Abstract
Background/Aims
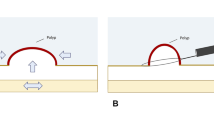
Duodenal underwater endoscopic mucosal resection (UEMR) has been suggested as a feasible treatment option for superficial non-ampullary duodenal epithelial tumors (SNADETs). However, its efficacy and safety have not been fully established yet. Thus, the objective of this systematic review and meta-analysis was to determine the efficacy and safety of UEMR as compared with conventional endoscopic mucosal resection (CEMR) in the treatment of SNADETs.
Methods
We conducted a comprehensive literature search in PubMed, EMBASE, the Cochrane Library. Studies comparing CEMR and UEMR for the resection of SNADET were included. Outcomes included en-bloc and complete resection rates, adverse events, and procedure time.
Results
A total of six studies with 2454 lesions were included in the quantitative synthesis. En-bloc and complete resection rates were not significantly different between UEMR and CEMR (OR for en-bloc resection: 0.997 [95% CI 0.439–2.266]; OR for complete resection: 0.960 [95% CI 0.628–1.468]). There was no significant risk difference for perforation (risk difference: − 0.002; 95% CI − 0.009 to 0.005) or delayed bleeding (risk difference: − 0.001; 95% CI − 0.014 to 0.011). Procedure time was significantly shorter in the UEMR (standardized mean difference: − 1.294; 95% CI − 2.461 to − 0.127). The risk of recurrence was not significantly different between UEMR and CEMR (risk difference: 0.001; 95% CI − 0.041 to 0.044).
Conclusion
Although our results did not show any superiority of UEMR over CEMR in the treatment of SNADETs, UEMR showed equivalent efficacy and safety as compared with CEMR and was associated with a shorter procedure time.






Similar content being viewed by others
References
Culver EL, McIntyre AS. Sporadic duodenal polyps: classification, investigation, and management. Endoscopy. 2011;43:144–155.
Goda K, Kikuchi D, Yamamoto Y et al. Endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors in Japan: multicenter case series. Dig Endosc. 2014;26:23–29.
Dabaja BS, Suki D, Pro B, Bonnen M, Ajani J. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004;101:518–526.
Amoyel M, Belle A, Dhooge M et al. Endoscopic management of non-ampullary duodenal adenomas. Endosc Int Open. 2022;10:E96–E108.
Navaneethan U, Hasan MK, Lourdusamy V et al. Efficacy and safety of endoscopic mucosal resection of non-ampullary duodenal polyps: a systematic review. Endosc Int Open. 2016;4:E699-708.
Fang Y, Ding X. Current status of endoscopic diagnosis and treatment for superficial non-ampullary duodenal epithelial tumors. Scand J Gastroenterol. 2021;56:604–612.
Probst A, Freund S, Neuhaus L et al. Complication risk despite preventive endoscopic measures in patients undergoing endoscopic mucosal resection of large duodenal adenomas. Endoscopy. 2020;52:847–855.
Binmoeller KF, Weilert F, Shah J, Bhat Y, Kane S. “Underwater” EMR without submucosal injection for large sessile colorectal polyps (with video). Gastrointest Endosc. 2012;75:1086–1091.
Yamashina T, Uedo N, Akasaka T et al. Comparison of underwater vs conventional endoscopic mucosal resection of intermediate-size colorectal polyps. Gastroenterology. 2019;157:e452.
Choi AY, Moosvi Z, Shah S et al. Underwater versus conventional EMR for colorectal polyps: systematic review and meta-analysis. Gastrointest Endosc. 2021;93:378–389.
Kiguchi Y, Kato M, Nakayama A et al. Feasibility study comparing underwater endoscopic mucosal resection and conventional endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumor < 20 mm. Dig Endosc. 2020;32:753–760.
Bhogal N, Mohan B, Chandan S et al. Efficacy and safety of underwater endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumors: a systematic review and meta-analysis. Ann Gastroenterol. 2020;33:379–384.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Kim SY, Park JE, Lee YJ et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66:408–414.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). 2022.
Furukawa M, Mitoro A, Ozutumi T et al. Efficacy of underwater endoscopic mucosal resection for superficial non-ampullary duodenal epithelial tumor. Clin Endosc. 2021;54:371–378.
Hirasawa K, Ozeki Y, Sawada A et al. Appropriate endoscopic treatment selection and surveillance for superficial non-ampullary duodenal epithelial tumors. Scand J Gastroenterol. 2021;56:342–350.
Kato M, Takeuchi Y, Hoteya S et al. Outcomes of endoscopic resection for superficial duodenal tumors: 10 years’ experience in 18 Japanese high volume centers. Endoscopy. 2021;54:663–670.
Okimoto K, Maruoka D, Matsumura T et al. Utility of underwater EMR for nonpolypoid superficial nonampullary duodenal epithelial tumors ≤20 mm. Gastrointest Endosc. 2022;95:140–148.
Toya Y, Endo M, Yamazato M et al. Resectability of underwater endoscopic mucosal resection for duodenal tumor: a single-center, retrospective pilot study. J Gastroenterol Hepatol. 2021;36:3191–3195.
Gaspar JP, Stelow EB, Wang AY. Approach to the endoscopic resection of duodenal lesions. World J Gastroenterol. 2016;22:600–617.
Kim HK, Chung WC, Lee BI, Cho YS. Efficacy and long-term outcome of endoscopic treatment of sporadic nonampullary duodenal adenoma. Gut Liver. 2010;4:373–377.
Tomizawa Y, Ginsberg GG. Clinical outcome of EMR of sporadic, nonampullary, duodenal adenomas: a 10-year retrospective. Gastrointest Endosc. 2018;87:1270–1278.
Shibagaki K, Ishimura N, Kinoshita Y. Endoscopic submucosal dissection for duodenal tumors. Ann Transl Med. 2017;5:188.
Yamamoto H, Miura Y. Duodenal ESD: conquering difficulties. Gastrointest Endosc Clin N Am. 2014;24:235–244.
Perez-Cuadrado-Robles E, Queneherve L, Margos W et al. ESD versus EMR in non-ampullary superficial duodenal tumors: a systematic review and meta-analysis. Endosc Int Open. 2018;6:E998–E1007.
Watanabe D, Hayashi H, Kataoka Y et al. Efficacy and safety of endoscopic submucosal dissection for non-ampullary duodenal polyps: a systematic review and meta-analysis. Dig Liver Dis. 2019;51:774–781.
Zhang X, Ly EK, Nithyanand S et al. Learning curve for endoscopic submucosal dissection with an untutored, prevalence-based approach in the United States. Clin Gastroenterol Hepatol. 2020;18:e581.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest or financial relationships relevant to this study to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10620_2022_7715_MOESM1_ESM.tif
Supplementary file1 Figure S1. Summary of results from Risk of Bias Assessment Tool for Nonrandomized Studies (RoBANS). (TIF 46173 kb)
Appendix 1: Detailed Literature Search Strategy
Appendix 1: Detailed Literature Search Strategy
PubMed
((underwater endoscopic resection) OR (underwater endoscopic mucosal resection) OR (underwater EMR) OR “UEMR” OR “U-EMR” OR “UW-EMR”) AND ((duoden*) OR (non-ampullary) OR (nonampullary) OR (small bowel)) AND ((polyp*) OR (neoplas*) OR (tumor*) OR (adenoma*) OR (carcinoma*) OR (lesion*)) AND (English[Language]).
Embase
-
1.
(underwater endoscopic resection or underwater endoscopic mucosal resection or underwater EMR or “UEMR” or “U-EMR” or “UW-EMR”).af.
-
2.
(duoden* or non-ampullary or nonampullary or small bowel).af.
-
3.
(polyp* or neoplas* or tumor* or adenoma* or carcinoma* or lesion*).af.
-
4.
1 and 2 and 3
Cochrane Library
#1 (underwater endoscopic resection or underwater endoscopic mucosal resection or underwater EMR or “UEMR” or “U-EMR” or “UW-EMR”).
#2 (duoden* or non-ampullary or nonampullary or small bowel).
#3 (polyp* or neoplas* or tumor* or adenoma* or carcinoma* or lesion*).
#4 #1 and #2 and #3.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, J.G., Lee, S.P., Jang, H.J. et al. Underwater Versus Conventional Endoscopic Mucosal Resection for Superficial Non-ampullary Duodenal Epithelial Tumors: A Systematic Review and Meta-Analysis. Dig Dis Sci 68, 1482–1491 (2023). https://doi.org/10.1007/s10620-022-07715-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07715-1