Abstract
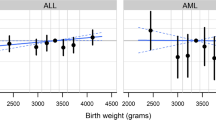
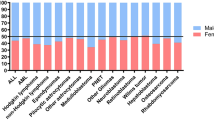
Advanced parental age has been associated with adverse health effects in the offspring including childhood (0–14 years) acute lymphoblastic leukemia (ALL), as reported in our meta-analysis of published studies. We aimed to further explore the association using primary data from 16 studies participating in the Childhood Leukemia International Consortium. Data were contributed by 11 case–control (CC) studies (7919 cases and 12,942 controls recruited via interviews) and five nested case–control (NCC) studies (8801 cases and 29,690 controls identified through record linkage of population-based health registries) with variable enrollment periods (1968–2015). Five-year paternal and maternal age increments were introduced in two meta-analyses by study design using adjusted odds ratios (OR) derived from each study. Increased paternal age was associated with greater ALL risk in the offspring (ORCC 1.05, 95% CI 1.00–1.11; ORNCC 1.04, 95% CI 1.01–1.07). A similar positive association with advanced maternal age was observed only in the NCC results (ORCC 0.99, 95% CI 0.91–1.07, heterogeneity I2 = 58%, p = 0.002; ORNCC 1.05, 95% CI 1.01–1.08). The positive association between parental age and risk of ALL was most marked among children aged 1–5 years and remained unchanged following mutual adjustment for the collinear effect of the paternal and maternal age variables; analyses of the relatively small numbers of discordant paternal-maternal age pairs were not fully enlightening. Our results strengthen the evidence that advanced parental age is associated with increased childhood ALL risk; collinearity of maternal with paternal age complicates causal interpretation. Employing datasets with cytogenetic information may further elucidate involvement of each parental component and clarify underlying mechanisms.


Similar content being viewed by others
References
Steliarova-Foucher E, Colombet M, Ries LAG, Moreno F, Dolya A, Bray F, et al. International incidence of childhood cancer, 2001-10: a population-based registry study. Lancet Oncol. 2017;18(6):719–31. https://doi.org/10.1016/S1470-2045(17)30186-9.
Wiemels J. Perspectives on the causes of childhood leukemia. Chem Biol Interact. 2012;196(3):59–67. https://doi.org/10.1016/j.cbi.2012.01.007.
Metayer C, Milne E, Clavel J, Infante-Rivard C, Petridou E, Taylor M, et al. The Childhood Leukemia International Consortium. Cancer Epidemiol. 2013;37(3):336–47. https://doi.org/10.1016/j.canep.2012.12.011.
Macmahon B, Levy MA. Prenatal origin of Childhood Leukemia. Evidence from Twins. N Engl J Med. 1964;270:1082–5. https://doi.org/10.1056/NEJM196405212702102.
Taub JW, Ge Y. The prenatal origin of childhood acute lymphoblastic leukemia. Leuk Lymphoma. 2004;45(1):19–25.
Gruhn B, Taub JW, Ge Y, Beck JF, Zell R, Hafer R, et al. Prenatal origin of childhood acute lymphoblastic leukemia, association with birth weight and hyperdiploidy. Leukemia. 2008;22(9):1692–7. https://doi.org/10.1038/leu.2008.152.
Milne E, Greenop KR, Metayer C, Schuz J, Petridou E, Pombo-de-Oliveira MS, et al. Fetal growth and childhood acute lymphoblastic leukemia: findings from the childhood leukemia international consortium. Int J Cancer. 2013;133(12):2968–79. https://doi.org/10.1002/ijc.28314.
Rudant J, Lightfoot T, Urayama KY, Petridou E, Dockerty JD, Magnani C, et al. Childhood acute lymphoblastic leukemia and indicators of early immune stimulation: a Childhood Leukemia International Consortium study. Am J Epidemiol. 2015;181(8):549–62. https://doi.org/10.1093/aje/kwu298.
Metayer C, Milne E, Dockerty JD, Clavel J, Pombo-de-Oliveira MS, Wesseling C, et al. Maternal supplementation with folic acid and other vitamins and risk of leukemia in offspring: a Childhood Leukemia International Consortium study. Epidemiology. 2014;25(6):811–22. https://doi.org/10.1097/EDE.0000000000000141.
Thomopoulos TP, Skalkidou A, Dessypris N, Chrousos G, Karalexi MA, Karavasilis TG, et al. Prelabor cesarean delivery and early-onset acute childhood leukemia risk. Eur J Cancer Prev. 2016;25(2):155–61. https://doi.org/10.1097/CEJ.0000000000000151.
Marcotte EL, Thomopoulos TP, Infante-Rivard C, Clavel J, Petridou ET, Schuz J, et al. Caesarean delivery and risk of childhood leukaemia: a pooled analysis from the Childhood Leukemia International Consortium (CLIC). Lancet Haematol. 2016;3(4):e176–85. https://doi.org/10.1016/S2352-3026(16)00002-8.
Kimberly L, Case A, Cheung AP, Sierra S, AlAsiri S, Carranza-Mamane B, et al. Advanced reproductive age and fertility: no. 269, November 2011. Int J Gynaecol Obstet. 2012;117(1):95–102.
Mathews TJ, Hamilton BE. Mean Age of Mothers is on the Rise: United States, 2000–2014. NCHS Data Brief. 2016;232:1–8.
Martin JA, Hamilton BE, Osterman MJ, Curtin SC, Matthews TJ. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65.
Laopaiboon M, Lumbiganon P, Intarut N, Mori R, Ganchimeg T, Vogel JP, et al. Advanced maternal age and pregnancy outcomes: a multicountry assessment. BJOG. 2014;121(Suppl 1):49–56. https://doi.org/10.1111/1471-0528.12659.
Hassold T, Abruzzo M, Adkins K, Griffin D, Merrill M, Millie E et al. Human aneuploidy: incidence, origin, and etiology. Environ Mol Mutagen. 1996;28(3):167–75. https://doi.org/10.1002/(SICI)1098-2280(1996)28:3<167::AID-EM2>3.0.CO;2-B.
Ramasamy R, Chiba K, Butler P, Lamb DJ. Male biological clock: a critical analysis of advanced paternal age. Fertil Steril. 2015;103(6):1402–6. https://doi.org/10.1016/j.fertnstert.2015.03.011.
Kong A, Frigge ML, Masson G, Besenbacher S, Sulem P, Magnusson G, et al. Rate of de novo mutations and the importance of father’s age to disease risk. Nature. 2012;488(7412):471–5. https://doi.org/10.1038/nature11396.
Wong WS, Solomon BD, Bodian DL, Kothiyal P, Eley G, Huddleston KC, et al. New observations on maternal age effect on germline de novo mutations. Nat Commun. 2016;7:10486. https://doi.org/10.1038/ncomms10486.
Adkins RM, Thomas F, Tylavsky FA, Krushkal J. Parental ages and levels of DNA methylation in the newborn are correlated. BMC Med Genet. 2011;12:47. https://doi.org/10.1186/1471-2350-12-47.
Rahbari R, Wuster A, Lindsay SJ, Hardwick RJ, Alexandrov LB, Turki SA, et al. Timing, rates and spectra of human germline mutation. Nat Genet. 2016;48(2):126–33. https://doi.org/10.1038/ng.3469.
Sergentanis TN, Thomopoulos TP, Gialamas SP, Karalexi MA, Biniaris-Georgallis SI, Kontogeorgi E, et al. Risk for childhood leukemia associated with maternal and paternal age. Eur J Epidemiol. 2015;30(12):1229–61. https://doi.org/10.1007/s10654-015-0089-3.
Contreras ZA, Hansen J, Ritz B, Olsen J, Yu F, Heck JE. Parental age and childhood cancer risk: a Danish population-based registry study. Cancer Epidemiol. 2017;49:202–15. https://doi.org/10.1016/j.canep.2017.06.010.
Urhoj SK, Raaschou-Nielsen O, Hansen AV, Mortensen LH, Andersen PK, Nybo Andersen AM. Advanced paternal age and childhood cancer in offspring: a nationwide register-based cohort study. Int J Cancer. 2017;140(11):2461–72. https://doi.org/10.1002/ijc.30677.
Wang R, Metayer C, Morimoto L, Wiemels JL, DeWan AT, Kang A, et al. Parental age and risk of pediatric cancer in the offspring: a population-based record-linkage study in California. Am J Epidemiol. 2017. https://doi.org/10.1093/aje/kwx160.
Marcotte EL, Druley TE, Johnson KJ, Richardson M, von Behren J, Mueller BA, et al. Parental age and risk of infant leukaemia: a pooled analysis. Paediatr Perinat Epidemiol. 2017. https://doi.org/10.1111/ppe.12412.
Schuz J. Non-response bias as a likely cause of the association between young maternal age at the time of delivery and the risk of cancer in the offspring. Paediatr Perinat Epidemiol. 2003;17(1):106–12.
Mateos MK, Barbaric D, Byatt SA, Sutton R, Marshall GM. Down syndrome and leukemia: insights into leukemogenesis and translational targets. Transl Pediatr. 2015;4(2):76–92. https://doi.org/10.3978/j.issn.2224-4336.2015.03.03.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175(1):66–73. https://doi.org/10.1093/aje/kwr265.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–74. https://doi.org/10.7326/M16-2607.
Maule MM, Vizzini L, Merletti F, Magnani C, Pastore G, Richiardi L. Parental age and risk of acute lymphocytic leukaemia and embryonal tumours in the Piedmont Region, Italy. Int J Epidemiol. 2007;36(3):691–2. https://doi.org/10.1093/ije/dym115.
Buka SL, Goldstein JM, Seidman LJ, Tsuang MT. Maternal recall of pregnancy history: accuracy and bias in schizophrenia research. Schizophr Bull. 2000;26(2):335–50.
Karalexi MA, Dessypris N, Thomopoulos TP, Ntouvelis E, Kantzanou M, Diamantaras AA, et al. Parental alcohol consumption and risk of leukemia in the offspring: a systematic review and meta-analysis. Eur J Cancer Prev. 2017;26(5):433–41. https://doi.org/10.1097/CEJ.0000000000000350.
Contreras ZA, Ritz B, Virk J, Cockburn M, Heck JE. Maternal pre-pregnancy and gestational diabetes, obesity, gestational weight gain, and risk of cancer in young children: a population-based study in California. Cancer Causes Control. 2016;27(10):1273–85. https://doi.org/10.1007/s10552-016-0807-5.
Amitay EL, Keinan-Boker L. Breastfeeding and childhood leukemia incidence: a meta-analysis and systematic review. JAMA Pediatr. 2015;169(6):e151025. https://doi.org/10.1001/jamapediatrics.2015.1025.
Pieters R, Schrappe M, De Lorenzo P, Hann I, De Rossi G, Felice M, et al. A treatment protocol for infants younger than 1 year with acute lymphoblastic leukaemia (Interfant-99): an observational study and a multicentre randomised trial. Lancet. 2007;370(9583):240–50. https://doi.org/10.1016/S0140-6736(07)61126-X.
Ross JA, Linabery AM, Blommer CN, Langer EK, Spector LG, Hilden JM, et al. Genetic variants modify susceptibility to leukemia in infants: a Children’s Oncology Group report. Pediatr Blood Cancer. 2013;60(1):31–4. https://doi.org/10.1002/pbc.24131.
Janecka M, Mill J, Basson MA, Goriely A, Spiers H, Reichenberg A, et al. Advanced paternal age effects in neurodevelopmental disorders-review of potential underlying mechanisms. Transl Psychiatry. 2017;7(1):e1019. https://doi.org/10.1038/tp.2016.294.
Merikangas AK, Calkins ME, Bilker WB, Moore TM, Gur RC, Gur RE. Parental age and offspring psychopathology in the Philadelphia Neurodevelopmental Cohort. J Am Acad Child Adolesc Psychiatry. 2017;56(5):391–400. https://doi.org/10.1016/j.jaac.2017.02.004.
McGrath JJ, Petersen L, Agerbo E, Mors O, Mortensen PB, Pedersen CB. A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiatry. 2014;71(3):301–9. https://doi.org/10.1001/jamapsychiatry.2013.4081.
Frans E, MacCabe JH, Reichenberg A. Advancing paternal age and psychiatric disorders. World Psychiatry. 2015;14(1):91–3. https://doi.org/10.1002/wps.20190.
Goriely A, Wilkie AO. Paternal age effect mutations and selfish spermatogonial selection: causes and consequences for human disease. Am J Hum Genet. 2012;90(2):175–200. https://doi.org/10.1016/j.ajhg.2011.12.017.
Mills MB, Hudgins L, Balise RR, Abramson DH, Kleinerman RA. Mutation risk associated with paternal and maternal age in a cohort of retinoblastoma survivors. Hum Genet. 2012;131(7):1115–22. https://doi.org/10.1007/s00439-011-1126-2.
Ferguson-Smith MA, Yates JR. Maternal age specific rates for chromosome aberrations and factors influencing them: report of a collaborative european study on 52 965 amniocenteses. Prenat Diagn. 1984;4 Spec No:5–44.
Miller RW. Relation between cancer and congenital defects in man. N Engl J Med. 1966;275(2):87–93. https://doi.org/10.1056/NEJM196607142750208.
Xavier AC, Taub JW. Acute leukemia in children with down syndrome. Haematologica. 2010;95(7):1043–5. https://doi.org/10.3324/haematol.2010.024968.
Agha MM, Williams JI, Marrett L, To T, Zipursky A, Dodds L. Congenital abnormalities and childhood cancer. Cancer. 2005;103(9):1939–48. https://doi.org/10.1002/cncr.20985.
Carozza SE, Langlois PH, Miller EA, Canfield M. Are children with birth defects at higher risk of childhood cancers? Am J Epidemiol. 2012;175(12):1217–24. https://doi.org/10.1093/aje/kwr470.
Faro R, Santolaya-Forgas J, Oyelese Y, Ananth C. 660: is paternal age a contributing factor for cesarean delivery? A population based study. AJOG Am J Obstetr Gynecol. 2011;204(1):S260–1.
Herstad L, Klungsoyr K, Skjaerven R, Tanbo T, Forsen L, Abyholm T, et al. Elective cesarean section or not? Maternal age and risk of adverse outcomes at term: a population-based registry study of low-risk primiparous women. BMC Pregnancy Childbirth. 2016;16:230. https://doi.org/10.1186/s12884-016-1028-3.
Barrington-Trimis JL, Cockburn M, Metayer C, Gauderman WJ, Wiemels J, McKean-Cowdin R. Trends in childhood leukemia incidence over two decades from 1992 to 2013. Int J Cancer. 2017;140(5):1000–8. https://doi.org/10.1002/ijc.30487.
Shah A, Coleman MP. Increasing incidence of childhood leukaemia: a controversy re-examined. Br J Cancer. 2007;97(7):1009–12. https://doi.org/10.1038/sj.bjc.6603946.
Petridou ET, Dimitrova N, Eser S, Kachanov D, Karakilinc H, Varfolomeeva S, et al. Childhood leukemia and lymphoma: time trends and factors affecting survival in five Southern and Eastern European Cancer Registries. Cancer Causes Control. 2013;24(6):1111–8. https://doi.org/10.1007/s10552-013-0188-y.
Adami HO, Nyren O. Enigmas, priorities and opportunities in cancer epidemiology. Eur J Epidemiol. 2016;31(12):1161–71. https://doi.org/10.1007/s10654-016-0218-7.
Acknowledgements
The CLIC studies thank the families for their consent and participation, the study staff, interviewers and pediatric oncologists for their support as well as Dr Constantinos Mihas and Dr Antonis Analytis for their contributions to statistical analyses. Acknowledgements by study site are shown in the Supplementary materials.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Core Writing Group: Eleni Th. Petridou, Marios K. Georgakis, Friederike Erdmann, Logan G. Spector, Eve Roman, Sameera Ezzat, Ana Maria Mora, Nick Dessypris, Joachim Schüz, Claire Infante-Rivard and Alkistis Skalkidou.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Petridou, E.T., Georgakis, M.K., Erdmann, F. et al. Advanced parental age as risk factor for childhood acute lymphoblastic leukemia: results from studies of the Childhood Leukemia International Consortium. Eur J Epidemiol 33, 965–976 (2018). https://doi.org/10.1007/s10654-018-0402-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-018-0402-z