Abstract
Background/aim
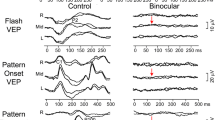
Early and accurate diagnosis of functional visual loss (FVL) allows optimum management. Visual evoked potentials (VEPs) offer a means of objectively estimating acuity and therefore could assist with early and accurate diagnosis. The aim of this study was to assess the sensitivity and specificity of the step VEP in diagnosing FVL.
Methods
A retrospective audit was conducted in 36 school-aged children presenting with reduced visual acuity and clinical suspicion of FVL. All had undergone step VEP testing as part of their investigation. Medical notes were reviewed, and where necessary, referring centres, general practitioners or electronic clinical portals were consulted to obtain longer-term outcome data.
Results
Twenty-seven of the 36 patients (75 %) were classified as having had FVL: all had a normal step VEP spatial threshold. Nine patients (25 %) had an organic cause for their acuity loss, of whom seven had abnormal step VEP spatial thresholds: the other two patients had some functional overlay to their organic disease. The step VEP sensitivity was 78 % (95 % confidence interval 40–96 %), and specificity was 100 % (95 % confidence interval 84–100 %).
Conclusion
The high specificity of the step VEP for FVL warrants increased suspicion of an organic cause should the step VEP spatial threshold be abnormal.



Similar content being viewed by others
References
Chen CS, Lee AW, Karagiannis A, Crompton JL, Selva D (2007) Practical clinical approaches to functional visual loss. J Clin Neurosci 14:1–7
Lessell S (2011) Nonorganic visual loss: what’s in a name? Am J Ophthalmol 151:569–571
Mace CJ, Trimble MR (1991) ‘Hysteria’, ‘functional’ or ‘psychogenic’? A survey of British neurologists’ preferences. J R Soc Med 84:471–475
Taylor D (1997) Non-organic visual disorders. In: Taylor D (ed) Paediatric ophthalmology. Blackwell Science Ltd, London, pp 765–771
Behrman J (1969) The visual evoked response in hysterical amblyopia. Br J Ophthalmol 53:839–845
Potts AM, Nagaya T (1969) Studies on the visual evoked response: III. Strabismus amblyopia and hysterical amblyopia. Doc Ophthalmol 26:394–402
Berman MS, Levi DM (1975) Hysterical amblyopia: electrodiagnostic and clinical evaluation. Am J Optom Physiol Opt 52:267–274
Kramer KK, La Piana FG, Appleton B (1979) Ocular malingering and hysteria: diagnosis and management. Surv Ophthalmol 24:89–96
Röver J, Bach M (1987) Pattern electroretinogram plus visual evoked potential: a decisive test in patients suspected of malingering. Doc Ophthalmol 66:245–251
Bobak P, Khanna P, Goodwin J, Brigell M (1993) Pattern visual evoked potentials in cases of ambiguous acuity loss. Doc Ophthalmol 85:185–192
Saitoh E, Adachi-Usami E, Mizota A, Fujimoto N (2001) Comparison of visual evoked potentials in patients with psychogenic visual disturbance and malingering. J Pediatr Ophthalmol Strabismus 38:21–26
Nakamura A, Tabuchi A, Matsuda E, Yamaguchi W (2000) Dynamic topography of pattern visual evoked potentials (PVEP) in psychogenic visual loss patients. Doc Ophthalmol 101:95–113
Nakamura A, Akio T, Matsuda E, Wakami Y (2001) Pattern visual evoked potentials in malingering. J Neuro-Ophthalmol 21:42–45
McBain VA, Robson AG, Hogg CR, Holder GE (2007) Assessment of patients with suspected non-organic visual loss using pattern appearance visual evoked potentials. Graefes Arch Clin Exp 245:502–510
Xu S, Meyer D, Yoser S, Mathews D, Elfervig JL (2001) Pattern visual evoked potential in the diagnosis of functional visual loss. Ophthalmology 108:76–81
Steele M, Seiple WH, Carr RE, Klug R (1989) The clinical utility of visual-evoked potential acuity testing. Am J Ophthalmol 108:572–577
Tyler CW, Apkarian P, Levi DM, Nakayama K (1979) Rapid assessment of visual function: an electronic sweep technique for the pattern visual evoked potential. Investig Ophthalmol Vis Sci 18:703–713
Mackay AM, Bradnam MS, Hamilton R, Elliot AT, Dutton GN (2008) Real-time rapid acuity assessment using VEPs: development and validation of the step VEP technique. Investig Ophthalmol Vis Sci 49:438–441
Colenbrander A (2003) Aspects of vision loss-visual functions and functional vision. Vis Impair Res 5:115–136
Brown B, Lovie-Kitchin J (1993) Repeated visual acuity measurement: establishing the patient’s own criterion for change. Optom Vis Sci 70(1):45–53
Mackay AM, Hamilton R, Bradnam MS (2003) Faster and more sensitive VEP recording in children. Doc Ophthalmol 107:251–259
Mackay AM, Bradnam MS, Hamilton R (2003) Rapid detection of threshold VEPs. Clin Neurophysiol 114:1009–1020
Victor JD, Mast J (1991) A new statistic for steady-state evoked potentials. Electroencephalog Clin Neurophysiol 78:378–388
Meigen T, Bach M (2000) On the statistical significance of electrophysiological steady-state responses. Doc Ophthalmol 98:207–232
Mackay AM (2003) Assessing children’s visual acuity using steady-state evoked potentials. University of Glasgow. PhD Thesis
Williams C, Northstone K, Sabates R, Feinstein L, Emond A, Dutton GN (2011) Visual perceptual difficulties and under-achievement at school in a large community-based sample of children. PLoS ONE 6:e14772
Acknowledgments
The authors thank the following for providing some of the patients described in this series: Dr. A Brown, Dr. J Dudgeon, Dr. R Bowman, Dr. S Gupta, Dr. I Hanna, Dr. I Hunter, Dr. N Kennedy, Dr. J Kerr, Dr. D Mansfield and Dr. M O’Regan.
Conflict of interests
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamilton, R., Bradnam, M.S., Dutton, G.N. et al. Sensitivity and specificity of the step VEP in suspected functional visual acuity loss. Doc Ophthalmol 126, 99–104 (2013). https://doi.org/10.1007/s10633-012-9362-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-012-9362-x