Abstract
Background
Although dysmenorrhea is a highly prevalent risk factor for irritable bowel syndrome (IBS), the factors underlying this risk are not fully understood. Prior studies support a hypothesis that repeated distressing menstrual pain promotes cross-organ pelvic sensitization with heightened visceral sensitivity.
Aims
To further explore cross-organ pelvic sensitization we examined the association of dysmenorrhea, provoked bladder pain, and other putative factors with self-reported IBS-domain pain frequency and new onset after 1-year follow up.
Methods
We measured visceral pain sensitivity with a noninvasive provoked bladder pain test in a cohort of reproductive-aged women, enriched for those reporting moderate-to-severe menstrual pain intensity but without any prior IBS diagnosis (n = 190). We analyzed the relationship between menstrual pain, provoked bladder pain, pain catastrophizing, anxiety, and depression with primary outcomes: (1) frequency of self-reported IBS-domain pain and (2) new onset of IBS-domain pain after 1-year follow up.
Results
All hypothesized factors correlated with the frequency of IBS-domain pain (p’s ≤ 0.038). In a cross-sectional model, only menstrual pain (standardized adjusted odds ratio 2.07), provoked bladder pain (1.49), and anxiety (1.90) were independently associated with IBS-domain pain ≥ 2 days/month (C statistic = 0.79). One year later, provoked bladder pain (3.12) was the only significant predictor of new onset IBS-domain pain (C statistic = 0.87).
Conclusion
Increased visceral sensitivity among women with dysmenorrhea could lead to IBS. Because provoked bladder pain predicted subsequent IBS, prospective studies should be performed to see if the early treatment of visceral hypersensitivity mitigates IBS.
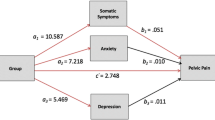
Graphical Abstract



Similar content being viewed by others
Data availability
Data is available at open science framework: https://doi.org/10.17605/OSF.IO/BMA4P
References
Canavan C, West J, Card T. The epidemiology of irritable bowel syndrome. Clin Epidemiol. 2014;6:71–80.
Manning AP, Thompson WG, Heaton KW et al. Towards positive diagnosis of the irritable bowel. Br Med J. 1978;2:653–654.
Kennedy TM, Jones RH, Hungin AP et al. Irritable bowel syndrome, gastro-oesophageal reflux, and bronchial hyper-responsiveness in the general population. Gut. 1998;43:770–774.
Kim YS, Kim N. Sex-Gender Differences in Irritable Bowel Syndrome. J Neurogastroenterol Motil. 2018;24:544–558.
Olafsdottir LB, Gudjonsson H, Jonsdottir HH et al. Natural History of Irritable Bowel Syndrome in Women and Dysmenorrhea: A 10-Year Follow-Up Study. Gastroenterol Res Pract. 2012;2012:1–7.
Zondervan KT, Yudkin PL, Vessey MP et al. The community prevalence of chronic pelvic pain in women and associated illness behaviour. Br J Gen Pract. 2001;51:541–547.
Giamberardino MA, Costantini R, Affaitati G et al. Viscero-visceral hyperalgesia: characterization in different clinical models. Pain. 2010;151:307–322.
Heitkemper M, Burr RL, Jarrett M et al. Evidence for autonomic nervous system imbalance in women with irritable bowel syndrome. Dig Dis Sci. 1998;43:2093–2098.
Albusoda A, Ruffle JK, Friis KA et al. Systematic review with meta-analysis: conditioned pain modulation in patients with the irritable bowel syndrome. Aliment Pharmacol Ther. 2018;48:797–806.
Pittayanon R, Lau JT, Yuan Y et al. Gut Microbiota in Patients With Irritable Bowel Syndrome-A Systematic Review. Gastroenterology. 2019;157:97–108.
Simpson CA, Mu A, Haslam N et al. Feeling down? A systematic review of the gut microbiota in anxiety/depression and irritable bowel syndrome. J Affect Disord. 2020;266:429–446.
Mayer EA, Labus JS, Tillisch K et al. Towards a systems view of IBS. Nat Rev Gastroenterol Hepatol. 2015;12:592–605.
Latthe P, Mignini L, Gray R et al. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332:749–755.
Nicholl BI, Halder SL, Macfarlane GJ et al. Psychosocial risk markers for new onset irritable bowel syndrome – Results of a large prospective population-based study. Pain. 2008;137:147–155.
Hollier JM, van Tilburg MAL, Liu Y et al. Multiple Psychological Factors Predict Abdominal Pain Severity in Children with Irritable Bowel Syndrome. Neurogastroenterol Motil. 2019;31:e13509.
van Tilburg MAL, Palsson OS, Whitehead WE. Which psychological factors exacerbate irritable bowel syndrome? Development of a comprehensive model. J Psychosom Res. 2013;74:486–492.
Mertz H, Naliboff B, Munakata J et al. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology. 1995;109:40–52.
Dorn SD, Palsson OS, Thiwan SIM et al. Increased colonic pain sensitivity in irritable bowel syndrome is the result of an increased tendency to report pain rather than increased neurosensory sensitivity. Gut. 2007;56:1202–1209.
Walker LS, Williams SE, Smith CA et al. Validation of a symptom provocation test for laboratory studies of abdominal pain and discomfort in children and adolescents. J Pediatr Psychol. 2006;31:703–713.
Hellman KM, Datta A, Steiner ND et al. Identification of experimental bladder sensitivity among dysmenorrhea sufferers. Am J Obstet Gynecol. 2018;219(84):e1-84.e8.
Tu FF, Hellman KM, Roth GE, et al. Noninvasive bladder testing of adolescent females to assess visceral hypersensitivity. Pain. 2021; Publish Ahead of Print.
Hellman KM, Roth GE, Dillane KE et al. Dysmenorrhea subtypes exhibit differential quantitative sensory assessment profiles. Pain. 2020;161:1227–1236.
Sabate J-M, Veyrac M, Mion F et al. Relationship between rectal sensitivity, symptoms intensity and quality of life in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2008;28:484–490.
Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11:395–402.
Azpiroz F, Guyonnet D, Donazzolo Y et al. Digestive Symptoms in Healthy People and Subjects With Irritable Bowel Syndrome: Validation of Symptom Frequency Questionnaire. J Clin Gastroenterol. 2015;49:e64-70.
Patrick DL, Drossman DA, Frederick IO et al. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400–411.
Katsarava Z, Schneeweiss S, Kurth T et al. Incidence and predictors for chronicity of headache in patients with episodic migraine. Neurology. 2004;62:788–790.
Friedman BW, Hochberg ML, Esses D et al. Applying the International Classification of Headache Disorders to the emergency department: an assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann Emerg Med. 2007;49:419.e1–9.
Hirschfeld G, Zernikow B. Variability of “optimal” cut points for mild, moderate, and severe pain: neglected problems when comparing groups. Pain. 2013;154:154–159.
Boonstra AM, Stewart RE, Köke AJA et al. Cut-Off Points for Mild, Moderate, and Severe Pain on the Numeric Rating Scale for Pain in Patients with Chronic Musculoskeletal Pain: Variability and Influence of Sex and Catastrophizing. Front Psychol. 2016. https://doi.org/10.3389/fpsyg.2016.01466.
Harris PA, Taylor R, Thielke R et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42:377–381.
Ford AC, Bercik P, Morgan DG et al. Validation of the Rome III criteria for the diagnosis of irritable bowel syndrome in secondary care. Gastroenterology. 2013;145:1262-1270.e1.
Casper RF, Powell AM. Premenstrual syndrome: documentation by a linear analog scale compared with two descriptive scales. Am J Obstet Gynecol. 1986;155:862–867.
Hjermstad MJ, Fayers PM, Haugen DF et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41:1073–1093.
Neal KR, Barker L, Spiller RC. Prognosis in post-infective irritable bowel syndrome: a six year follow up study. Gut. 2002;51:410–413.
Cella D, Riley W, Stone A et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194.
Tu FF, Kane JN, Hellman KM. Noninvasive experimental bladder pain assessment in painful bladder syndrome. BJOG. 2017;124:283–291.
Tu FF, Epstein AE, Pozolo KE et al. A noninvasive bladder sensory test supports a role for dysmenorrhea increasing bladder noxious mechanosensitivity. Clin J Pain. 2013;29:883–890.
Faul F, Erdfelder E, Lang A-G et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal statistical society: series B (Methodological). 1995;57:289–300.
Hosmer DW, Lemesbow S. Goodness of fit tests for the multiple logistic regression model. Communications in statistics-Theory and Methods. 1980;9:1043–1069.
Thompson CG, Kim RS, Aloe AM et al. Extracting the variance inflation factor and other multicollinearity diagnostics from typical regression results. Basic and Applied Social Psychology. 2017;39:81–90.
Austin PC, Steyerberg EW. Interpreting the concordance statistic of a logistic regression model: relation to the variance and odds ratio of a continuous explanatory variable. BMC Med Res Methodol. 2012;12:82.
Westling AM, Tu FF, Griffith JW et al. The association of dysmenorrhea with noncyclic pelvic pain accounting for psychological factors. Am J Obstet Gynecol. 2013;209:e1-422.e10.
Heitkemper MM, Jarrett M. Pattern of gastrointestinal and somatic symptoms across the menstrual cycle. Gastroenterology. 1992;102:505–513.
Heitkemper MM, Cain KC, Jarrett ME et al. Symptoms across the menstrual cycle in women with irritable bowel syndrome. Am J Gastroenterol. 2003;98:420–430.
Gore M, Brandenburg NA, Dukes E et al. Pain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleep. J Pain Symptom Manage. 2005;30:374–385.
Gerrits MMJG, van Marwijk HWJ, van Oppen P et al. Longitudinal association between pain, and depression and anxiety over four years. J Psychosom Res. 2015;78:64–70.
Yamamoto Y, Furukawa S, Watanabe J et al. Association between menstrual pain and functional dyspepsia in a Japanese young population. Neurogastroenterol Motil. 2022;34:e14324.
Böttcher B, Gizewski ER, Siedentopf C et al. Behavioural and neural responses to aversive visceral stimuli in women with primary dysmenorrhoea. Eur J Pain. 2019;23:272–284.
Peng H-Y, Huang P-C, Liao J-M et al. Estrous cycle variation of TRPV1-mediated cross-organ sensitization between uterus and NMDA-dependent pelvic-urethra reflex activity. Am J Physiol Endocrinol Metab. 2008;295:E559-568.
Winnard KP, Dmitrieva N, Berkley KJ. Cross-organ interactions between reproductive, gastrointestinal, and urinary tracts: modulation by estrous stage and involvement of the hypogastric nerve. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1592-1601.
Wesselmann U, Lai J. Mechanisms of referred visceral pain: uterine inflammation in the adult virgin rat results in neurogenic plasma extravasation in the skin. Pain. 1997;73:309–317.
Cho HS, Park JM, Lim CH et al. Anxiety, depression and quality of life in patients with irritable bowel syndrome. Gut Liver. 2011;5:29–36.
Elsenbruch S, Rosenberger C, Bingel U et al. Patients with irritable bowel syndrome have altered emotional modulation of neural responses to visceral stimuli. Gastroenterology. 2010;139:1310–1319.
Qi R, Liu C, Ke J et al. Intrinsic brain abnormalities in irritable bowel syndrome and effect of anxiety and depression. Brain Imaging Behav. 2016;10:1127–1134.
Chey WD, Kurlander J, Eswaran S. Irritable bowel syndrome: a clinical review. JAMA. 2015;313:949–958.
Quigley EMM, Fried M, Gwee K-A et al. World Gastroenterology Organisation Global Guidelines Irritable Bowel Syndrome: A Global Perspective Update September 2015. J Clin Gastroenterol. 2016;50:704–713.
Bérubé M, Martorella G, Côté C et al. The Effect of Psychological Interventions on the Prevention of Chronic Pain in Adults: A Systematic Review and Meta-analysis. Clin J Pain. 2021;37:379–395.
Gaylord SA, Palsson OS, Garland EL et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am J Gastroenterol. 2011;106:1678–1688.
Tu FF, Datta A, Atashroo D et al. Clinical profile of comorbid dysmenorrhea and bladder sensitivity: a cross-sectional analysis. Am J Obstet Gynecol. 2020;222:e1-594.e11.
Lai HH, Krieger JN, Pontari MA et al. Painful Bladder Filling and Painful Urgency are Distinct Characteristics in Men and Women with Urological Chronic Pelvic Pain Syndromes: A MAPP Research Network Study. J Urol. 2015;194:1634–1641.
Laden BF, Bresee C, De Hoedt A et al. Comorbidities in a Nationwide, Heterogenous Population of Veterans with Interstitial Cystitis/Bladder Pain Syndrome. Urology. 2021;156:37–43.
Aziz I, Törnblom H, Palsson OS et al. How the Change in IBS Criteria From Rome III to Rome IV Impacts on Clinical Characteristics and Key Pathophysiological Factors. Am J Gastroenterol. 2018;113:1017–1025.
Hahn B, Watson M, Yan S et al. Irritable Bowel Syndrome Symptom Patterns: Frequency, Duration, and Severity. Dig Dis Sci. 1998;43:2715–2718.
Prior A, Read NW. Reduction of rectal sensitivity and post-prandial motility by granisetron, a 5 HT3-receptor antagonist, in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 1993;7:175–180.
Konthapakdee N, Grundy L, O’Donnell T et al. Serotonin exerts a direct modulatory role on bladder afferent firing in mice. J Physiol. 2019;597:5247–5264.
Fukudo S, Matsueda K, Haruma K et al. Optimal dose of ramosetron in female patients with irritable bowel syndrome with diarrhea: A randomized, placebo-controlled phase II study. Neurogastroenterol Motil. 2017;29:e13023.
Juza R, Vlcek P, Mezeiova E et al. Recent advances with 5-HT3 modulators for neuropsychiatric and gastrointestinal disorders. Med Res Rev. 2020;40:1593–1678.
Acknowledgments
The authors thank Dr. G.F. Gebhart for advice and editorial assistance. They are grateful to Ellen Garrison, Katlyn Dillane, and Genevieve Roth for technical assistance. This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD098193) and the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK100368).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F.F. Tu reports personal fees from Myovant, Tremeau Pharmaceuticals, and UroShape, royalties from Wolters Kluwer, and Grant support from Dot Laboratories and Eximis outside the submitted work. The remaining authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shlobin, A.E., Tu, F.F., Sain, C.R. et al. Bladder Pain Sensitivity Is a Potential Risk Factor for Irritable Bowel Syndrome. Dig Dis Sci 68, 3092–3102 (2023). https://doi.org/10.1007/s10620-023-07868-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07868-7