Abstract
Background
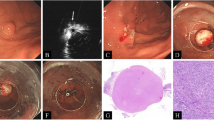
We previously treated small gastric submucosal tumors originating from the muscularis propria layer by precutting endoscopic band ligation but lacked precise pathological results. Then, precutting endoscopic band ligation was modified by additional snare resection after ligation to obtain tumor specimens, termed precutting endoscopic band ligation-assisted resection.
Aims
In this study, we aimed to explore the safety, feasibility, and efficacy of precutting endoscopic band ligation-assisted resection.
Methods
From 2021 to 2022, a total of 16 consecutive patients underwent precutting endoscopic band ligation-assisted resection to treat small gastric submucosal tumors originating from the muscularis propria. The clinical demography, perioperative data, and follow-up outcomes were retrospectively collected.
Results
With a mean operative time of 21.3 min, all lesions were successfully and completely resected, and no severe adverse events or local recurrences occurred postoperatively. More importantly, en bloc and R0 resection were achieved in all 16 patients.
Conclusion
Precutting endoscopic band ligation-assisted resection is a safe, effective, and time-saving endoscopic technique for managing gastric small gastric submucosal tumors originating from the muscularis propria for both diagnosis and eradication.
Graphical Abstract



Similar content being viewed by others
References
Zhang D, Lin Q, Shi R, et al. Ligation-assisted endoscopic submucosal resection with apical mucosal incision to treat gastric subepithelial tumors originating from the muscularis propria. Endoscopy 2018; 50: 1180–1185.
Liu S, Zhou X, Yao Y, et al. Resection of the gastric submucosal tumor (G-SMT) originating from the muscularis propria layer: comparison of efficacy, patients’ tolerability, and clinical outcomes between endoscopic full-thickness resection and surgical resection. Surg Endosc 2020; 34: 4053–4064.
Li B, Chen T, Qi Z-P, et al. Efficacy and safety of endoscopic resection for small submucosal tumors originating from the muscularis propria layer in the gastric fundus. Surg Endosc 2019; 33: 2553–2561.
Bruno M, Carucci P, Repici A, et al. The natural history of gastrointestinal subepithelial tumors arising from muscularis propria: an endoscopic ultrasound survey. J Clin Gastroenterol 2009; 43: 821–825.
Sharzehi K, Sethi A, Savides T. AGA clinical practice update on management of subepithelial lesions encountered during routine endoscopy: expert review. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2022; 20: 2435-2443.e2434.
Shiratori W, Matsumura T, Okimoto K, et al. Long-term course of gastric submucosal tumors: growth speed and size-increasing factors. Gastrointest Endosc. 2023. https://doi.org/10.1016/j.gie.2023.01.020.
Li S, Liang X, Zhang B, et al. Novel endoscopic management for small gastric submucosal tumors: a single-center experience (with video). Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver 2021; 53: 895–899.
Siyu S, Sheng W, Guoxin W, et al. Gastric perforations after ligation of GI stromal tumors in the gastric fundus. Gastrointest Endosc 2010; 72: 615–616.
Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 2006; 23: 70–83.
Joensuu H, Hohenberger P, Corless CL. Gastrointestinal stromal tumour. Lancet (Lond Engl) 2013; 382: 973–983.
Guo J, Liu Z, Sun S, et al. Endoscopic full-thickness resection with defect closure using an over-the-scope clip for gastric subepithelial tumors originating from the muscularis propria. Surg Endosc 2015; 29: 3356–3362.
Kushnir VM, Keswani RN, Hollander TG, et al. Compliance with surveillance recommendations for foregut subepithelial tumors is poor: results of a prospective multicenter study. Gastrointest Endosc 2015; 81: 1378–1384.
Karaca C, Turner BG, Cizginer S, et al. Accuracy of EUS in the evaluation of small gastric subepithelial lesions. Gastrointest Endosc 2010; 71: 722–727.
Coe TM, Fero KE, Fanta PT, et al. Population-based epidemiology and mortality of small malignant gastrointestinal stromal tumors in the USA. J Gastrointest Surg 2016; 20: 1132–1140.
Tanaka J, Oshima T, Hori K, et al. Small gastrointestinal stromal tumor of the stomach showing rapid growth and early metastasis to the liver. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 2010; 22: 354–356.
Chen H, Li B, Li L, et al. Current status of endoscopic resection of gastric subepithelial tumors. Am J Gastroenterol 2019; 114: 718–725.
Meng Y, Cao C, Song S, et al. Endoscopic band ligation versus endoscopic submucosal dissection and laparoscopic resection for small gastric stromal tumors. Surg Endosc 2016; 30: 2873–2878.
Chang KJ, Yoshinaka R, Nguyen P. Endoscopic ultrasound-assisted band ligation: a new technique for resection of submucosal tumors. Gastrointest Endosc 1996; 44: 720–722.
Sun S, Jin Y, Chang G, et al. Endoscopic band ligation without electrosurgery: a new technique for excision of small upper-GI leiomyoma. Gastrointest Endosc 2004; 60: 218–222.
Pan W, Shi D. Band-assisted endoscopic mucosal resection for small (≤ 1.5 cm) submucosal tumors originating from the muscularis propria in the gastric fundus: a prospective study. Surg Endosc. 2022. https://doi.org/10.1007/s00464-022-09688-8.
Huang WH, Feng CL, Lai HC, et al. Endoscopic ligation and resection for the treatment of small EUS-suspected gastric GI stromal tumors. Gastrointest Endosc 2010; 71: 1076–1081.
Binmoeller KF, Shah JN, Bhat YM, et al. Suck-ligate-unroof-biopsy by using a detachable 20-mm loop for the diagnosis and therapy of small subepithelial tumors (with video). Gastrointest Endosc 2014; 79: 750–755.
Mao X, Yang X, Chen X, et al. Single-cell transcriptome analysis revealed the heterogeneity and microenvironment of gastrointestinal stromal tumors. Cancer Sci 2021; 112: 1262–1274.
Huang ZZ, Mao R, Li YQ, et al. Cost-efficient snare-assisted peroral endoscopic myotomy in comparison of conventional endoscopic knife for treatment of achalasia: results of a randomized controlled trial. Dis Esophagus Off J Int Soc Dis Esophagus 2022; 35: doab099.
Fujiya M, Tanaka K, Dokoshi T, et al. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc 2015; 81: 583–595.
Feng WA, Zeineddin S, Mazraani M, et al. Transvaginal resection of a gastrointestinal stromal tumor (GIST) of the rectum. Am Surg 2023; 89: 3289–3291.
Ye JX, Liu Y, Qin Y, et al. Mast cells or not? CD117 positive cells in esophageal leiomyoma. Histol Histopathol 2015; 30: 581–588.
Lee JH, Kedia P, Stavropoulos SN, et al. AGA clinical practice update on endoscopic management of perforations in gastrointestinal tract: expert review. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2021; 19: 2252-2261.e2252.
Takada J, Araki H, Onogi F, et al. Safety and efficacy of carbon dioxide insufflation during gastric endoscopic submucosal dissection. World J Gastroenterol 2015; 21: 8195–8202.
Dike CR, Rahhal R, Bishop WP. Is carbon dioxide insufflation during endoscopy in children as safe and as effective as we think? J Pediatr Gastroenterol Nutr 2020; 71: 211–215.
Gündüz F, Kani HT, Chang S, et al. Effect of carbon dioxide versus room air insufflation on post-colonoscopic pain: a prospective, randomized, controlled study. Turk J Gastroenterol Off J Turk Soc Gastroenterol 2020; 31: 676–680.
Kim SH, Hong SJ. A prospective randomized controlled trial of the safety and efficacy of carbon dioxide insufflation compared with room air insufflation during gastric endoscopic submucosal dissection. J Gastroenterol Hepatol 2022; 37: 558–567.
Binmoeller KF. Resecting a small gastrointestinal stromal tumor: feasible, but are you feeling lucky today? Endoscopy 2018; 50: 1143–1145.
Martínek J, Ryska O, Tuckova I, et al. Comparing over-the-scope clip versus endoloop and clips (KING closure) for access site closure: a randomized experimental study. Surg Endosc 2013; 27: 1203–1210.
Funding
This study was supported by the Joint Project Foundation of Chongqing Health Commission and Chongqing Scientific and Technological Commission (Grant No. 2021MSXM103). This study was also supported by the Chongqing Science and Technology Commission Foundation (cstc2020jcyj-msxmX0045).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (AVI 48425 KB) Video 1: The entire procedure for precutting EBLR
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, S., Li, Q., Liu, M. et al. Precutting Endoscopic Band Ligation-Assisted Resection Is Safe and Effective for Treating Gastric Submucosal Tumors from the Muscularis Propria. Dig Dis Sci 69, 1762–1769 (2024). https://doi.org/10.1007/s10620-024-08381-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08381-1