Abstract
Background and Aims
Chronic digestive disorders are associated with increased costs for healthcare systems and often require provision of both urgent care and non-face-to-face (non-F2F) care, such as responding to patient messages. Numerous benefits of integrated gastroenterology (GI) behavioral health have been identified; however, it is unclear if integrated care impacts healthcare utilization, including urgent care and non-F2F contact. We sought to investigate the association between patient engagement with GI behavioral health and healthcare utilization.
Methods
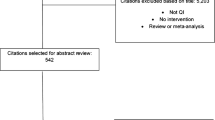
We performed a retrospective chart review study of adult patients who were referred for and completed at least one behavioral health appointment between January 1, 2019 and December 21, 2021 in the Gastroenterology and Hepatology department of a large academic medical center. Data on electronic medical record (EMR) messages, phone calls, and Emergency Department utilization were collected 6 months before and 9 months after patient engagement with GI behavioral health.
Results
466 adult patients completed at least one behavioral health visit from 2019 to 2021. Overall, messages, phone calls, and ED visits all decreased significantly from the 6 months before behavioral health treatment to 6 months after (all P values < 0.001).
Conclusion
Engagement with integrated GI behavioral health is associated with reduced non-F2F care and emergency department utilization in patients with chronic digestive disorders. Increasing access to GI behavioral health may result in reduced provider workload and healthcare system costs.


Similar content being viewed by others
References
Black CJ, Ford AC. Global burden of irritable bowel syndrome: Trends, predictions and risk factors. Nat Rev Gastroenterol Hepatol 2020;17:473–486. https://doi.org/10.1038/s41575-020-0286-8.
Beard JA, Click BH. The burden of cost in inflammatory bowel disease: A medical economic perspective. Curr Opin Gastroenterol 2020;36:310–316. https://doi.org/10.1097/MOG.0000000000000642.
Jalal M, Campbell JA, Hopper AD. Practical guide to the management of chronic pancreatitis. Frontline Gastroenterol 2019;10:253–260. https://doi.org/10.1136/flgastro-2018-101071.
Mikocka-Walus AA, Turnbull DA, Andrews JM et al. Psychological problems in gastroenterology outpatients: A South Australian experience. Psychological co-morbidity in IBD, IBS and hepatitis C. Clin Pract Epidemiol Ment Health 2008;4:15. https://doi.org/10.1186/1745-0179-4-15.
Szigethy E, Murphy SM, Ehrlich OG et al. Mental health costs of inflammatory Bowel diseases. Inflamm Bowel Dis 2021;27:40–48. https://doi.org/10.1093/ibd/izaa030.
Bosman MHMA, Weerts ZZRM, Snijkers JTW et al. The socioeconomic impact of irritable Bowel syndrome: An analysis of direct and indirect health care costs. Clin Gastroenterol Hepatol. 2023. https://doi.org/10.1016/j.cgh.2023.01.017.
Eschenroeder HC, Manzione LC, Adler-Milstein J et al. Associations of physician burnout with organizational electronic health record support and after-hours charting. J Am Med Inform Assoc 2021;28:960–966. https://doi.org/10.1093/jamia/ocab053.
Drossman DA, Chang L, Deutsch JK et al. A review of the evidence and recommendations on communication skills and the patient-provider relationship: A Rome foundation working team report. Gastroenterology 2021;161:1670-1688.e7. https://doi.org/10.1053/j.gastro.2021.07.037.
Thun S, Halsteinli V, Løvseth L. A study of unreasonable illegitimate tasks, administrative tasks, and sickness presenteeism amongst Norwegian physicians: An everyday struggle? BMC Health Serv Res 2018;18:407. https://doi.org/10.1186/s12913-018-3229-0.
Li C, Parpia C, Sriharan A, Keefe DT. Electronic medical record-related burnout in healthcare providers: A scoping review of outcomes and interventions. BMJ Open 2022;12:e060865. https://doi.org/10.1136/bmjopen-2022-060865.
Hodkinson A, Zhou A, Johnson J et al. Associations of physician burnout with career engagement and quality of patient care: Systematic review and meta-analysis. BMJ. 2022. https://doi.org/10.1136/bmj-2022-070442.
Kruimel J, Leue C, Winkens B et al. Integrated medical–psychiatric outpatient care in functional gastrointestinal disorders improves outcome: A pilot study. Eur J Gastroenterol Hepatol 2015;27:721–727. https://doi.org/10.1097/MEG.0000000000000335.
Basnayake C, Kamm MA, Stanley A et al. Long-term outcome of multidisciplinary versus standard gastroenterologist care for functional gastrointestinal disorders: A randomized trial. Clin Gastroenterol Hepatol 2022;20:2102-2111.e9. https://doi.org/10.1016/j.cgh.2021.12.005.
Basnayake C, Kamm MA, Stanley A et al. Standard gastroenterologist versus multidisciplinary treatment for functional gastrointestinal disorders (MANTRA): An open-label, single-centre, randomised controlled trial. Lancet Gastroenterol Hepatol 2020;5:890–899. https://doi.org/10.1016/S2468-1253(20)30215-6.
Kinsinger SW. Snapshot of an integrated psychosocial gastroenterology service. World J Gastroenterol 2015;21:1893. https://doi.org/10.3748/wjg.v21.i6.1893.
Lores T, Goess C, Mikocka-Walus A et al. Integrated psychological care reduces health care costs at a hospital-based inflammatory Bowel disease service. Clin Gastroenterol Hepatol 2021;19:96-103.e3. https://doi.org/10.1016/j.cgh.2020.01.030.
Chey WD, Keefer L, Whelan K, Gibson PR. Behavioral and diet therapies in integrated care for patients with irritable Bowel syndrome. Gastroenterology 2021;160:47–62. https://doi.org/10.1053/j.gastro.2020.06.099.
Colombel JF, Shin A, Gibson PR. AGA clinical practice update on functional gastrointestinal symptoms in patients with inflammatory Bowel disease: Expert review. Clin Gastroenterol Hepatol 2019;17:380-390.e1. https://doi.org/10.1016/j.cgh.2018.08.001.
Salwen-Deremer JK, Bardach SH, Tormey LK, Szkodny LE, Gohres K, Siegel CA. Redesigning a gastroenterology behavioral health program to improve patient access. Clin Gastroenterol Hepatol 2024;22:12-15.e1. https://doi.org/10.1016/j.cgh.2023.09.032.
Drossman DA, Chang LC, Chey WD, Kellow J, Tack J, Whitehead WE. Rome IV functional gastrointestinal disorders: Disorders of gut–brain interaction, 4th edn. Raleigh: The Rome Foundation; 2016.
Burton Murray H, Ljótsson B. Future of brain–gut behavior therapies: Mediators and moderators. Gastroenterol Clin North Am 2022;51:723–739. https://doi.org/10.1016/j.gtc.2022.06.011.
Amrhein V, Trafimow D, Greenland S. Inferential statistics as descriptive statistics: There is no replication crisis if we don’t expect replication. Am Stat 2019;73:262–270. https://doi.org/10.1080/00031305.2018.1543137.
Aziz I, Simrén M. The overlap between irritable bowel syndrome and organic gastrointestinal diseases. Lancet Gastroenterol Hepatol 2021;6:139–148. https://doi.org/10.1016/S2468-1253(20)30212-0.
Guadagnoli L, Geeraerts A, Geysen H et al. Psychological processes, not physiological parameters, are most important contributors to symptom severity in patients with refractory heartburn/regurgitation symptoms. Gastroenterology 2023;165:848–860. https://doi.org/10.1053/j.gastro.2023.06.019.
Sperber AD, Freud T, Aziz I et al. Greater overlap of Rome IV disorders of gut–brain interactions leads to increased disease severity and poorer quality of life. Clin Gastroenterol Hepatol 2022;20:e945–e956. https://doi.org/10.1016/j.cgh.2021.05.042.
Ford AC, Lacy BE, Harris LA, Quigley EMM, Moayyedi P. Effect of antidepressants and psychological therapies in irritable Bowel syndrome: An updated systematic review and meta-analysis. Am J Gastroenterol 2019;114:21–39. https://doi.org/10.1038/s41395-018-0222-5.
Rodrigues DM, Motomura DI, Tripp DA, Beyak MJ. Are psychological interventions effective in treating functional dyspepsia? A systematic review and meta-analysis. J Gastroenterol Hepatol 2021;36:2047–2057. https://doi.org/10.1111/jgh.15566.
Timmer A, Preiss JC, Motschall E, Rücker G, Jantschek G, Moser G. Psychological interventions for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2011. https://doi.org/10.1002/14651858.CD006913.pub2.
Keefer L, Doerfler B, Artz C. Optimizing management of Crohnʼs disease within a project management framework: Results of a pilot study§. Inflamm Bowel Dis 2012;18:254–260. https://doi.org/10.1002/ibd.21679.
Riehl ME, Pandolfino JE, Palsson OS, Keefer L. Feasibility and acceptability of esophageal-directed hypnotherapy for functional heartburn: Hypnotherapy for functional heartburn. Dis Esophagus 2016;29:490–496. https://doi.org/10.1111/dote.12353.
Murray HB, Juarascio AS, Di Lorenzo C, Drossman DA, Thomas JJ. Diagnosis and treatment of rumination syndrome: A critical review. Am J Gastroenterol 2019;114:562–578. https://doi.org/10.14309/ajg.0000000000000060.
Glasinovic E, Wynter E, Arguero J et al. Treatment of supragastric belching with cognitive behavioral therapy improves quality of life and reduces acid gastroesophageal reflux. Am J Gastroenterol 2018;113:539–547. https://doi.org/10.1038/ajg.2018.15.
Adler-Milstein J, Zhao W, Willard-Grace R, Knox M, Grumbach K. Electronic health records and burnout: Time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. J Am Med Inform Assoc 2020;27:531–538. https://doi.org/10.1093/jamia/ocz220.
Funding
This work received support from Susan and Richard Levy Healthcare Delivery Incubator.
Author information
Authors and Affiliations
Contributions
B. A. was lead in project conceptualization, planning, and drafting of the manuscript; M.C. contributed to project conceptualization and drafting of the manuscript; P. M-C conducted statistical analyses and interpretation; L.T. contributed to collecting data, drafting of the manuscript; J. S-D contributed to planning/conducting study, collecting data, and drafting of the manuscript. Each author has approved the final draft of the manuscript being submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arizmendi, B.J., Craven, M.R., Martinez-Camblor, P. et al. Engagement in GI Behavioral Health Is Associated with Reduced Portal Messages, Phone Calls, and ED Visits. Dig Dis Sci (2024). https://doi.org/10.1007/s10620-024-08428-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10620-024-08428-3