Abstract
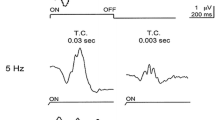
Purpose Occult macular dystrophy (OMD) is an unusual, inherited macular dystrophy characterized by a slowly progressive decline of visual acuity with normal fundus and fluorescein angiography (FA). The authors present a 43-year-old man who was diagnosed as having OMD because of the results of electrophysiological, psychophysical, optical coherence tomography (OCT) tests. Methods Routine ophthalmological evaluation, FA, visual field tests, electroretinographic examinations (EOG, ERG, PERG and mfERG recordings according to ISCEV standards) and foveal thickness measurements (OCT) were performed. Results Funduscopic examinations, FA, full field ERG as well as PERG results were all normal. In both eyes, the abnormalities were observed in static perimetry (relative central scotomas), mfERG (significant reduction of P1 amplitude in the central retinas) and OCT (significantly thinner foveal thickness). Conclusions A new case with OMD is added to preceding reports. The mfERG and OCT tests are important in detection of OMD patients. It can help in differential diagnosis of amblyopia, optic nerve diseases and non-organic visual disorders.





Similar content being viewed by others
References
Miyake Y, Ichikawa K, Shiose Y, Kawase Y (1989) Hereditary macular dystrophy without visible fundus abnormality. Am J Ophthalmol 108:292–299
Miyake Y, Horiguchi M, Tomita N, Kondo M, Tanikawa A, Takahashi H et al (1996) Occult macular dystrophy. Am J Ophthalmol 122:644–653
Miyake Y (2006) Occult macular dystrophy. In: Electrodiagnosis of retinal diseases. Springer-Verlag, Tokyo
Piao Ch, Kondo M, Tanikawa A, Terasaki H, Miyake Y (2000) Multifocal electroretinogram in occult macular dystrophy. Invest Ophthalmol Vis Sci 41:513–517
Matthews GP, Sandberg MA, Berson EL (1992) Foveal cone electroretinograms in patients with central visual loss of unexplained etiology. Arch Ophthalmol 110:1568–1570
Kondo M, Ueno S, Piao Ch, Ito Y, Terasaki H, Miyake Y (2004) Occult macular dystrophy in an 11 year old boy. Br J Ophthalmol 88:1602–1603
Fujii S, Escano MFT, Ishibashi K, Matsuo H, Yamamoto M (1999) Multifocal electroretinography in patients with occult macular dystrophy. Br J Ophthalmol 83:879–880 (letters)
Lyons JS (2005) Non-familial occult macular dystrophy. Doc Ophthalmol 111:49–56
Nakamura M, Kanamori A, Maeda H, Negi A (2003) A case of occult macular dystrophy accompanying normal tension glaucoma. Am J Ophthalmol 135:715–717
Wilderberger H, Niemeyer G, Junghardt A (2003) Multifocal electroretinogram (mfERG) in a family with occult macular dystrophy (OMD). Klin Monatsbl Augenheilkd 220:111–115
Kondo M, Ito Y, Ueno S, Piao Ch, Terasaki H, Miyake Y (2003) Foveal thickness in occult macular dystrophy. Am J Ophthalmol 135:725–728
Brockhurst RJ, Sandberg MA (2007) Optical coherence tomography findings in occult macular dystrophy. Am J Ophthalmol 143: 516–518
Brown M et al (2006) ISCEV Standard for Clinical Electro-oculography (EOG) (2006). Doc Ophthalmol 113:205–212
Marmor MF, Holder GE, Seelinger MW, Yamamoto S (2004 Update) Standard for clinical electroretinography. Doc Ophthalmol 108:107–114
Bach M et al (2000) Standard for pattern electroretinography. Doc Ophthalmol 101:35–49
Holder GE et al (2007) ISCEV standard for clinical pattern electroretinography – 2007 update. Doc Ophthalmol 114:111–116
Marmor MF et al (2003) Guidelines for Basic Multifocal Electroretinography (mfERG). Doc Ophthalmol 106:105–115
Kondo M, Miyake Y, Kondo N, Ueno S, Takakuwa H, Terasaki H (2004) Peripheral cone dystrophy: a variant of cone dystrophy with predominant dysfunction in the peripheral cone system. Ophthalmology 111:732–739
Ohba N (1974) Progressive cone dystrophy: for cases of unusual form. Jpn J Ophthalmol 18:50–69
Kellner V, Jandeck C, Uvaus H, Foerster MH (1998) Hereditäre Makuladystrophien. Ophthalmologe 95(9):597–601
Hood DC, Odel JG, Chen CS, Winn BJ (2003) The multifocal electroretinogram. J Neuro-Ophthalmol 23:225–235
Lois N, Holder GE, Bunce C, Fitzke FW, Bird AC (2001) Phenotypic subtypes of Stargardt macular dystrophy – fundus flavimaculatus. Arch Ophthalmol 119:359–369
Berminger T, Schuurmans RP (1985) Spatial tuning of the pattern ERG across temporal frequency. Doc Ophthalmol 61:17–25
Acknowledgement
The authors thank Mrs. L. Rekowska for her help with recordings and data acquisition.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lubiński, W., Gosławski, W., Penkala, K. et al. A 43-year-old man with reduced visual acuity and normal fundus: occult macular dystrophy—case report. Doc Ophthalmol 116, 111–118 (2008). https://doi.org/10.1007/s10633-007-9086-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-007-9086-5