Summary
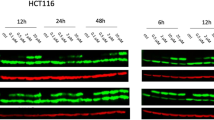
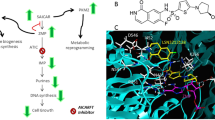
Capecitabine, an orally available prodrug of 5-FU, requires activation by carboxylesterase (CES) enzymes present in the liver to generate 5′-deoxy-5-flurocytidine ribose (5′-DFCR). The deamination of the latter by cytidine deaminase gives 5′-deoxy-5-fluorouridine ribose (5′-DFUR). Finally, the conversion of 5′-DFUR to the cytotoxic drug 5-FU, occurs primarily in the tumour and is catalyzed by thymidine phosphorylase (TP). Accordingly, it was surmised that events associated with an increase of TP levels should enhance the potency of capecitabine and its metabolites. EGFR inhibition was found to be one such event. The observed synergy between gefitinib and 5′-DFUR has inspired the design of single molecules capable of acting as prodrugs of both an EGFR inhibitor and 5-FU. Here, we report on the synthesis and characterization of one such molecule, ZRX1, that consists of an acetylated 5′-DFCR moiety linked to a quinazoline inhibitor of EGFR through an alkyl dicarbamate spacer that requires CES activation to generate the two active metabolites. Our results showed that ZRX1 was ineffective as an intact molecule. However, when CES was present, ZRX1 induced an increase in EGFR inhibition, TP expression, DNA damage and apoptosis. ZRX1 was, at least, 3-fold more potent than capecitabine and 5′-DFUR and recapitulated the effects of the combination treatments. LC-MS analysis showed that in the presence of CES, ZRX1 is metabolized into a mixture of bioactive quinazoline derivatives and 5′-DFCR derived metabolites. Our results in toto, suggest that capecitabine-based EGFR targeting combi-molecules of the same type than ZRX1, have the potential to induce stronger growth inhibitory potency than capecitabine, 5′-DFUR or single EGFR inhibitors and equivalent potency when compared with combinations of EGFR inhibitors + 5′-DFUR.












Similar content being viewed by others
References
Cassata A, Procoplo G, Alu M, Ferrari L, Ferrario E, Beretta E, Longarini R, Busto G, De Candis D, Bajetta E (2001) Capecitabine: indications and future perspectives in the treatment of metastatic colorectal and breast cancer. Tumori 87:364–371
Aprile G, Mazzer M, Moroso S, Puglisi F (2009) Pharmacology and therapeutic efficacy of capecitabine: focus on breast and colorectal cancer. Anticancer Drugs 20(4):217–229
Shimma N, Umeda I, Arasaki M, Murasaki C, Masubuchi K, Kohchi Y, Miwa M, Ura M, Sawada N, Tahara H et al (2000) The design and synthesis of a new tumor-selective fluoropyrimidine carbamate, capecitabine. Bioorg Med Chem 8(7):1697–1706
Miwa M, Ura M, Nishida M, Sawada N, Ishikawa T, Mori K, Shimma N, Umeda I, Ishitsuka H (1998) Design of a novel oral fluoropyrimidine carbamate, capecitabine, which generates 5-fluorouracil selectively in tumours by enzymes concentrated in human liver and cancer tissue. Eur J Cancer 34:1274–1281
Ishitsuka H (2000) Capecitabine: preclinical pharmacology studies. Invest New Drugs 18:343–354
Mimori K, Ueo H, Kuroki T, Shiraishi T, Creer S, Taylor S, Ishii H, Mori M (2004) Prediction of 5′-deoxy-5-fluorouridine sensitivity in colorectal cancer cases by thymidine phosphorylase activity and preliminary identification of susceptibility related genes. Oncol Rep 12(1):19–23
Andreetta C, Puppin C, Minisini A, Valent F, Pegolo E, Damante G, Di Loreto C, Pizzolitto S, Pandolfi M, Fasola G, Piga A, Puglisi F (2009) Thymidine phosphorylase expression and benefit from capecitabine in patients with advanced breast cancer. Ann Oncol 20(2):265–271
O’Neil BH, McLeod HL (2006) Thymidine phosphorylase and capecitabine: a predictive marker for therapy selection? J Clin Oncol 24(25):4051–4053
Sawada N, Ishikawa T, Fukase Y, Nishida M, Yoshikubo T, Ishitsuka H (1998) Induction of thymidine phosphorylase activity and enhancement of capecitabine efficacy by Taxol/Taxotere in human cancer xenografts. Clin Cancer Res 4:1013–1019
Talbot DC, Moiseyenko V, Van Belle S, O’Reilly SM, Alba Conejo E, Ackland S, Eisenberg P, Melnychuk D, Pienkowski T, Burger HU, Laws S, Osterwalder B (2002) Randomised, phase II trial comparing oral capecitabine (Xeloda®) with paclitaxel in patients with metastatic/advanced breast cancer pretreated with anthracyclines. Br J Cancer 86:1367–1372
Magne N, Fischel JL, Dubreuil A, Formento P, Marcie S, Lagrange JL, Milano G (2002) Sequence-dependent effects of ZD1839 (“Iressa”) in combination with cytotoxic treatment in human head and neck cancer. Br J Cancer 86:819–827
Magne N, Fischel JL, Dubreuil A, Formento P, Ciccolini J, Formento JL, Tiffon C, Renee N, Marchetti S, Etienne MC, Milano G (2003) ZD1839 (Iressa) modifies the activity of key enzymes linked to fluoropyrimidine activity: rational basis for a new combination therapy with capecitabine. Clin Cancer Res 9:4735–4742
Ait-Tihyaty M, Rachid Z, Mihalcioiu C, Jean-Claude BJ (2012) Inhibition of EGFR phosphorylation in a panel of human breast cancer cells correlates with synergistic interactions between gefitinib and 5′-DFUR, the bioactive metabolite of Xeloda((R)). Breast Cancer Res Treat 133(1):217–226
Nair P (2005) Epidermal growth factor receptor family and its role in cancer progression. Curr Sci 88:890–898
Yarden Y, Shilo BZ (2007) SnapShot: EGFR signaling pathway. Cell 131(5):1018
Fischer OM, Hart S, Gschwind A, Ullrich A (2003) EGFR signal transactivation in cancer cells. Biochem Soc Trans 31(Pt 6):1203–1208
Roberts PJ, Der CJ (2007) Targeting the Raf-MEK-ERK mitogen-activated protein kinase cascade for the treatment of cancer. Oncogene 26(22):3291–3310
Katsoulas A, Rachid Z, McNamee JP, Williams C, Jean-Claude BJ (2008) Combi-targeting concept: an optimized single-molecule dual-targeting model for the treatment of chronic myelogenous leukemia. Mol Cancer Ther 7(5):1033–1043
Rachid Z, Macphee M, Williams C, Todorova M, Jean-Claude BJ (2009) Design and synthesis of new stabilized combi-triazenes for targeting solid tumors expressing the epidermal growth factor receptor (EGFR) or its closest homologue HER2. Bioorg Med Chem Lett 19(18):5505–5509
Larroque-Lombard AL, Todorova M, Qiyu Q, Jean-Claude B (2011) Synthesis and studies on three-compartment flavone-containing combi-molecules designed to target EGFR, DNA, and MEK. Chem Biol Drug Des 77(5):309–318
Brahimi F, Rachid Z, McNamee JP, Alaoui-Jamali MA, Tari AM, Jean-Claude BJ (2005) Mechanism of action of a novel “combi-triazene” engineered to possess a polar functional group on the alkylating moiety: evidence for enhancement of potency. Biochem Pharmacol 70(4):511–519
MacPhee M, Rachid Z, Todorova M, Qiu Q, Belinsky G, Jean-Claude BJ (2011) Characterization of the potency of epidermal growth factor (EGFR)-DNA targeting combi-molecules containing a hydrolabile carbamate at the 3-position of the triazene chain. Invest New Drugs 29(5):833–845
Brahimi F, Matheson SL, Dudouit F, McNamee JP, Tari AM, Jean-Claude BJ (2002) Inhibition of epidermal growth factor receptor-mediated signaling by “Combi-triazene” BJ2000, a new probe for Combi-Targeting postulates. J Pharmacol Exp Ther 303(1):238–246
Todorova MI, Larroque AL, Dauphin-Pierre S, Fang YQ, Jean-Claude BJ (2010) Subcellular distribution of a fluorescence-labeled combi-molecule designed to block epidermal growth factor receptor tyrosine kinase and damage DNA with a green fluorescent species. Mol Cancer Ther 9(4):869–882
Shindoh H, Kawashima A, Shishido N, Nakano K, Kobayashi K, Horii I (2006) Relationship between AUC of 5′-DFUR and toxicity of capecitabine, fluoropyrimidine carbamate analogs, and 5′-DFUR in monkeys, mice, and rats. J Toxicol Sci 31(3):265–285
Quinney SK, Sanghani SP, Davis WI, Hurley TD, Sun Z, Murry DJ, Bosron WF (2005) Hydrolysis of capecitabine to 5′-deoxy-5-fluorocytidine by human carboxylesterases and inhibition by loperamide. J Pharmacol Exp Ther 313(3):1011–1016
Augusteyn RC, de Jersey J, Webb EC, Zerner B (1969) On the homology of the active-site peptides of liver carboxylesterases. Biochim Biophys Acta 171(1):128–137
Hosokawa M (2008) Structure and catalytic properties of carboxylesterase isozymes involved in metabolic activation of prodrugs. Molecules 13(2):412–431
Saboulard D, Naesens L, Cahard D, Salgado A, Pathirana R, Velazquez S, McGuigan C, De Clercq E, Balzarini J (1999) Characterization of the activation pathway of phosphoramidate triester prodrugs of stavudine and zidovudine. Mol Pharmacol 56(4):693–704
Barker DL, Jencks WP (1969) Pig liver esterase. Physical properties. Biochemistry 8(10):3879–3889
Landowski CP, Lorenzi PL, Song X, Amidon GL (2006) Nucleoside ester prodrug substrate specificity of liver carboxylesterase. J Pharmacol Exp Ther 316(2):572–580
Trempe GL 1976 Human breast cancer in culture. Recent Results Cancer Res Fortschritte der Krebsforschung (57):33–41
Brinkley BR, Beall PT, Wible LJ, Mace ML, Turner DS, Cailleau RM (1980) Variations in cell form and cytoskeleton in human breast carcinoma cells in vitro. Cancer Res 40(9):3118–3129
Kaeser MD, Pebernard S, Iggo RD (2004) Regulation of p53 stability and function in HCT116 colon cancer cells. J Biol Chem 279(9):7598–7605
Hosokawa M, Satoh T (2002) Measurement of carboxylesterase (CES) activities. Current protocols in toxicology / editorial board, Mahin D Maines (editor-in-chief) et al., Chapter 4:Unit4 7
De Angelis P, Svendsrud DH, Kravik KL, Stokke T (2006) Cellular response to 5-fluorouracil (5-FU) in 5-FU-resistant colon cancer cell lines during treatment and recovery. Mol Cancer 5(20)
Wyatt MD, Wilson DM 3rd (2009) Participation of DNA repair in the response to 5-fluorouracil. Cell Mol Life Sci 66(5):788–799
Bunz F, Hwang PM, Torrance C, Waldman T, Zhang Y, Dillehay L, Williams J, Lengauer C, Kinzler KW, Vogelstein B (1999) Disruption of p53 in human cancer cells alters the responses to therapeutic agents. J Clin Invest 104(3):263–269
Mackean M, Planting A, Twelves C, Schellens J, Allman D, Osterwalder B, Reigner B, Griffin T, Kaye S, Verweij J (1998) Phase I and pharmacologic study of intermittent twice-daily oral therapy with capecitabine in patients with advanced and/or metastatic cancer. J Clin Oncol 16(9):2977–2985
Shindoh H, Nakano K, Yoshida T, Ishigai M (2011) Comparison of in vitro metabolic conversion of capecitabine to 5-FU in rats, mice, monkeys and humans—toxicological implications. J Toxicol Sci 36(4):411–422
Acknowledgments
We would like to thank the Canadian Institute of Health Research for their financial support of the project (201816 CIHR Operating Grant MOP-49440). In addition, we would like to express our gratitude to the Research Institute /McGill University Health Center, the McGill/Canadian Institute Health Research Drug development training Program and Fonds de recherche du Québec – Santé (FRQS) for providing Maria Ait-Tihyaty with generous scholarships.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ait-Tihyaty, M., Rachid, Z., Larroque-Lombard, AL. et al. ZRX1, the first EGFR inhibitor-capecitabine based combi-molecule, requires carboxylesterase-mediated hydrolysis for optimal activity. Invest New Drugs 31, 1409–1423 (2013). https://doi.org/10.1007/s10637-013-0008-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-013-0008-y