and outcomes in a large cohort of neonates. Arch Dis Child Fetal Neonatal Ed. 2018;103:F167–72.
Barton M, Forrester AM, McDonald J. Update on congenital cytomegalovirus infection: prenatal prevention, newborn diagnosis, and management [Internet]. Canadian Paediatric Society Infectious Diseases and Immunization Committee; 2020 [cited 2023 Aug 28]. https://cps.ca/en/documents/position/update-on-congenital-cytomegalovirus-infection-prenatal-prevention-newborn-diagnosis-and-management.
Sun S, Savitz DA, Wellenius GA. Changes in adverse pregnancy outcomes associated with the COVID-19 pandemic in the United States. JAMA Netw Open. 2021;4:e2129560.
Molina RL, Tsai TC, Dai D, Soto M, Rosenthal N, Orav EJ, et al. Comparison of pregnancy and birth outcomes before vs during the COVID-19 pandemic. JAMA Netw Open. 2022;5:e2226531.
Mendoza M, Garcia-Ruiz I, Maiz N, Rodo C, Garcia‐Manau P, Serrano B, et al. Pre‐eclampsia‐like syndrome induced by severe COVID‐19: a prospective observational study. BJOG. 2020;127:1374–80.
Shook LL, Sullivan EL, Lo JO, Perlis RH, Edlow AG. COVID-19 in pregnancy: implications for fetal brain development. Trends Mol Med. 2022;28:319–30.
Edlow AG, Castro VM, Shook LL, Kaimal AJ, Perlis RH. Neurodevelopmental outcomes at 1 year in infants of mothers who tested positive for SARS-CoV-2 during pregnancy. JAMA Netw Open. 2022;5:e2215787.
Funding
This work was supported by the Canadian Institutes of Health Research (PUU-177957) and the Fonds de recherche du Québec – Santé (296785).
Author information
Authors and Affiliations
Contributions
NA, ÉB, and JHP conceived and designed the study. ÉB performed the data analysis with input from NA and JHP. All authors helped interpret the results. NA and ÉB drafted the article, and LA, AL, JHP, and TML revised it critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This is an observational study. The institutional review board of the University of Montreal Hospital Centre waived the requirement for an ethics review and informed consent for this study.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Auger, N., Arbour, L., Lewin, A. et al. Congenital anomalies during Covid-19: artifact of surveillance or a real TORCH?. Eur J Epidemiol (2024). https://doi.org/10.1007/s10654-024-01122-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10654-024-01122-8