Abstract
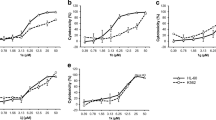
The discovery and development of effective novel compounds is paramount in oncology for improving cancer therapy. In this study, we developed a new derivative of spiroindolone (7’,8’-Dimethoxy-1’,3’-dimethyl-1,2,3’,4’-tetrahydrospiro[indole-3,5’- pyrazolo[3,4-c]isoquinolin]-2-one) and evaluated its anticancer- and immunomodulatory potential in a vitro model of chronic leukemia. We utilized the chronic leukemia cell line K562, as well as non-cancerous peripheral blood mononuclear cells (PBMC) and Vero cells (kidney epithelium of Cercopithecus aethiops). We assessed the cytotoxicity of the compound using the MTT assay, and performed cell cycle assays to determine its impact on different stages of the cell cycle. To evaluate its antineoplastic activity, we conducted a colony formation test to measure the effect of the compound on the clonal growth of cancer cells. Furthermore, we evaluated the immunomodulatory activity of the compound by measuring the levels of pro and anti-inflammatory cytokines. The study findings demonstrate that the spiroindolone-derived compound exerted noteworthy cytotoxic effects against K562 cells, with an IC50 value of 25.27 µg/mL. Additionally, it was observed that the compound inhibited the clonal proliferation of K562 cells while displaying minimal toxicity to normal cells. The compound exhibited its antiproliferative activity by inducing G2/M cell cycle arrest, preventing the entry of K562 cells into mitosis. Notably, the compound demonstrated an immunomodulatory effect by upregulating the production of cytokines IL-6 and IL-12/23p40. In conclusion, the spiroindolone-derived compound evaluated in this study has demonstrated significant potential as a therapeutic agent for the treatment of chronic myeloid leukemia. Further investigations are warranted to explore its clinical applications.





Similar content being viewed by others
Data availability
Data obtained and analyzed in this study are available from the corresponding author upon reasonable request.
References
Wang H, Naghavi M, Allen C et al (2016) Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of Disease Study 2015. Lancet 388:1459. https://doi.org/10.1016/S0140-6736(16)31012-1
Campbell PJ, Martincorena I (2015) Somatic mutation in cancer and normal cells. Science (1979) 349:961–968
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Brown G (2022) Oncogenes and the Origins of Leukemias. Int J Mol Sci 23. https://doi.org/10.3390/IJMS23042293
Minciacchi VR, Kumar R, Krause DS (2021) Chronic myeloid leukemia: a model disease of the past, Present and Future. Cells 10:1–23. https://doi.org/10.3390/CELLS10010117
Zhou T, Medeiros JL, Hu S (2018) Chronic myeloid leukemia: beyond BCR-ABL1. Curr Hematol Malig Rep 13:435–445. https://doi.org/10.37545/haematoljbd20177
Lee H, Basso IN, Kim DDH (2021) Target spectrum of the BCR-ABL tyrosine kinase inhibitors in chronic myeloid leukemia. Int J Hematol 113:632–641. https://doi.org/10.1007/S12185-021-03126-6
Baccarani M, Rosti G, Soverini S (2019) Chronic myeloid leukemia: the concepts of resistance and persistence and the relationship with the BCR-ABL1 transcript type. Leukemia 33:2358–2364. https://doi.org/10.1038/s41375-019-0562-1
Bhamidipati PK, Kantarjian H, Cortes J et al (2013) Management of imatinib-resistant patients with chronic myeloid leukemia. Ther Adv Hematol 4:103–117. https://doi.org/10.1177/2040620712468289
Bouwman SA, Zoleko-Manego R, Renner KC et al (2020) The early preclinical and clinical development of cipargamin (KAE609), a novel antimalarial compound. Travel Med Infect Dis 36:101765. https://doi.org/10.1016/J.TMAID.2020.101765
Altowyan MS, Barakat A, Al-Majid AM, Al-Ghulikah HA (2019) Spiroindolone Analogues as potential hypoglycemic with dual inhibitory activity on α-Amylase and α-Glucosidase. Molecules 24. https://doi.org/10.3390/MOLECULES24122342
Arun Y, Bhaskar G, Balachandran C et al (2013) Facile one-pot synthesis of novel dispirooxindole-pyrrolidine derivatives and their antimicrobial and anticancer activity against A549 human lung adenocarcinoma cancer cell line. Bioorg Med Chem Lett 23:1839–1845. https://doi.org/10.1016/J.BMCL.2013.01.023
Girgis AS (2009) Regioselective synthesis of dispiro[1H-indene-2,3′-pyrrolidine-2′,3″-[3H]indole]-1,2″(1″H)-diones of potential anti-tumor properties. Eur J Med Chem 44:91–100. https://doi.org/10.1016/J.EJMECH.2008.03.013
Sharma P, Kumar A, Sahu V et al (2009) Synthesis of bioactive spiro-2-[3’-(2’-phenyl)-3H-indolyl]-1-aryl-3- phenylaziridines and SAR studies on their antimicrobial behavior. Med Chem Res 18:383–395. https://doi.org/10.1007/S00044-008-9135-Y/FIGURES/1
Ye N, Chen H, Wold EA et al (2016) Therapeutic potential of Spirooxindoles as Antiviral Agents. ACS Infect Dis 2:382. https://doi.org/10.1021/ACSINFECDIS.6B00041
de Oliveira RC, Pontes GS, Kostyuk A et al (2020) Anticancer and immunomodulatory activities of a Novel Water-Soluble Derivative of Ellipticine. Biomolecules 25:1–12
Meyskens FL, Mukhtar H, Rock CL et al (2016) Cancer Prevention: obstacles, Challenges, and the Road ahead. JNCI J Natl Cancer Inst 108. https://doi.org/10.1093/JNCI/DJV309
O’Donnell JS, Teng MWL, Smyth MJ (2019) Cancer immunoediting and resistance to T cell-based immunotherapy. Nat Rev Clin Oncol 16:151–167. https://doi.org/10.1038/s41571-018-0142-8
LEAHY JW, LEWIS GL, NUSS JM et al (2005) ANAPLASTIC LYMPHOMA KINASE MODULATORS AND METHODS OF USE
Lu B, Cao H, Cao J et al (2016) Discovery of EBI-907: a highly potent and orally active B-Raf(V600E) inhibitor for the treatment of melanoma and associated cancers. Bioorg Med Chem Lett 26:819–823. https://doi.org/10.1016/J.BMCL.2015.12.086
Defois M, Rémondin C, Josselin B et al (2022) Synthesis and kinase inhibitory potencies of Pyrazolo[3,4-g]isoquinolines. Molecules 27. https://doi.org/10.3390/MOLECULES27175578
Mortier J, Frederick R, Ganeff C et al (2010) Pyrazolo[4,3-c]isoquinolines as potential inhibitors of NF-κB activation. Biochem Pharmacol 79:1462–1472. https://doi.org/10.1016/J.BCP.2010.01.007
Theivendren P, Kunjiappan S, Hegde YM et al (2021) Importance of protein kinase and its inhibitor: a review. https://doi.org/10.5772/INTECHOPEN.98552
Boni C, Sorio C (2021) Current views on the interplay between Tyrosine Kinases and Phosphatases in Chronic myeloid leukemia. Cancers (Basel) 13. https://doi.org/10.3390/CANCERS13102311
Cilloni D, Saglio G (2012) Molecular pathways: BCR-ABL. Clin Cancer Res 18:930–937. https://doi.org/10.1158/1078-0432.CCR-10-1613/83554/AM/MOLECULAR-PATHWAYS-BCR-ABLBCR-ABL.
Thompson LJ, Fields AP (1996) βII protein kinase C is required for the G2/M phase transition of cell cycle. J Biol Chem 271:15045–15053. https://doi.org/10.1074/JBC.271.25.15045
Wolanin K, Magalska A, Kusio-Kobialka M et al (2010) Expression of oncogenic kinase bcr-abl impairs mitotic checkpoint and promotes aberrant divisions and resistance to microtubule-targeting agents. Mol Cancer Ther 9:1328–1338. https://doi.org/10.1158/1535-7163.MCT-09-0936
Morgan MA, Dolp O, Reuter CWM (2001) Cell-cycle-dependent activation of mitogen-activated protein kinase kinase (MEK-1/2) in myeloid leukemia cell lines and induction of growth inhibition and apoptosis by inhibitors of RAS signaling. Blood 97:1823–1834. https://doi.org/10.1182/BLOOD.V97.6.1823
Feinstein TN, Linstedt AD (2007) Mitogen-activated protein kinase kinase 1-dependent golgi unlinking occurs in G2 phase and promotes the G2/M cell cycle transition. Mol Biol Cell 18:594. https://doi.org/10.1091/MBC.E06-06-0530
Raja UM, Gopal G, Shirley S et al (2017) Immunohistochemical expression and localization of cytokines/chemokines/growth factors in gastric cancer. Cytokine 89:82–90. https://doi.org/10.1016/j.cyto.2016.08.032
Mihara M, Hashizume M, Yoshida H et al (2012) IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci (Lond) 122:143–159. https://doi.org/10.1042/CS20110340
Welner RS, Amabile G, Bararia D et al (2015) Treatment of chronic myelogenous leukemia by blocking cytokine alterations found in normal stem and progenitor cells. Cancer Cell 27:671–681. https://doi.org/10.1016/J.CCELL.2015.04.004
Reynaud D, Pietras E, Barry-Holson K et al (2011) IL-6 controls leukemic multipotent progenitor cell fate and contributes to chronic myelogenous leukemia development. Cancer Cell 20:661. https://doi.org/10.1016/J.CCR.2011.10.012
Fisher DT, Chen Q, Skitzki JJ et al (2011) IL-6 trans-signaling licenses mouse and human tumor microvascular gateways for trafficking of cytotoxic T cells. J Clin Invest 121:3846–3859. https://doi.org/10.1172/JCI44952
Mikucki ME, Fisher DT, Ku AW et al (2013) Preconditioning thermal therapy: flipping the switch on IL-6 for anti-tumour immunity. Int J Hyperthermia 29:464–473. https://doi.org/10.3109/02656736.2013.807440
Mirlekar B, Pylayeva-Gupta Y (2021) IL-12 family cytokines in Cancer and Immunotherapy. Cancers (Basel) 13:1–23. https://doi.org/10.3390/CANCERS13020167
Chen CIU, Koschmieder S, Kerstiens L et al (2012) NK cells are dysfunctional in human chronic myelogenous leukemia before and on imatinib treatment and in BCR-ABL-positive mice. Leukemia 26:465–474. https://doi.org/10.1038/LEU.2011.239
Salih J, Hilpert J, Placke T et al (2010) The BCR/ABL-inhibitors imatinib, nilotinib and dasatinib differentially affect NK cell reactivity. Int J Cancer 127:2119–2128. https://doi.org/10.1002/IJC.25233
Nour el deen RAA, Harfoush RA, Elgharabawy MM et al (2011) Levels of interleukins 12 (IL-12) and 13 (IL-13), hepatitis B and C serology, and blood cultures among acute myeloid leukemia (AML) patients in Egypt. J Venom Anim Toxins including Trop Dis 17:293–299. https://doi.org/10.1590/S1678-91992011000300009
Huang J, Liu Y, Au BC et al (2016) Preclinical validation: LV/IL-12 transduction of patient leukemia cells for immunotherapy of AML. Mol Ther Methods Clin Dev 3:16074. https://doi.org/10.1038/MTM.2016.74
Acknowledgements
Acknowledgments to the Institute of Chemical Institute of Ukraine, to the Horizon2020-MSCA-RISE-2016-734759 project, acronym VAHVISTUS, to the Research Support Foundation of the State of Amazonas (FAPEAM) e to the Hospital Foundation of Hematology and Hemotherapy of the Amazon (FHEMOAM).
Funding
This research was funded by the Research Support Foundation of the State of Amazonas (FAPEAM) (CT&I ÁREAS PRIORITÁRIAS #01.02.016301.03422/2021-03), the Coordination of Improvement of Higher Education Personnel (CAPES) (Finance code—PROCAD AMAZÔNIA 88881.200581/201801) and the Horizon2020-MSCA-RISE-2016-734759 project, acronym VAHVISTUS.
Author information
Authors and Affiliations
Contributions
Carlos Eduardo de C. Alves: project administration, manuscript writing, writing - review and editing, methodology, investigation, data analysis. Serge L. Bogza, Nathalie Bohdan and Alexander B. Rozhenko: compound design and synthesis, manuscript review. Alice de Freitas Gomes: methodology, investigation, formal analysis. Regiane Costa de Oliveira: methodology, investigation, formal analysis, writing - review. Renata Galvão de Azevedo and Larissa Raquel Silva: methodology, investigation, formal analysis. Anamika Dhyani: methodology, investigation, formal analysis, provision of resources for the study. Andriy Grafov: compound design and synthesis, provision of resources for the study. Gemilson Soares Pontes: project administration, conceptualization, funding acquisition, investigation, writing - review and editing, formal analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
All authors declare no conflicts of interest.
Ethics approval
Approval for the utilization of human PBMCs was granted by the Research Ethics Committee (REC) of the Foundation of Hematology and Hemotherapy Foundation of Amazonas State (HEMOAM), Brazil (approval number: 3.138.343; approved on February 8, 2019).
Consent to publish
All authors allowed the submission of the manuscript for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Castro Alves, C.E., Bogza, S.L., Bohdan, N. et al. Pharmacological assessment of the antineoplastic and immunomodulatory properties of a new spiroindolone derivative (7’,8’-Dimethoxy-1’,3’-dimethyl-1,2,3’,4’-tetrahydrospiro[indole-3,5’-pyrazolo[3,4-c]isoquinolin]-2-one) in chronic myeloid leukemia. Invest New Drugs 41, 629–637 (2023). https://doi.org/10.1007/s10637-023-01382-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-023-01382-3