Abstract
Background
Recurrence of common bile duct stones (CBDs) commonly happens after endoscopic retrograde cholangiopancreatography (ERCP). The clinical prediction models for the recurrence of CBDs after ERCP are lacking.
Aims
We aim to develop high-performance prediction models for the recurrence of CBDS after ERCP treatment using automated machine learning (AutoML) and to assess the AutoML models versus the traditional regression models.
Methods
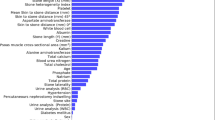
473 patients with CBDs undergoing ERCP were recruited in the single-center retrospective cohort study. Samples were divided into Training Set (65%) and Validation Set (35%) randomly. Three modeling approaches, including fully automated machine learning (Fully automated), semi-automated machine learning (Semi-automated), and traditional regression were applied to fit prediction models. Models’ discrimination, calibration, and clinical benefits were examined. The Shapley additive explanations (SHAP), partial dependence plot (PDP), and SHAP local explanation (SHAPLE) were proposed for the interpretation of the best model.
Results
The area under roc curve (AUROC) of semi-automated gradient boost machine (GBM) model was 0.749 in Validation Set, better than the other fully/semi-automated models and the traditional regression models (highest AUROC = 0.736). The calibration and clinical application of AutoML models were adequate. Through the SHAP-PDP-SHAPLE pipeline, the roles of key variables of the semi-automated GBM model were visualized. Lastly, the best model was deployed online for clinical practitioners.
Conclusion
The GBM model based on semi-AutoML is an optimal model to predict the recurrence of CBDs after ERCP treatment. In comparison with traditional regressions, AutoML algorithms present significant strengths in modeling, which show promise in future clinical practices.







Similar content being viewed by others
References
Wu Y, Xu CJ, Xu SF. Advances in risk factors for recurrence of common bile duct stones. Int J Med Sci. 2021;18:1067–1074.
Kim DI, Kim MH, Lee SK et al. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42–48.
Dasari BV, Tan CJ, Gurusamy KS et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2013;12:CD003327.
Nzenza TC, Al-Habbal Y, Guerra GR, Manolas S, Yong T, McQuillan T. Recurrent common bile duct stones as a late complication of endoscopic sphincterotomy. BMC Gastroenterol. 2018;18:39.
Park SY, Hong TH, Lee SK, Park IY, Kim TH, Kim SG. Recurrence of common bile duct stones following laparoscopic common bile duct exploration: a multicenter study. J Hepato-Biliary-Pancreat Sci. 2019;26:578–582.
Waring J, Lindvall C, Umeton R. Automated machine learning: Review of the state-of-the-art and opportunities for healthcare. Artif Intell Med. 2020;104:101822.
Vickers AJ, Elkin EB. Decision Curve Analysis: A Novel Method for Evaluating Prediction Models. Med Decis Making. 2006;26:565–574.
Lundberg S M, Lee S I. A unified approach to interpreting model predictions. Advances in neural information processing systems. 2017:30.
Zhang Z. Univariate description and bivariate statistical inference: the first step delving into data. Ann Transl Med. 2016;4:91.
Grimes DA. The nomogram epidemic: resurgence of a medical relic. Ann Intern Med. 2008;149:273–275.
Luo J, Wu M, Gopukumar D, Zhao Y. Big data application in biomedical research and health care: a literature review. Biomed Inform Insights. 2016;8:1.
Toga AW, Foster I, Kesselman C et al. Big biomedical data as the key resource for discovery science. J Am Med Inform Assoc. 2015;22:1126–1131.
Murdoch TB, Detsky AS. The inevitable application of big data to health care. JAMA. 2013;309:1351–1352.
Wolpert DH, Macready WG. No free lunch theorems for optimization. IEEE Trans Evol Comput. 1997;1:67–82.
Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019;380:1347–1358.
Beam AL, Kohane IS. Big data and machine learning in health care. JAMA. 2018;319:1317–1318.
Pereira-Lima JC, Jakobs R, Winter UH et al. Long-term results (7 to 10 years) of endoscopic papillotomy for choledocholithiasis: Multivariate analysis of prognostic factors for the recurrence of biliary symptoms. Gastrointest Endosc. 1998;48:457–464.
Kawaji Y, Isayama H, Nakai Y et al. Multiple recurrences after endoscopic removal of common bile duct stones: A retrospective analysis of 976 cases. J Gastroenterol Hepatol. 2019;34:1460–1466.
Deng F, Zhou M, Liu P-P et al. Causes associated with recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography: A large sample sized retrospective study. World J Clin Cases. 2019;7:1028–1037.
Song ME, Chung MJ, Lee DJ et al. Cholecystectomy for prevention of recurrence after endoscopic clearance of bile duct stones in Korea. Yonsei Med J. 2016;57:132–137.
Jeon J, Lim SU, Park C-H, Jun C-H, Park S-Y, Rew J-S. Restoration of common bile duct diameter within 2 weeks after endoscopic stone retraction is a preventive factor for stone recurrence. Hepatobiliary Pancreat Dis Int HBPD INT. 2018;17:251–256.
Marin JJG, Macias RIR, Briz O, Banales JM, Monte MJ. Bile acids in physiology, pathology and pharmacology. Curr Drug Metab. 2015;17:4–29.
Beuers U, Trauner M, Jansen P, Poupon R. New paradigms in the treatment of hepatic cholestasis: from UDCA to FXR. PXR and beyond. J Hepatol. 2015;62:S25-37.
Yoo ES, Yoo BM, Kim JH et al. Evaluation of risk factors for recurrent primary common bile duct stone in patients with cholecystectomy. Scand J Gastroenterol. 2018;53:466–470.
Lu JP, Xian NC, Lei Z. Risk factors of stone recurrence after endoscopic retrograde cholangiopancreatography for common bile duct stones. Medicine (Baltimore). 2020;99:e20412.
Lu Y, Wu JC, Liu L, Bie LK, Gong B. Short-term and long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Eur J Gastroenterol Hepatol. 2014;26:1367–1373.
Ohashi A, Tamada K, Wada S et al. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc Off J Jpn Gastroenterol Endosc Soc. 2009;21:73–77.
Funding
The work was supported by the National Natural Science Foundation of China (82000540), the Youth Program of Suzhou Health Committee (KJXW2019001), Development Project of Clinical Medicine in Jiangsu University (JLY20180134), Science and Technology Plan (Apply Basic Research) of Changzhou City (CJ20210006), and Science and Technology Plan of Suzhou City (SKY2021038).
Author information
Authors and Affiliations
Contributions
CX and JZ took part in the study concept and design. JG, LL, MY, CY, and XL involved in the acquisition of data. JL and YS were involved in statistical analyses. YS, JL, and YW participated in the first draft of the manuscript. JZ made the critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
No relevant conflicts of interest to declare among authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, Y., Lin, J., Zhu, J. et al. Predicting the Recurrence of Common Bile Duct Stones After ERCP Treatment with Automated Machine Learning Algorithms. Dig Dis Sci 68, 2866–2877 (2023). https://doi.org/10.1007/s10620-023-07949-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07949-7