Abstract
Background/Aims
Early and accurate identification of patients with acute pancreatitis (AP) at high risk of persistent acute respiratory failure (PARF) is crucial. We sought to determine the accuracy of simplified Lung Injury Prediction Score (sLIPS) and simplified Early Acute Lung Injury (sEALI) for predicting PARF in ward AP patients.
Methods
Consecutive AP patients in a training cohort from West China Hospital of Sichuan University (n = 912) and a validation cohort from The First Affiliated Hospital of Nanchang University (n = 1033) were analyzed. PARF was defined as oxygen in arterial blood/fraction of inspired oxygen < 300 mmHg that lasts for > 48 h. The sLIPS was composed by shock (predisposing condition), alcohol abuse, obesity, high respiratory rate, low oxygen saturation, high oxygen requirement, hypoalbuminemia, and acidosis (risk modifiers). The sEALI was calculated from oxygen 2 to 6 L/min, oxygen > 6 L/min, and high respiratory rate. Both indices were calculated on admission.
Results
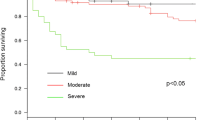
PARF developed in 16% (145/912) and 22% (228/1033) (22%) of the training and validation cohorts, respectively. In these patients, sLIPS and sEALI were significantly increased. sLIPS ≥ 2 predicted PARF in the training (AUROC 0.87, 95% CI 0.84–0.89) and validation (AUROC 0.81, 95% CI 0.78–0.83) cohorts. sLIPS was significantly more accurate than sEALI and current clinical scoring systems in both cohorts (all P < 0.05).
Conclusions
Using routinely available clinical data, the sLIPS can accurately predict PARF in ward AP patients and outperforms the sEALI and current existing clinical scoring systems.

Similar content being viewed by others
References
Mederos MA, Reber HA, Girgis MD. Acute pancreatitis: a review. JAMA 2021;325:382–390.
Banks PA, Bollen TL, Dervenis C et al. Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–111.
Crockett SD, Wani S, Gardner TB et al. American Gastroenterological Association Institute guideline on initial management of acute pancreatitis. Gastroenterology 2018;154:1096–1101.
Dellinger EP, Forsmark CE, Layer P et al. Determinant-based classification of acute pancreatitis severity an international multidisciplinary consultation. Ann Surg 2012;256:875–880.
Di MY, Liu H, Yang ZY et al. Prediction models of mortality in acute pancreatitis in adults: a systematic review. Ann Intern Med 2016;165:482–490.
Shi N, Zhang X, Zhu Y et al. Predicting persistent organ failure on admission in patients with acute pancreatitis: development and validation of a mobile nomogram. Hpb 2022.
Kui B, Pintér J, Molontay R et al. EASY‐APP: An artificial intelligence model and application for early and easy prediction of severity in acute pancreatitis. Clin Transl Med 2022;12.
Shi N, Liu TT, de la Iglesia-Garcia D et al. Duration of organ failure impacts mortality in acute pancreatitis. Gut 2020;69:604-+.
Parniczky A, Kui B, Szentesi A et al. Prospective, multicentre, nationwide clinical data from 600 cases of acute pancreatitis. PLoS ONE 2016;11.
Iyer H, Elhence A, Mittal S et al. Pulmonary complications of acute pancreatitis. Expert Rev Respir Med 2020;14:209–217.
Banks PA, Bollen TL, Dervenis C et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–111.
Dellinger EP, Forsmark CE, Layer P et al. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg 2012;256:875–880.
Zhao X, Huang W, Li J et al. Noninvasive positive-pressure ventilation in acute respiratory distress syndrome in patients with acute pancreatitis: a retrospective cohort study. Pancreas 2016;45:58–63.
Guo Q, Li A, Xia Q et al. The role of organ failure and infection in necrotizing pancreatitis: a prospective study. Ann Surg 2014;259:1201–1207.
Liu T, Huang W, Szatmary P et al. Accuracy of circulating histones in predicting persistent organ failure and mortality in patients with acute pancreatitis. Br J Surg 2017;104:1215–1225.
Schepers NJ, Bakker OJ, Besselink MG et al. Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis. Gut 2019;68:1044–1051.
Shi N, Liu T, de la Iglesia-Garcia D et al. Duration of organ failure impacts mortality in acute pancreatitis. Gut 2020;69:604–605.
Sternby H, Bolado F, Canaval-Zuleta HJ et al. Determinants of severity in acute pancreatitis: a nation-wide multicenter prospective cohort study. Ann Surg 2019;270:348–355.
Li L, Jin T, Wen S et al. Early rapid fluid therapy is associated with increased rate of noninvasive positive-pressure ventilation in hemoconcentrated patients with severe acute pancreatitis. Dig Dis Sci 2020;1, 1.
Jin T, Li L, Zhu P et al. Optimising fluid requirements after initial resuscitation: a pilot study evaluating mini-fluid challenge and passive leg raising test in patients with predicted severe acute pancreatitis. Pancreatology 2022;1.
Jin T, Li L, Deng L et al. Hemoconcentration is associated with early faster fluid rate and increased risk of persistent organ failure in acute pancreatitis patients. JGH Open 2020;4:684–691.
Beitler JR, Thompson BT, Baron RM et al. Advancing precision medicine for acute respiratory distress syndrome. Lancet Respir Med 2022;10:107–120.
Meyer NJ, Gattinoni L, Calfee CS. Acute respiratory distress syndrome. Lancet 2021;398:622–637.
Gajic O, Dabbagh O, Park PK et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med 2011;183:462–470.
Trillo-Alvarez C, Cartin-Ceba R, Kor DJ et al. Acute lung injury prediction score: derivation and validation in a population-based sample. Eur Respir J 2011;37:604–609.
Mikkelsen ME, Shah CV, Meyer NJ et al. The epidemiology of acute respiratory distress syndrome in patients presenting to the emergency department with severe sepsis. Shock 2013;40:375–381.
Kor DJ, Talmor DS, Banner-Goodspeed VM et al. Lung Injury Prevention with Aspirin (LIPS-A): a protocol for a multicentre randomised clinical trial in medical patients at high risk of acute lung injury. BMJ Open 2012;2.
Kor DJ, Warner DO, Alsara A et al. Derivation and diagnostic accuracy of the surgical lung injury prediction model. Anesthesiology 2011;115:117–128.
Levitt JE, Bedi H, Calfee CS et al. Identification of early acute lung injury at initial evaluation in an acute care setting prior to the onset of respiratory failure. Chest 2009;135:936–943.
Levitt JE, Calfee CS, Goldstein BA et al. Early acute lung injury: criteria for identifying lung injury prior to the need for positive pressure ventilation*. Crit Care Med 2013;41:1929–1937.
Esteban A, Frutos-Vivar F, Ferguson ND et al. Sepsis incidence and outcome: contrasting the intensive care unit with the hospital ward. Crit Care Med 2007;35:1284–1289.
Ferguson ND, Frutos-Vivar F, Esteban A et al. Clinical risk conditions for acute lung injury in the intensive care unit and hospital ward: a prospective observational study. Crit Care 2007;11:R96.
Quartin AA, Campos MA, Maldonado DA et al. Acute lung injury outside of the ICU: incidence in respiratory isolation on a general ward. Chest 2009;135:261–268.
Shari G, Kojicic M, Li G et al. Timing of the onset of acute respiratory distress syndrome: a population-based study. Respir Care 2011;56:576–582.
Hou PC, Elie-Turenne MC, Mitani A et al. Towards prevention of acute lung injury: frequency and outcomes of emergency department patients at-risk - a multicenter cohort study. Int J Emerg Med 2012;5:22.
Soto GJ, Kor DJ, Park PK et al. Lung injury prediction score in hospitalized patients at risk of acute respiratory distress syndrome. Crit Care Med 2016;44:2182–2191.
Gong MN, Thompson BT, Williams P et al. Clinical predictors of and mortality in acute respiratory distress syndrome: potential role of red cell transfusion. Crit Care Med 2005;33:1191–1198.
Moss M, Guidot DM, Steinberg KP et al. Diabetic patients have a decreased incidence of acute respiratory distress syndrome. Crit Care Med 2000;28:2187–2192.
Naito Y, Tsuchiya S, Ishihara S et al. Impact of preexisting pulmonary fibrosis detected on chest radiograph and CT on the development of gefitinib-related interstitial lung disease. Am J Clin Oncol 2008;31:340–344.
Iscimen R, Cartin-Ceba R, Yilmaz M et al. Risk factors for the development of acute lung injury in patients with septic shock: an observational cohort study. Crit Care Med 2008;36:1518–1522.
von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–1457.
Zheng X, Li L, Zhu Y et al. Superoxide dismutase predicts persistent circulation failure and mortality in the Early Stage of Acute Pancreatitis. Dig Dis Sci 2020;65:3551–3557.
Mounzer R, Langmead CJ, Wu BU et al. Comparison of existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Gastroenterology 2012;142:1476–82; quiz e15–16.
Antonelli M, Levy M, Andrews PJ et al. Hemodynamic monitoring in shock and implications for management. International Consensus Conference, Paris, France, 27–28 April 2006. Intensive Care Med 2007;33:575–90.
Rivers E, Nguyen B, Havstad S et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001;345:1368–1377.
Fernandez-Perez ER, Sprung J, Afessa B et al. Intraoperative ventilator settings and acute lung injury after elective surgery: a nested case control study. Thorax 2009;64:121–127.
Gong MN, Bajwa EK, Thompson BT et al. Body mass index is associated with the development of acute respiratory distress syndrome. Thorax 2010;65:44–50.
Mangialardi RJ, Martin GS, Bernard GR et al. Hypoproteinemia predicts acute respiratory distress syndrome development, weight gain, and death in patients with sepsis. Ibuprofen in Sepsis Study Group. Crit Care Med 2000;28:3137–45.
Knaus WA, Draper EA, Wagner DP et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–829.
Working Group IAPAPAAPG. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013;13:e1-15.
Higgs A, McGrath BA, Goddard C et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018;120:323–352.
Force ADT, Ranieri VM, Rubenfeld GD et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526–2533.
Huang W, Windsor JA. Fulminant or early severe acute pancreatitis is overlooked by classifications of severity. Crit Care Med 2017;45:e744–e745.
Barbour SJ, Coppo R, Zhang H et al. Evaluating a new international risk-prediction tool in IgA nephropathy. JAMA Intern Med 2019;179:942–952.
Yilmaz M, Keegan MT, Iscimen R et al. Toward the prevention of acute lung injury: protocol-guided limitation of large tidal volume ventilation and inappropriate transfusion. Crit Care Med 2007;35:1660–1066; quiz 1667.
Fernandez-Perez ER, Yilmaz M, Jenad H et al. Ventilator settings and outcome of respiratory failure in chronic interstitial lung disease. Chest 2008;133:1113–1119.
Fine MJ, Auble TE, Yealy DM et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997;336:243–250.
Liapikou A, Ferrer M, Polverino E et al. Severe community-acquired pneumonia: validation of the Infectious Diseases Society of America/American Thoracic Society guidelines to predict an intensive care unit admission. Clin Infect Dis 2009;48:377–385.
Espana PP, Capelastegui A, Gorordo I et al. Development and validation of a clinical prediction rule for severe community-acquired pneumonia. Am J Respir Crit Care Med 2006;174:1249–1256.
Villar J, Blanco J, del Campo R et al. Assessment of PaO(2)/FiO(2) for stratification of patients with moderate and severe acute respiratory distress syndrome. BMJ Open 2015;5:e006812.
Martin DS, Grocott MP. Oxygen therapy in critical illness: precise control of arterial oxygenation and permissive hypoxemia. Crit Care Med 2013;41:423–432.
Dobszai D, Matrai P, Gyongyi Z et al. Body-mass index correlates with severity and mortality in acute pancreatitis: a meta-analysis. World J Gastroenterol 2019;25:729–743.
Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet 2015;386:85–96.
Szentesi A, Farkas N, Sipos Z et al. Alcohol consumption and smoking dose-dependently and synergistically worsen local pancreas damage. Gut 2022.
Ocskay K, Vinko Z, Nemeth D et al. Hypoalbuminemia affects one third of acute pancreatitis patients and is independently associated with severity and mortality. Sci Rep 2021;11.
Sharma V, Shanti Devi T, Sharma R et al. Arterial pH, bicarbonate levels and base deficit at presentation as markers of predicting mortality in acute pancreatitis: a single-centre prospective study. Gastroenterol Rep 2014;2:226–231.
Rumbus Z, Toth E, Poto L et al. Bidirectional Relationship Between Reduced Blood pH and Acute Pancreatitis: A Translational Study of Their Noxious Combination. Front Physiol 2018;9.
Takács T, Rosztóczy A, Maléth J et al. Intraductal acidosis in acute biliary pancreatitis. Pancreatology 2013;13:333–335.
National Heart L, Blood Institute Acute Respiratory Distress Syndrome Clinical Trials N, Wiedemann HP et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006;354:2564–75.
Alpert JS, Thygesen K, Antman E et al. Myocardial infarction redefined–a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36:959–969.
Acknowledgments
TJ and LD are correspondence authors with equal contributions. These authors thank all the staff from pancreas multidisciplinary team at West China Hospital and First Affiliated Hospital of Nanchang University for their continuous support. This study was supported by Key Research and Development Project of Science and Technology Department of Sichuan Province (No. 2021YFS0250); NZ-China Strategic Research Alliance 2016 Award (Ministry of Science and Technology, China [Grant No. 2016YFE0101800], QX, TJ, WH, and LD; Health Research Council, New Zealand, ARP and JAW), and National Institute for Health Research Senior Investigator Award (RS).
Author information
Authors and Affiliations
Contributions
Study concept, design, and obtaining funding: TJ, LD, QX, and WH. Data acquisition: LL, LD, SL, XZ, WH, PZ, WW, XS, NS, LX, and NL, and YZ. Statistical analysis and interpretation of data: LL and PZ. Drafting of Manuscript: LL and WH. Important intellectual input: ARP, VKS, and RS. Critical revision of the manuscript: JAW. All authors have approved the final version of manuscript submitted.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, L., Liu, S., Zhang, X. et al. Predicting Persistent Acute Respiratory Failure in Acute Pancreatitis: The Accuracy of Two Lung Injury Indices. Dig Dis Sci 68, 2878–2889 (2023). https://doi.org/10.1007/s10620-023-07855-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07855-y