Abstract
Background
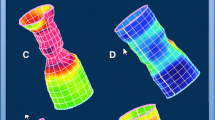
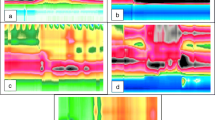
We developed a deep learning algorithm to evaluate defecatory patterns to identify dyssynergic defecation using 3-dimensional high definition anal manometry (3D-HDAM).
Aims
We developed a 3D-HDAM deep learning algorithm to evaluate for dyssynergia.
Methods
Spatial–temporal data were extracted from consecutive 3D-HDAM studies performed between 2018 and 2020 at Dartmouth-Hitchcock Health. The technical procedure and gold standard definition of dyssynergia were based on the London consensus, adapted to the needs of 3D-HDAM technology. Three machine learning models were generated: (1) traditional machine learning informed by conventional anorectal function metrics, (2) deep learning, and (3) a hybrid approach. Diagnostic accuracy was evaluated using bootstrap sampling to calculate area-under-the-curve (AUC). To evaluate overfitting, models were validated by adding 502 simulated defecation maneuvers with diagnostic ambiguity.
Results
302 3D-HDAM studies representing 1208 simulated defecation maneuvers were included (average age 55.2 years; 80.5% women). The deep learning model had comparable diagnostic accuracy [AUC 0.91 (95% confidence interval 0.89–0.93)] to traditional [AUC 0.93(0.92–0.95)] and hybrid [AUC 0.96(0.94–0.97)] predictive models in training cohorts. However, the deep learning model handled ambiguous tests more cautiously than other models; the deep learning model was more likely to designate an ambiguous test as inconclusive [odds ratio 4.21(2.78–6.38)] versus traditional/hybrid approaches.
Conclusions
Deep learning is capable of considering complex spatial–temporal information on 3D-HDAM technology. Future studies are needed to evaluate the clinical context of these preliminary findings.




Similar content being viewed by others
References
Peery AF, Crockett SD, Murphy CC et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology. 2019;156:254-272.e11. https://doi.org/10.1053/j.gastro.2018.08.063.
Sommers T, Corban C, Sengupta N et al. Emergency Department Burden of Constipation in the United States from 2006 to 2011. Am J Gastroenterol. 2015;110:572–579. https://doi.org/10.1038/ajg.2015.64.
Singh G, Lingala V, Wang H et al. Use of Health Care Resources and Cost of Care for Adults With Constipation. Clin Gastroenterol Hepatol. 2007;5:1053–1058. https://doi.org/10.1016/j.cgh.2007.04.019.
Sethi S, Mikami S, LeClair J et al. Inpatient Burden of Constipation in the United States: An Analysis of National Trends in the United States from 1997 to 2010. Am J Gastroenterol. 2014;109:250–256. https://doi.org/10.1038/ajg.2013.423.
Wald A, Bharucha AE, Limketkai B et al. ACG Clinical Guidelines: Management of Benign Anorectal Disorders. Am J Gastroenterol. 2021;116:1987–2008. https://doi.org/10.14309/ajg.0000000000001507.
Carrington EV, Heinrich H, Knowles CH et al. Methods of anorectal manometry vary widely in clinical practice: Results from an international survey. Neurogastroenterol Motil. 2017;29:e13016. https://doi.org/10.1111/nmo.13016.
Carrington EV, Heinrich H, Knowles CH et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil. 2020;32:e13679. https://doi.org/10.1111/nmo.13679.
Pannala R, Krishnan K, Melson J et al. Emerging role of artificial intelligence in GI endoscopy. Gastrointest Endosc. 2020;92:1151–1152. https://doi.org/10.1016/j.gie.2020.09.022.
Berzin TM, Parasa S, Wallace MB, Gross SA, Repici A, Sharma P. Position statement on priorities for artificial intelligence in GI endoscopy: a report by the ASGE Task Force. Gastrointest Endosc. 2020;92:951–959. https://doi.org/10.1016/j.gie.2020.06.035.
Le Berre C, Sandborn WJ, Aridhi S et al. Application of Artificial Intelligence to Gastroenterology and Hepatology. Gastroenterology. 2020;158:76-94.e2. https://doi.org/10.1053/j.gastro.2019.08.058.
Brandler J, Camilleri M. Pretest and Post-test Probabilities of Diagnoses of Rectal Evacuation Disorders Based on Symptoms, Rectal Exam, and Basic Tests: a Systematic Review. Clin Gastroenterol Hepatol. 2020;18:2479–2490. https://doi.org/10.1016/j.cgh.2019.11.049.
Ortengren AR, Ramkissoon RA, Chey WD, et al. Anorectal manometry to diagnose dyssynergic defecation: Systematic review and meta‐analysis of diagnostic test accuracy. Neurogastroenterol Motil. 2021. https://doi.org/10.1111/nmo.14137
Rao SSC, Mudipalli RS, Stessman M, Zimmerman B. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus). Neurogastroenterol Motil. 2004;16:589–596. https://doi.org/10.1111/j.1365-2982.2004.00526.x.
McInnes L, Healy J, Saul N, Großberger L. UMAP: Uniform Manifold Approximation and Projection. J Open Source Softw. 2018;3:861. https://doi.org/10.21105/joss.00861.
van der Sommen F, de Groof J, Struyvenberg M et al. Machine learning in GI endoscopy: practical guidance in how to interpret a novel field. Gut. 2020;69:2035–2045. https://doi.org/10.1136/gutjnl-2019-320466.
Lee TH, Bharucha AE. How to Perform and Interpret a High-resolution Anorectal Manometry Test. J Neurogastroenterol Motil. 2015;22:46–59. https://doi.org/10.5056/jnm15168.
Funding
Dr. Shah is supported by the AGA Research Foundation’s 2019 American Gastroenterological Association-Shire Research Scholar Award in Functional GI and Motility Disorders. Dr. Levy is supported under National Institutes of Health subaward P20GM104416.
Author information
Authors and Affiliations
Contributions
ES and JL were involved in study concept and design. CN and JC performed data extraction. JL performed statistical analysis. JL authored the initial draft of the manuscript. All authors critically revised the manuscript and approved the final copy.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Shah is a consultant for Laborie/GI Supply. Dr. Baker is a consultant for Laborie/GI Supply, Diversatek, and Medtronic. Dr. Chey is a consultant for Allergan, Biomerica, IM Health, Ironwood, Outpost, QOL Medical, Ritter, Salix, Urovant and has research grants from Commonwealth Diagnostics, Ironwood, QOL Medical, Salix, Urovant, Vibrant, and Zespri. The authors have no relevant disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (M4V 8359 kb)
Supplementary file3 (M4V 8778 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Levy, J.J., Navas, C.M., Chandra, J.A. et al. Video-Based Deep Learning to Detect Dyssynergic Defecation with 3D High-Definition Anorectal Manometry. Dig Dis Sci 68, 2015–2022 (2023). https://doi.org/10.1007/s10620-022-07759-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07759-3