Abstract
In epidemiology, left-truncated data may bias exposure effect estimates. We analyzed the bias induced by left truncation in estimating breast cancer risk associated with exposure to airborne dioxins. Simulations were run with exposure estimates from a Geographic Information System (GIS)-based metric and considered two hypotheses for historical exposure, three scenarios for intra-individual correlation of annual exposures, and three exposure-effect models. For each correlation/model combination, 500 nested matched case–control studies were simulated and data fitted using a conditional logistic regression model. Bias magnitude was assessed by estimated odds-ratios (ORs) versus theoretical relative risks (TRRs) comparisons. With strong intra-individual correlation and continuous exposure, left truncation overestimated the Beta parameter associated with cumulative dioxin exposure. Versus a theoretical Beta of 4.17, the estimated mean Beta (5%; 95%) was 73.2 (67.7; 78.8) with left-truncated exposure and 4.37 (4.05; 4.66) with lifetime exposure. With exposure categorized in quintiles, the TRR was 2.0, the estimated ORQ5 vs. Q1 2.19 (2.04; 2.33) with truncated exposure versus 2.17 (2.02; 2.32) with lifetime exposure. However, the difference in exposure between Q5 and Q1 was 18× smaller with truncated data, indicating an important overestimation of the dose effect. No intra-individual correlation resulted in effect dilution and statistical power loss. Left truncation induced substantial bias in estimating breast cancer risk associated with exposure with continuous and categorical models. With strong intra-individual exposure correlation, both models detected associations, but categorical models provided better estimates of effect trends. This calls for careful consideration of left truncation-induced bias in interpreting environmental epidemiological data.


Similar content being viewed by others
Availability of data and material
The data are available on request from corresponding author.
Code availability
R software code is available on request from corresponding author.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Rodgers KM, Udesky JO, Rudel RA, Brody JG. Environmental chemicals and breast cancer: an updated review of epidemiological literature informed by biological mechanisms. Environ Res. 2018;160:152–82.
Revich BA, Sotskov IP, Kliuev NA, Brodskiĭ ES, Lipchenko IN, Muzurov IV, et al. [Dioxins in the environment and in the blood and breast milk of residents of the town of Chapayevsk]. Gig Sanit. 2001;6–11.
Dai D, Oyana TJ. Spatial variations in the incidence of breast cancer and potential risks associated with soil dioxin contamination in Midland, Saginaw, and Bay Counties, Michigan, USA. Environ Health. 2008;7:49.
Adami HO, Lipworth L, Titus-Ernstoff L, Hsieh CC, Hanberg A, Ahlborg U, Baron J, Trichopoulos D. Organochlorine compounds and estrogen-related cancers in women. Cancer Causes Control. 1995;6:551–66.
Crump KS, Canady R, Kogevinas M. Meta-analysis of dioxin cancer dose response for three occupational cohorts. Environ Health Perspect. 2003;111:681–7.
Xu J, Ye Y, Huang F, Chen H, Wu H, Huang J, Hu J, Xia D, Wu Y. Association between dioxin and cancer incidence and mortality: a meta-analysis. Sci Rep. 2016;6:38012.
Rudel RA, Ackerman JM, Attfield KR, Brody JG. New exposure biomarkers as tools for breast cancer epidemiology, biomonitoring, and prevention: a systematic approach based on animal evidence. Environ Health Perspect. 2014;122:881–95.
Brown NM, Manzolillo PA, Zhang JX, Wang J, Lamartiniere CA. Prenatal TCDD and predisposition to mammary cancer in the rat. Carcinogenesis. 1998;19:1623–9.
Jenkins S, Rowell C, Wang J, Lamartiniere CA. Prenatal TCDD exposure predisposes for mammary cancer in rats. Reprod Toxicol. 2007;23:391–6.
Fenton SE, Hamm JT, Birnbaum LS, Youngblood GL. Persistent abnormalities in the rat mammary gland following gestational and lactational exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD). Toxicol Sci. 2002;67:63–74.
Lewis BC, Hudgins S, Lewis A, Schorr K, Sommer R, Peterson RE, Flaws JA, Furth PA. In utero and lactational treatment with 2,3,7,8-tetrachlorodibenzo-p-dioxin impairs mammary gland differentiation but does not block the response to exogenous estrogen in the postpubertal female rat. Toxicol Sci. 2001;62:46–53.
Vorderstrasse BA, Cundiff JA, Lawrence BP. Developmental exposure to the potent aryl hydrocarbon receptor agonist 2,3,7,8-tetrachlorodibenzo-p-dioxin Impairs the cell-mediated immune response to infection with influenza a virus, but enhances elements of innate immunity. J Immunotoxicol. 2004;1:103–12.
Birnbaum LS, DeVito MJ. Use of toxic equivalency factors for risk assessment for dioxins and related compounds. Toxicology. 1995;105:391–401.
Clarke MA, Joshu CE. Early life exposures and adult cancer risk. Epidemiol Rev. 2017;39:11–27.
Andersen ZJ, Ravnskjær L, Andersen KK, Loft S, Brandt J, Becker T, Ketzel M, Hertel O, Lynge E, Bräuner EV. Long-term exposure to fine particulate matter and breast cancer incidence in the danish nurse cohort study. Cancer Epidemiol Biomarkers Prev. 2017;26:428–30.
Shmuel S, White AJ, Sandler DP. Residential exposure to vehicular traffic-related air pollution during childhood and breast cancer risk. Environ Res. 2017;159:257–63.
Danjou AMN, Fervers B, Boutron-Ruault M-C, Philip T, Clavel-Chapelon F, Dossus L. Estimated dietary dioxin exposure and breast cancer risk among women from the French E3N prospective cohort. Breast Cancer Res. 2015;17:39.
Flesch-Janys D, Steindorf K, Gurn P, Becher H. Estimation of the cumulated exposure to polychlorinated dibenzo-p-dioxins/furans and standardized mortality ratio analysis of cancer mortality by dose in an occupationally exposed cohort. Environ Health Perspect. 1998;106(Suppl 2):655–62.
Liu R, Nelson DO, Hurley S, Hertz A, Reynolds P. Residential exposure to estrogen disrupting hazardous air pollutants and breast cancer risk: the California Teachers Study. Epidemiology. 2015;26:365–73.
Steenland K, Deddens J, Piacitelli L. Risk assessment for 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) based on an epidemiologic study. Am J Epidemiol. 2001;154:451–8.
Coudon T, Hourani H, Nguyen C, Faure E, Mancini FR, Fervers B, Salizzoni P. Assessment of long-term exposure to airborne dioxin and cadmium concentrations in the Lyon metropolitan area (France). Environ Int. 2018;111:177–90.
Quass U, Fermann M, Bröker G. The European dioxin air emission inventory project–final results. Chemosphere. 2004;54:1319–27.
Applebaum KM, Ray RM, Astrakianakis G, Gao DL, Thomas DB, Christiani DC, LaValley MP, Li W, Checkoway H, Eisen EA. Evidence of a paradoxical relationship between endotoxin and lung cancer after accounting for left truncation in a study of Chinese female textile workers. Occup Environ Med. 2013;70:709–15.
Schisterman EF, Cole SR, Ye A, Platt RW. Accuracy loss due to selection bias in cohort studies with left truncation. Paediatr Perinat Epidemiol. 2013;27:491–502.
Vandenbroucke J, Pearce N. Point: incident exposures, prevalent exposures, and causal inference: does limiting studies to persons who are followed from first exposure onward damage epidemiology? Am J Epidemiol. 2015;182:826–33.
Hazelbag CM, Klungel OH, van Staa TP, de Boer A, Groenwold RHH. Left truncation results in substantial bias of the relation between time-dependent exposures and adverse events. Ann Epidemiol. 2015;25:590–6.
Wacholder S. When measurement errors correlate with truth: surprising effects of nondifferential misclassification. Epidemiology. 1995;6:157–61.
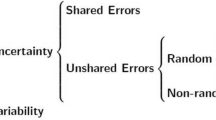
Björk J, Strömberg U. Effects of systematic exposure assessment errors in partially ecologic case-control studies. Int J Epidemiol. 2002;31:154–60.
Goldman GT, Mulholland JA, Russell AG, Srivastava A, Strickland MJ, Klein M, Waller LA, Tolbert PE, Edgerton ES. Ambient air pollutant measurement error: characterization and impacts in a time-series epidemiologic study in Atlanta. Environ Sci Technol. 2010;44:7692–8.
Goldman GT, Mulholland JA, Russell AG, Gass K, Strickland MJ, Tolbert PE. Characterization of ambient air pollution measurement error in a time-series health study using a geostatistical simulation approach. Atmos Environ. 2012;57:101–8.
Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. 2000;108:419–26.
Shy CM, Morgenstern H. the effect of misclassification of exposure status in epidemiological studies of air pollution health effects. Bull N Y Acad Med. 1978;54:11.
Kader GD, Perry M. Variability for categorical variables. J Stat Educ. 2007;15:4.
Richmond-Bryant J, Long TC. Influence of exposure measurement errors on results from epidemiologic studies of different designs. J Expo Sci Environ Epidemiol. 2020;30:420–9.
Goldberg MS, Labrèche F, Weichenthal S, et al. The association between the incidence of postmenopausal breast cancer and concentrations at street-level of nitrogen dioxide and ultrafine particles. Environ Res. 2017;158:7–15.
Leu M, Reilly M, Czene K. Evaluation of bias in familial risk estimates: a study of common cancers using Swedish population-based registers. J Natl Cancer Inst. 2008;100:1318–25.
Applebaum KM, Malloy EJ, Eisen EA. Left truncation, susceptibility, and bias in occupational cohort studies. Epidemiology. 2011;22:599–606.
Cain KC, Harlow SD, Little RJ, Nan B, Yosef M, Taffe JR, Elliott MR. Bias due to left truncation and left censoring in longitudinal studies of developmental and disease processes. Am J Epidemiol. 2011;173:1078–84.
Clavel-Chapelon F, E3N Study Group. Cohort profile: the French E3N cohort study. Int J Epidemiol. 2015;44:801–9.
Riboli E, Hunt KJ, Slimani N, et al. European prospective investigation into cancer and nutrition (EPIC): study populations and data collection. Public Health Nutr. 2002;5:1113–24.
Amadou A, Praud D, Coudon T, et al. Chronic long-term exposure to cadmium air pollution and breast cancer risk in the French E3N cohort. Int J Cancer. 2020;146:341–51.
Danjou AMN, Coudon T, Praud D, et al. Long-term airborne dioxin exposure and breast cancer risk in a case-control study nested within the French E3N prospective cohort. Environ Int. 2019;124:236–48.
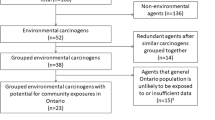
Coudon T, Danjou AMN, Faure E, Praud D, Severi G, Mancini FR, Salizzoni P, Fervers B. Development and performance evaluation of a GIS-based metric to assess exposure to airborne pollutant emissions from industrial sources. Environ Health. 2019;18:8.
Faure E, Danjou AMN, Clavel-Chapelon F, Boutron-Ruault M-C, Dossus L, Fervers B. Accuracy of two geocoding methods for geographic information system-based exposure assessment in epidemiological studies. Environ Health. 2017;16:15.
Hites RA. Dioxins: an overview and history. Environ Sci Technol. 2011;45:16–20.
Pacyna JM, Breivik K, Münch J, Fudala J. European atmospheric emissions of selected persistent organic pollutants, 1970–1995. Atmos Environ. 2003;37:119–31.
Bertolini G. Aperçu historique (jusqu’en 1950) du développement de l’incinération des ordures ménagères dans le monde. Déchets, Sci et Tech. 2000. https://doi.org/10.4267/dechets-sciences-techniques.1351.
Kjeller L-O, Jones KC, Johnston AE, Rappe C. Evidence for a decline in atmospheric emissions of PCDD/Fs in the U.K. Environ Sci Technol. 1996;30:1398–403.
Levy D, Dzikowski C. En 2014, un quart de la population qui déménage change de département. Insee Première. 2017;N.1654:4p.
Binder-Foucard F, Bossard N, Delafosse P, Belot A, Woronoff A-S, Remontet L, et al. Cancer incidence and mortality in France over the 1980-2012 period: solid tumors. Rev Epidemiol Sante Publique. 2014;62:95–108.
Van den Berg M, Birnbaum L, Bosveld AT, et al. Toxic equivalency factors (TEFs) for PCBs, PCDDs, PCDFs for humans and wildlife. Environ Health Perspect. 1998;106:775–92.
Flesch-Janys D, Becher H, Gurn P, Jung D, Konietzko J, Manz A, Päpke O. Elimination of polychlorinated dibenzo-p-dioxins and dibenzofurans in occupationally exposed persons. J Toxicol Environ Health. 1996;47:363–78.
Birnbaum LS, Staskal DF, Diliberto JJ. Health effects of polybrominated dibenzo-p-dioxins (PBDDs) and dibenzofurans (PBDFs). Environ Int. 2003;29:855–60.
Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, et al. Risk factors of breast cancer: a systematic review and meta-analysis. Asia Pac J Public Health. 2013;25:368–87.
Kogevinas M. Human health effects of dioxins: cancer, reproductive and endocrine system effects. Hum Reprod Update. 2001;7:331–9.
Thun MJ, Linet MS, Cerhan JR, Haiman C, Schottenfeld D. Schottenfeld and fraumeni Cancer epidemiology and prevention, fourth edition [Internet]. Fourth. Oxford University Press; 2017 [cited 2020 Feb 20]. Available from: https://mayoclinic.pure.elsevier.com/en/publications/schottenfeld-and-fraumeni-cancer-epidemiology-and-prevention-four.
Roy P, Esteve J. Using relative risk models for estimating synergy between two risk factors. Stat Med. 1998;17:1357–73.
Armstrong BG. Effect of measurement error on epidemiological studies of environmental and occupational exposures. Occup Environ Med. 1998;55:651–6.
Basagaña X, Aguilera I, Rivera M, Agis D, Foraster M, Marrugat J, Elosua R, Künzli N. Measurement error in epidemiologic studies of air pollution based on land-use regression models. Am J Epidemiol. 2013;178:1342–6.
Ayres JG. Trends in air quality in the UK. Allergy. 1997;52:7–13.
Goddard SL, Williams KR, Robins C, Butterfield DM, Brown RJC. Concentration trends of metals in ambient air in the UK: a review. Environ Monit Assess. 2019;191:683.
Nøst TH, Sandanger TM, Nieboer E, Odland JØ, Breivik K. The impacts of emission trends of POPs on human concentration dynamics: Lessons learned from a longitudinal study in Norway (1979–2007). Int J Hyg Environ Health. 2017;220:776–81.
Slama R, Vernet C, Nassan FL, Hauser R, Philippat C. Characterizing the effect of endocrine disruptors on human health: the role of epidemiological cohorts. C R Biol. 2017;340:421–31.
Funding
The study benefited from grants from the French ADEME (Agence de l'Environnement et de la Maîtrise de l'Énergie (Grant No 1306C0031) and the Ligue Contre le Cancer en Saône-et-Loire. The study was also carried out in partnership with Fondation ARC contre le cancer and supported by the project SIRIC (LYRICAN, grant no. INCa-DGOS-INSERM_12563). The first author was supported by SCUSI (Coopérations Scientifiques et Académiques Internationales) and Région Auvergne-Rhône-Alpes via Université de Lyon and the Cancéropôle Lyon Auvergne Rhône-Alpes (CLARA) / Shanghai Health Project: strengthening of the scientific cooperation regarding domains of regional excellence. The nineth author was supported by an academic doctoral fellowship from École Doctorale Interdisciplinaire Sciences-Santé, Université de Lyon.
Author information
Authors and Affiliations
Contributions
Study design: BF, PR, YZ. Data provision: DP, EF, GS, FM, TC. Data analysis: YZ, PR, CM. Result interpretation: PR, BF, AA, YZ. Manuscript drafting and revision: YZ, AA, BF, PR, JI.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Ethics approval
This simulation study did not require ethical approval.
Consent to participate
Not applicable.
Consent for publication
All authors agreed to the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhai, Y., Amadou, A., Mercier, C. et al. The impact of left truncation of exposure in environmental case–control studies: evidence from breast cancer risk associated with airborne dioxin. Eur J Epidemiol 37, 79–93 (2022). https://doi.org/10.1007/s10654-021-00776-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-021-00776-y