Abstract
Purpose
To determine whether normal to supernormal 30-Hz flicker ERGs are associated with visual function and prognosis in patients with central retinal artery occlusion (CRAO).
Methods
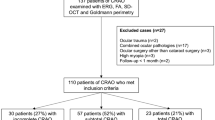
A total of 133 patients diagnosed with unilateral acute non-arteritic CRAO by examination with electroretinography (ERG) were examined. Thirty-hertz flicker ERG amplitudes were analyzed according to the severity of CRAO, and their correlation with visual function and prognosis was assessed. All patients were categorized into one of three groups according to the flicker ERG amplitude ratios between affected and fellow eyes: ≥ 110%, supernormal; 90–110%, normal; and < 90%, subnormal.
Results
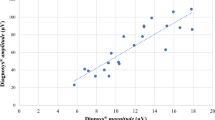
Thirty-hertz flicker ERG parameters differed significantly according to the severity of retinal ischemia, i.e., between incomplete versus complete CRAO: mean amplitude (55.89 ± 24.38 > 45.41 ± 23.47 μV, P = 0.029), amplitude ratio (76.1 ± 23.1% > 58.7 ± 25.7%, P < 0.001), and proportion of normal to supernormal flicker ERGs (30.5% > 12.4%, P < .001). One-month and final follow-up visual function and prognosis were better in the normal to supernormal flicker ERGs: 1 month BCVA (1.55 ± 0.65 > 2.05 ± 0.61 logMAR, P < .001), final BCVA (1.32 ± 0.79 > 1.97 ± 0.68 logMAR, P < .001), 1-month VA improvement (− 0.50 ± 0.47 > − 0.10 ± 0.29 logMAR, P < .001), and final VA improvement (− 0.74 ± 0.61 > − 0.18 ± 0.37 logMAR, P < .001).
Conclusions
Normal to supernormal 30-Hz flicker ERG changes in eyes with CRAO are associated with the milder severity of retinal ischemia and showed better visual function and outcome than the subnormal ERG group.







Similar content being viewed by others
References
Augsburger JJ, Magargal LE (1980) Visual prognosis following treatment of acute central retinal artery obstruction. Br J Ophthalmol 64:913–917
Arruga J, Sanders MD (1982) Ophthalmologic findings in 70 patients with evidence of retinal embolism. Ophthalmology 89:1336–1347
Brown GC, Magargal LE (1982) Central retinal artery obstruction and visual acuity. Ophthalmology 89:14–19
Atebara NH, Brown GC, Cater J (1995) Efficacy of anterior chamber paracentesis and Carbogen in treating acute nonarteritic central retinal artery occlusion. Ophthalmology 102:2029–2034 (discussion 2034–2025)
Hayreh SS, Zimmerman MB (2005) Central retinal artery occlusion: visual outcome. Am J Ophthalmol 140:376–391. https://doi.org/10.1016/j.ajo.2005.03.038
Ahn SJ, Kim JM, Hong JH, Woo SJ, Ahn J, Park KH, Han MK, Jung C (2013) Efficacy and safety of intra-arterial thrombolysis in central retinal artery occlusion. Invest Ophthalmol Vis Sci 54:7746–7755. https://doi.org/10.1167/iovs.13-12952
Ahn SJ, Woo SJ, Park KH, Jung C, Hong JH, Han MK (2015) Retinal and choroidal changes and visual outcome in central retinal artery occlusion: an optical coherence tomography study. Am J Ophthalmol 159(667–676):e661. https://doi.org/10.1016/j.ajo.2015.01.001
Kim HM, Park YJ, Park KH, Woo SJ (2019) Visual field defects and changes in central retinal artery occlusion. PLoS ONE 14:e0209118. https://doi.org/10.1371/journal.pone.0209118
Henkes HE (1954) Electroretinography in circulatory disturbances of the retina. II. The electroretinogram in cases of occlusion of the central retinal artery or of its branches. AMA Arch Ophthalmol 51:42–53
Karpe G, Uchermann A (1955) The clinical electroretinogram. VII. The electroretinogram in circulatory disturbances of the retina. Acta Ophthalmol (Copenh) 33:493–516
McCulloch DL, Marmor MF, Brigell MG, Hamilton R, Holder GE, Tzekov R, Bach M (2015) ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol 130:1–12. https://doi.org/10.1007/s10633-014-9473-7
Yotsukura J, Adachi-Usami E (1993) Correlation of electroretinographic changes with visual prognosis in central retinal artery occlusion. Ophthalmologica 207:13–18. https://doi.org/10.1159/000310400
Machida S, Gotoh Y, Tanaka M, Tazawa Y (2004) Predominant loss of the photopic negative response in central retinal artery occlusion. Am J Ophthalmol 137:938–940. https://doi.org/10.1016/j.ajo.2003.10.023
Matsumoto CS, Shinoda K, Yamada K, Nakatsuka K (2009) Photopic negative response reflects severity of ocular circulatory damage after central retinal artery occlusion. Ophthalmologica 223:362–369. https://doi.org/10.1159/000227782
Marmor MF, Zrenner E (1995) Standard for clinical electroretinography (1994 update). Doc Ophthalmol 89:199–210
Marmor MF, Zrenner E (1998) Standard for clinical electroretinography (1999 update). International society for clinical electrophysiology of vision. Doc Ophthalmol 97:143–156
Johnson MA, Marcus S, Elman MJ, McPhee TJ (1988) Neovascularization in central retinal vein occlusion: electroretinographic findings. Arch Ophthalmol 106:348–352. https://doi.org/10.1001/archopht.1988.01060130374025
Johnson MA, McPhee TJ (1993) Electroretinographic findings in iris neovascularization due to acute central retinal vein occlusion. Arch Ophthalmol 111:806–814. https://doi.org/10.1001/archopht.1993.01090060094030
Matsui Y, Katsumi O, Mehta MC, Hirose T (1994) Correlation of electroretinographic and fluorescein angiographic findings in unilateral central retinal vein obstruction. Graefes Arch Clin Exp Ophthalmol 232:449–457. https://doi.org/10.1007/bf00195353
Yasuda S, Kachi S, Kondo M, Ushida H, Uetani R, Terui T, Piao CH, Terasaki H (2011) Significant correlation between electroretinogram parameters and ocular vascular endothelial growth factor concentration in central retinal vein occlusion eyes. Invest Ophthalmol Vis Sci 52:5737–5742. https://doi.org/10.1167/iovs.10-6923
Miyata R, Kondo M, Kato K, Sugimoto M, Matsubara H, Ikesugi K, Ueno S, Yasuda S, Terasaki H (2018) Supernormal Flicker ERGs in eyes with central retinal vein occlusion: clinical characteristics, prognosis, and effects of anti-VEGF agent. Invest Ophthalmol Vis Sci 59:5854–5861. https://doi.org/10.1167/iovs.18-25087
David NJ, Saito Y, Heyman A (1961) Arm to retina fluorescein appearance time. A new method of diagnosis of carotid artery occlusion. Arch Neurol 5:165–170
Bjarnhall G, Maepea O, Sperber GO, Linden C, Monestam E, Alm A (2002) Analysis of mean retinal transit time from fluorescein angiography in human eyes: normal values and reproducibility. Acta Ophthalmol Scand 80:652–655
Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M, International Society for Clinical Electrophysiology of V (2008 update) (2009) ISCEV Standard for full-field clinical electroretinography. Doc Ophthalmol 118:69–77. https://doi.org/10.1007/s10633-008-9155-4
Larsson J, Andreasson S (2001) Photopic 30 Hz flicker ERG as a predictor for rubeosis in central retinal vein occlusion. Br J Ophthalmol 85:683–685. https://doi.org/10.1136/bjo.85.6.683
Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M (2009) Resolving the clinical acuity categories “hand motion” and “counting fingers” using the freiburg visual acuity test (FrACT). Graefes Arch Clin Exp Ophthalmol 247:137–142. https://doi.org/10.1007/s00417-008-0926-0
Asayama R, Takata H (1965) Electroretinogram in the occlusion of central retinal artery. Nippon Ganka Gakkai Zasshi 69:155–161
Shinoda K, Yamada K, Matsumoto CS, Kimoto K, Nakatsuka K (2008) Changes in retinal thickness are correlated with alterations of electroretinogram in eyes with central retinal artery occlusion. Graefes Arch Clin Exp Ophthalmol 246:949–954. https://doi.org/10.1007/s00417-008-0791-x
Matsumoto CS, Shinoda K, Nakatsuka K (2011) High correlation of scotopic and photopic electroretinogram components with severity of central retinal artery occlusion. Clin Ophthalmol 5:115–121. https://doi.org/10.2147/OPTH.S16053
McLeod D (2019) Misery perfusion, diffusive oxygen shunting and interarterial watershed infarction underlie oxygenation-based hypoperfusion maculopathy. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2019.03.015
Viswanathan S, Frishman LJ, Robson JG, Harwerth RS, Smith EL 3rd (1999) The photopic negative response of the macaque electroretinogram: reduction by experimental glaucoma. Invest Ophthalmol Vis Sci 40:1124–1136
Machida S (2012) Clinical applications of the photopic negative response to optic nerve and retinal diseases. J Ophthalmol 2012:397178. https://doi.org/10.1155/2012/397178
Gouras P, MacKay CJ (1992) Supernormal cone electroretinograms in central retinal vein occlusion. Invest Ophthalmol Vis Sci 33:508–515
Henkes HE (1953) Electroretinography in circulatory disturbances of the retina. I. Electroretinogram in cases of occlusion of central retinal vein or of one of its branches. AMA Arch Ophthalmol 49:190–201. https://doi.org/10.1001/archopht.1953.00920020195009
Sakaue H, Katsumi O, Hirose T (1989) Electroretinographic findings in fellow eyes of patients with central retinal vein occlusion. Arch Ophthalmol 107:1459–1462. https://doi.org/10.1001/archopht.1989.01070020533033
McLeod D, Beatty S (2015) Evidence for an enduring ischaemic penumbra following central retinal artery occlusion, with implications for fibrinolytic therapy. Prog Retin Eye Res 49:82–119. https://doi.org/10.1016/j.preteyeres.2015.06.001
Hayreh SS, Kolder HE, Weingeist TA (1980) Central retinal artery occlusion and retinal tolerance time. Ophthalmology 87:75–78. https://doi.org/10.1016/s0161-6420(80)35283-4
Hayreh SS, Zimmerman MB, Kimura A, Sanon A (2004) Central retinal artery occlusion. Retinal survival time. Exp Eye Res 78:723–736
Feng Y, Venema VJ, Venema RC, Tsai N, Caldwell RB (1999) VEGF induces nuclear translocation of Flk-1/KDR, endothelial nitric oxide synthase, and caveolin-1 in vascular endothelial cells. Biochem Biophys Res Commun 256:192–197. https://doi.org/10.1006/bbrc.1998.9790
Joussen AM, Poulaki V, Qin W, Kirchhof B, Mitsiades N, Wiegand SJ, Rudge J, Yancopoulos GD, Adamis AP (2002) Retinal vascular endothelial growth factor induces intercellular adhesion molecule-1 and endothelial nitric oxide synthase expression and initiates early diabetic retinal leukocyte adhesion in vivo. Am J Pathol 160:501–509. https://doi.org/10.1016/S0002-9440(10)64869-9
Fard MA, Lashey A, Dehpour AR (2010) Aqueous humor nitric oxide in patients with central retinal vein occlusion. Nitric Oxide 23:332–334. https://doi.org/10.1016/j.niox.2010.09.006
Vielma A, Delgado L, Elgueta C, Osorio R, Palacios AG, Schmachtenberg O (2010) Nitric oxide amplifies the rat electroretinogram. Exp Eye Res 91:700–709. https://doi.org/10.1016/j.exer.2010.08.014
Sato M, Ohtsuka T, Stell WK (2011) Endogenous nitric oxide enhances the light-response of cones during light-adaptation in the rat retina. Vision Res 51:131–137. https://doi.org/10.1016/j.visres.2010.10.011
Kim YH, Park KH, Woo SJ (2020) Clinical manifestations and visual prognosis of cilioretinal artery Sparing central retinal artery occlusion. Korean J Ophthal 34(1):27
Funding
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. 2018M3A9B5021319) and a research grant from Seoul National University Bundang Hospital (16-2019-003). The funding organization had no role in the design or conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Ethics Review Board of Seoul National University Bundang Hospital (IRB No. B-1912/582-101) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.M., Park, K.H. & Woo, S.J. Normal to supernormal 30-Hz flicker ERGs predict visual function and prognosis in central retinal artery occlusion. Doc Ophthalmol 141, 279–292 (2020). https://doi.org/10.1007/s10633-020-09775-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-020-09775-y