Summary
Through rational drug design, we previously identified an indenoprazole derivative, 2-(6-ethoxy-3-(3-ethoxyphenylamino)-1-methyl-1,4-dihydroindeno[1,2-c]pyrazol-7-yloxy)acetamide (LL01), as a potent tubulin polymerization inhibitor targeting the tubulin colchicine binding site. In this study, we further demonstrated that LL01 was not a P-gp substrate. It potently inhibited the growth of a variety of tumor cells, including those with multidrug resistance, with GI50 values in the low nanomole ranges. In vitro liver microsome stability assay, LL01 was modest stable in the liver microsomes of human, mouse and rat, but was fast metabolized in dog. After single oral administration of LL01 at a dose of 10 mg/kg in SD male rats, LL01 showed acceptable PK properties with a mean bioavailability of 41%. In human HepG2 hepatoma xenograft, at the oral doses of 25 mg/kg/day and 12.5 mg/kg/day, LL01 inhibited the tumor growth by 61.27%, and 43.74%, respectively, which is much better than the positive drug sorafenib (29.45%; 30 mg/kg/day). Therefore, LL01 might be a potential drug candidate for further investigation for hepatocellular carcinoma therapy.



Similar content being viewed by others
References
Heald R, Nogales E (2002) Microtubule dynamics. J Cell Sci 115(1):3–4
McIntosh JR, Grishchuk E, West RR (2002) Chromosome−microtubule interactions during mitosis. Annu Rev Cell Dev Biol 18:193–219
Brouhard GJ, Rice LM (2014) The contribution of αβ-tubulin curvature to microtubule dynamics. J Cell Biol 207(3):323–334
Akhmanova A, Steinmetz MO (2015) Control of microtubule organization and dynamics: two ends in the limelight. Nat Rev Mol Cell Biol 16:711–726
Dumontet C, Jorda MA (2010) Microtubule-binding agents: a dynamic field of cancer therapeutics. Nat Rev Drug Discov 9:790–803
Stanton RA, Gernert KM, Nettles JH, Aneja R (2011) Drugs that target dynamic microtubules: a new molecular perspective. Med Res Rev 31(3):443–481
Prota AE, Bargsten K, Zurwerra D et al (2013) Molecular mechanism of action of microtubule-stabilizing anticancer agents. Science 339(6119):587–590
Vindya NG, Sharma N, Yadav M, Ethiraj KR (2015) Tubulins−the target for anticancer therapy. Curr Top Med Chem 15(1):73–82
Chen H, Lin Z, Arnst KE, Miller DD, Li W (2017) Tubulin inhibitor-based antibody-drug conjugates for cancer therapy. Molecules 22(8):1281
Steinmetz MO, Prota AE (2018) Microtubule-targeting agents: strategies to hijack the cytoskeleton. Trends Cell Biol 28(10):776–792
Dorléans A, Gigant B, Ravelli RBG, Mailliet P, Mikol V, Knossow M (2009) Variations in the colchicine-binding domain provide insight into the structural switch of tubulin. Proc Natl Acad Sci U S A 106(33):13775–13779
Perez EA (2009) Microtubule inhibitors: differentiating tubulin-inhibiting agents based on mechanisms of action, clinical activity, and resistance. Mol Cancer Ther 8(8):2086–2095
Gigant B, Wang C, Ravelli RBG et al (2005) Structural basis for the regulation of tubulin by vinblastine. Nature 435:519–522
Kavallaris M (2010) Microtubules and resistance to tubulin-binding agents. Nat Rev Cancer 10(3):194–204
Du J, Li B, Fang Y et al (2015) Overexpression of class III β-tubulin, sox2, and nuclear survivin is predictive of taxane resistance in patients with stage III ovarian epithelial cancer. BMC Cancer 15:536
Duran GE, Wang YC, Francisco EB et al (2015) Mechanisms of resistance to cabazitaxel. Mol Cancer Ther 14(1):193–201
Stengel C, Newman SP, Leese MP, Potter BV, Reed MJ, Purohit A (2010) Class III beta-tubulin expression and in vitro resistance to microtubule targeting agents. Br J Cancer 102(2):316–324
Karki R, Mariani M, Andreoli M et al (2013) βIII-tubulin: biomarker of taxane resistance or drug target? Expert Opin Ther Targets 17(4):461–472
Wang XF, Xie L (2012) Vascular disrupting agents targeting at tubulin: a novel class of antitumor drug. J Int Pharm Res 39(6):445–454
Liu YM, Chen HL, Lee HY, Liou JP (2014) Tubulin inhibitors: a patent review. Expert Opin Ther Pat 24(1):69–88
Kaur R, Kaur G, Gill RK, Soni R, Bariwal J (2014) Recent developments in tubulin polymerization inhibitors: an overview. Eur J Med Chem 87:89–124
Ji YT, Liu YN, Liu ZP (2015) Tubulin colchicine binding site inhibitors as vascular disrupting agents in clinical developments. Curr Med Chem 22(11):1348–1360
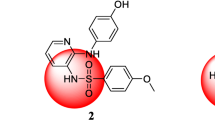
Liu YN, Wang JJ, Ji YT et al (2016) Design, synthesis, and biological evaluation of 1-methyl-1,4-dihydroindeno[1,2-c]pyrazole analogues as potential anticancer agents targeting tubulin colchicine binding site. J Med Chem 59(11):5341–5355
Zhang Y, Gong FL, Lu ZN et al (2017) DHPAC, a novel synthetic microtubule destabilizing agent, possess high anti-tumor activity in vincristine-resistant oral epidermoid carcinoma in vitro and in vivo. Int J Biochem Cell Biol 93:1–11
Manda VK, Avula B, Ali Z et al (2013) Characterization of in vitro ADME properties of diosgenin and dioscin from Dioscorea villosa. Planta Med 79(05):1421–1428
Rueff J, Rodrigues AS (2016) Cancer drug resistance: a brief overview from a genetic view point. Methods Mol Biol 1395:1–18
Barbuti AM, Chen ZS (2015) Paclitaxel through the ages of anticancer therapy: exploring its role in chemoresistance and radiation therapy. Cancers 7:2360–2371
Duan Z, Brakora KA, Seiden MV (2004) Inhibition of ABCB1 (MDR1) and ABCB4 (MDR3) expression by small interfering RNA and reversal of paclitaxel resistance in human ovarian cancer cells. Mol Cancer Ther 3(7):833–838
Kathawala RJ, Sodani K, Chen K et al (2014) Masitinib antagonizes ATP-binding cassette subfamily C member 10-mediated paclitaxel resistance: a preclinical study. Mol Cancer Ther 13(3):714–723
Kavallaris M (2010) Microtubules and resistance to tubulin-binding agents. Nat Rev Cancer 10(3):194–204
Cheng KL, Bradley T, Budman DR (2008) Novel microtubule-targeting agents – the epothilones. Biologics: Targets & Therapy 2(4):789–811
Sampson VB, Vetter NS, Zhang W et al (2016) Integrating mechanisms of response and resistance against the tubulin binding agent Eribulin in preclinical models of osteosarcoma. Oncotarget 7(52):86594–86607
Mangiatordi GF, Trisciuzzi D, Alberga D et al (2017) Novel chemotypes targeting tubulin at the colchicine binding site and unbiasing P-glycoprotein. Eur J Med Chem 139:792–803
Wang Q, Rage JD, Weinstein K et al (2005) Evaluation of the MDR-MDCK cell line as a permeability screen for the blood–brain barrier. Int J Pharm 288(2):349–359
Acharya P, O’Connor MP, Polli JP, Ayrton A, Ellens H, Bentz J (2008) Kinetic identification of membrane transporters that assist P-glycoprotein-mediated transport of digoxin and loperamide through a confluent monolayer of MDCKII-hMDR1 cells. Drug Metab Dispos 36(2):452–460
Houston JB (1994) Utility of in vitro drug metabolism data in predicting in vivo metabolic clearance. Biochem Pharmacol 47(9):1469–1479
Obach RS (1999) Prediction of human clearance of twenty-nine drugs from hepatic microsomal intrinsic clearance data: an examination of in vitro half-life approach and nonspecific binding to microsomes. Drug Metab Dispos 27(11):1350–1359
Riley RJ, McGinnity DF, Austin RP (2005) A unified model for predicting human hepatic, metabolic clearance from in vitro intrinsic clearance data in hepatocytes and microsomes. Drug Metab Dispos 33(9):1304–1311
Barter ZE, Bayliss MK, Beaune PH et al (2007) Scaling factors for the extrapolation of in vivo metabolic drug clearance from in vitro data: reaching a consensus on values of human microsomal protein and hepatocellularity per gram of liver. Curr Drug Metab 8(1):33–45
Flores A, Marrero JA (2014) Emerging trends in hepatocellular carcinoma: focus on diagnosis and therapeutics. Clin Med Insights: Oncol 8(8):71–76
Forner A, Reig M, Bruix J (2018) Hepatocellular carcinoma. Lancet 391(10127):1301–1314
Wilhelm S, Carter C, Lynch M et al (2006) Discovery and development of sorafenib: a multikinase inhibitor for treating cancer. Nat Rev Drug Discov 5(10):835–844
Llovet JM, Ricci S, Mazzaferro V et al (2008) Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 359(4):378–390
Cheng AL, Kang YK, Chen Z et al (2009) Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo controlled trial. Lancet Oncol 10(1):25–34
Heo YA, Syed YY (2018) Regorafenib: a review in hepatocellular carcinoma. Drugs 78(9):951–958
Kudo M, Finn RS, Qin S et al (2018) Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391(10126):1163–1173
Funding
The work was supported by the National Natural Science Foundation of China (NSFC, Grant No. 81573275) and the Key Research and Development Project of Shandong Province (2017CXGC1401), China.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the study. Data were generated and analysed by JDW, YJC, YGZ, LQT, CMZ and ZPL. YJC, YGZ, LQT and CMZ contributed to the design of some of the studies and interpretation of results. JDW, YGZ and ZPL designed the overall study, interpreted all results. JDW wrote the manuscript and ZPL made a revision. All authors reviewed the manuscript for accuracy and contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Author JDW declares that he has no conflict of interest. Author YJC declares that he has no conflict of interest. Author YGZ declares that he has no conflict of interest. Author LQT declares that he has no conflict of interest. Author CMZ declares that she has no conflict of interest. Author ZPL declares that he has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants. The animal experiments were performed under the guidance of the Animal Care and Welfare Committee of Shandong University and followed the principles outlined in the Declaration of Helsinki for animal experimental investigations.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, JD., Cui, YJ., Zhou, YG. et al. Tubulin colchicine site binding agent LL01 displays potent antitumor efficiency both in vitro and in vivo with suitable drug-like properties. Invest New Drugs 38, 29–38 (2020). https://doi.org/10.1007/s10637-019-00753-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-019-00753-z