Abstract
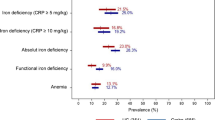
Iron deficiency anemia affects approximately 45% of patients with inflammatory bowel disease (IBD), negatively impacts the quality of life in this patient population, and significantly burdens our healthcare system. The pathogenesis of iron deficiency in IBD patients is multifactorial, including intestinal bleeding, malabsorption, and inadequate oral intake. Regular screening and diagnosis in these patients are imperative, and often patients have mixed iron deficiency anemia and anemia of chronic disease, especially in those with active inflammation. Iron may be replenished either orally or intravenously. While oral iron is safe, affordable, and easy to administer, patients often suffer from intolerable gastrointestinal side effects, and particularly in IBD patients, oral iron may increase inflammation and contribute to flares. Therefore, although it is substantially underused, intravenous (IV) iron is considered first-line treatment for patients with active disease, severe anemia, oral iron intolerance, and erythropoietin requirements. Several IV iron formulations are available, and iron sucrose and ferric carboxymaltose are the most frequently used and well studied in patients with IBD. However, iron isomaltoside could potentially become a popular choice among providers given its safety, efficacy, and convenience. Overall, screening, diagnosis, and treatment of iron deficiency anemia are important in patients with IBD. Individual patient characteristics, risks, and benefits, and advantages and disadvantages, should be considered when determining the best route and formulation for iron repletion.

Similar content being viewed by others
References
Ott C, Schölmerich J. Extraintestinal manifestations and complications in IBD. Nat Rev Gastroenterol Hepatol. 2013;10:585–595.
Patel D, Trivedi C, Khan N. Management of anemia in patients with inflammatory bowel disease (IBD). Curr Treat Options Gastroenterol. 2018;16:112–128.
Gisbert JP, Gomollón F. Common misconceptions in the diagnosis and management of anemia in inflammatory bowel disease. Am J Gastroenterol. 2008;103:1299–1307.
Hou JK, Gasche C, Drazin NZ et al. Assessment of gaps in care and the development of a care pathway for anemia in patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2017;23:35–43.
Blaney H, Vu P, Mathew A et al. Anemia severity associated with increased healthcare utilization and costs in inflammatory bowel disease. Dig Dis Sci. 2021;66:2555–2563.
Akpınar H, Çetiner M, Keshav S, Örmeci N, Törüner M. Diagnosis and treatment of iron deficiency anemia in patients with inflammatory bowel disease and gastrointestinal bleeding: iron deficiency anemia working group consensus report. Turk J Gastroenterol. 2017;28:81–87.
Danese S, Hoffman C, Vel S et al. Anaemia from a patient perspective in inflammatory bowel disease: results from the European Federation of Crohn’s and Ulcerative Colitis Association’s online survey. Eur J Gastroenterol Hepatol. 2014;26:1385–1391.
Al-Naseem A, Sallam A, Choudhury S, Thachil J. Iron deficiency without anaemia: a diagnosis that matters. Clin Med (Lond). 2021;21:107–113.
Rieder F, Paul G, Schnoy E et al. Hemoglobin and hematocrit levels in the prediction of complicated Crohn’s disease behavior–a cohort study. PLoS ONE. 2014;9:e104706.
Nairz M, Theurl I, Wolf D, Weiss G. Iron deficiency or anemia of inflammation?: Differential diagnosis and mechanisms of anemia of inflammation. Wien Med Wochenschr. 2016;166:411–423.
Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021;397:233–248.
Braunstein E. Iron deficiency anemia. In: Merck manual professional version. Merck Publishing; 2021.
González Alayón C, Pedrajas Crespo C, Marín Pedrosa S et al. Prevalence of iron deficiency without anaemia in inflammatory bowel disease and impact on health-related quality of life. Gastroenterol Hepatol. 2018;41:22–29.
DeLoughery TG. Iron deficiency anemia. Med Clin North Am. 2017;101:319–332.
Dignass AU, Gasche C, Bettenworth D et al. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J Crohns Colitis. 2015;9:211–222.
Bergamaschi G, Di Sabatino A, Albertini R, et al. Prevalence and pathogenesis of anemia in inflammatory bowel disease. Influence of anti-tumor necrosis factor-alpha treatment. Haematologica. 2010;95(2):199–205.
Shin DH, Kim HS, Park MJ, Suh IB, Shin KS. Utility of access soluble transferrin receptor (sTfR) and sTfR/log Ferritin Index in diagnosing iron deficiency anemia. Ann Clin Lab Sci. 2015;45:396–402.
Infusino I, Braga F, Dolci A, Panteghini M. Soluble transferrin receptor (sTfR) and sTfR/log ferritin index for the diagnosis of iron-deficiency anemia A meta-analysis. Am J Clin Pathol. 2012;138:642–649.
Gasche C, Berstad A, Befrits R et al. Guidelines on the diagnosis and management of iron deficiency and anemia in inflammatory bowel diseases. Inflamm Bowel Dis. 2007;13:1545–1553.
Shah Y, Patel D, Khan N. Iron deficiency anemia in IBD: an overlooked comorbidity. Expert Rev Gastroenterol Hepatol. 2021;15:771–781.
Khan N, Patel D, Trivedi C et al. Incidence of acute myeloid leukemia and myelodysplastic syndrome in patients with inflammatory bowel disease and the impact of thiopurines on their risk. Am J Gastroenterol. 2021;116:741–747.
Guagnozzi D, Lucendo AJ. Anemia in inflammatory bowel disease: a neglected issue with relevant effects. World J Gastroenterol. 2014;20:3542–3551.
Subramaniam K, D’Rozario J, Pavli P. Lymphoma and other lymphoproliferative disorders in inflammatory bowel disease: a review. J Gastroenterol Hepatol. 2013;28:24–30.
Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS ONE. 2015;10:e0117383.
Nielsen OH, Ainsworth M, Coskun M, Weiss G. Management of iron-deficiency anemia in inflammatory bowel disease: a systematic review. Medicine (Baltimore). 2015;94:e963.
Kulnigg S, Stoinov S, Simanenkov V et al. A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose (FERINJECT) randomized controlled trial. Am J Gastroenterol. 2008;103:1182–1192.
Tulewicz-Marti E, Moniuszko A, Rydzewska G. Management of anemia in inflammatory bowel disease: a challenge in everyday clinical practice. Prz Gastroenterol. 2017;12:239–243.
Tsiolakidou G, Koutroubakis IE. Stimulating erythropoiesis in inflammatory bowel disease associated anemia. World J Gastroenterol. 2007;13:4798–4806.
Werner T, Wagner SJ, Martínez I et al. Depletion of luminal iron alters the gut microbiota and prevents Crohn’s disease-like ileitis. Gut. 2011;60:325–333.
Zimmermann MB, Chassard C, Rohner F et al. The effects of iron fortification on the gut microbiota in African children: a randomized controlled trial in Cote d’Ivoire. Am J Clin Nutr. 2010;92:1406–1415.
Bhandari S, Pereira DIA, Chappell HF, Drakesmith H. Intravenous irons: from basic science to clinical practice. Pharmaceuticals (Basel). 2018;11(3).
Nielsen OH, Soendergaard C, Vikner ME, Weiss G. Rational management of iron-deficiency anaemia in inflammatory bowel disease. Nutrients. 2018;10(1).
Gasche C, Ahmad T, Tulassay Z et al. Ferric maltol is effective in correcting iron deficiency anemia in patients with inflammatory bowel disease: results from a phase-3 clinical trial program. Inflamm Bowel Dis. 2015;21:579–588.
Santiago P. Ferrous versus ferric oral iron formulations for the treatment of iron deficiency: a clinical overview. ScientificWorldJournal. 2012;2012:846824.
Moretti D, Goede JS, Zeder C et al. Oral iron supplements increase hepcidin and decrease iron absorption from daily or twice-daily doses in iron-depleted young women. Blood. 2015;126:1981–1989.
Stoffel NU, Cercamondi CI, Brittenham G et al. Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials. Lancet Haematol. 2017;4:e524–e533.
Stoffel NU, Zeder C, Brittenham GM, Moretti D, Zimmermann MB. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica. 2020;105:1232–1239.
Li N, Zhao G, Wu W et al. The efficacy and safety of vitamin c for iron supplementation in adult patients with iron deficiency anemia: a randomized clinical trial. JAMA Netw Open. 2020;3:e2023644.
Cancelo-Hidalgo MJ, Castelo-Branco C, Palacios S et al. Tolerability of different oral iron supplements: a systematic review. Curr Med Res Opin. 2013;29:291–303.
D'Amico F, Peyrin-Biroulet L, Danese S. Oral iron for IBD patients: lessons learned at time of COVID-19 pandemic. J Clin Med. 2020;9(5).
Schmidt C, Ahmad T, Tulassay Z et al. Ferric maltol therapy for iron deficiency anaemia in patients with inflammatory bowel disease: long-term extension data from a Phase 3 study. Aliment Pharmacol Ther. 2016;44:259–270.
Kumar A, Brookes MJ. Iron therapy in inflammatory bowel disease. Nutrients. 2020;12(11).
Abbati G, Incerti F, Boarini C et al. Safety and efficacy of sucrosomial iron in inflammatory bowel disease patients with iron deficiency anemia. Intern Emerg Med. 2019;14:423–431.
Auerbach M. Treatment of iron deficiency anemia in adults. In: Robert Means WM, Jennifer Tirnauer, Lisa Kunins, ed. UpToDate.2022.
Bonovas S, Fiorino G, Allocca M et al. Intravenous versus oral iron for the treatment of anemia in inflammatory bowel disease: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2016;95:e2308.
Lee TW, Kolber MR, Fedorak RN, van Zanten SV. Iron replacement therapy in inflammatory bowel disease patients with iron deficiency anemia: a systematic review and meta-analysis. J Crohns Colitis. 2012;6:267–275.
Avni T, Bieber A, Steinmetz T, Leibovici L, Gafter-Gvili A. Treatment of anemia in inflammatory bowel disease–systematic review and meta-analysis. PLoS ONE. 2013;8:e75540.
Kletzmayr J, Sunder-Plassmann G, Hörl WH. High dose intravenous iron: a note of caution. Nephrol Dial Transplant. 2002;17:962–965.
Ishida JH, Marafino BJ, McCulloch CE et al. Receipt of intravenous iron and clinical outcomes among hemodialysis patients hospitalized for Infection. Clin J Am Soc Nephrol. 2015;10:1799–1805.
Sullivan JL. Iron therapy and cardiovascular disease. Kidney Int Suppl. 1999;69:S135-137.
Del Vecchio L, Ekart R, Ferro CJ et al. Intravenous iron therapy and the cardiovascular system: risks and benefits. Clin Kidney J. 2021;14:1067–1076.
Macdougall IC, White C, Anker SD et al. Intravenous iron in patients undergoing maintenance hemodialysis. N Engl J Med. 2019;380:447–458.
Ganzoni AM. Intravenous iron-dextran: therapeutic and experimental possibilities. Schweiz Med Wochenschr. 1970;100:301–303.
Evstatiev R, Marteau P, Iqbal T, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141(3):846–853.e841–842.
Favrat B, Balck K, Breymann C et al. Evaluation of a single dose of ferric carboxymaltose in fatigued, iron-deficient women–PREFER a randomized, placebo-controlled study. PLoS ONE. 2014;9:e94217.
Niepel D, Klag T, Malek NP, Wehkamp J. Practical guidance for the management of iron deficiency in patients with inflammatory bowel disease. Therap Adv Gastroenterol. 2018;11:1756284818769074.
Chertow GM, Mason PD, Vaage-Nilsen O, Ahlmén J. On the relative safety of parenteral iron formulations. Nephrol Dial Transplant. 2004;19:1571–1575.
Chertow GM, Mason PD, Vaage-Nilsen O, Ahlmén J. Update on adverse drug events associated with parenteral iron. Nephrol Dial Transplant. 2006;21:378–382.
Stein J, Dignass AU. Management of iron deficiency anemia in inflammatory bowel disease—a practical approach. Ann Gastroenterol. 2013;26:104–113.
Lindgren S, Wikman O, Befrits R et al. Intravenous iron sucrose is superior to oral iron sulphate for correcting anaemia and restoring iron stores in IBD patients: a randomized, controlled, evaluator-blind, multicentre study. Scand J Gastroenterol. 2009;44:838–845.
Muñoz M, Villar I, García-Erce JA. An update on iron physiology. World J Gastroenterol. 2009;15:4617–4626.
Schröder O, Mickisch O, Seidler U et al. Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease–a randomized, controlled, open-label, multicenter study. Am J Gastroenterol. 2005;100:2503–2509.
Evstatiev R, Alexeeva O, Bokemeyer B et al. Ferric carboxymaltose prevents recurrence of anemia in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2013;11:269–277.
Kaitha S, Bashir M, Ali T. Iron deficiency anemia in inflammatory bowel disease. World J Gastrointest Pathophysiol. 2015;6:62–72.
Briot K, Geusens P, Em Bultink I, Lems WF, Roux C. Inflammatory diseases and bone fragility. Osteoporos Int. 2017;28:3301–3314.
Schaefer B, Zoller H, Wolf M. Risk factors for and effects of persistent and severe hypophosphatemia following ferric carboxymaltose. J Clin Endocrinol Metab. 2021.
Tozzi D, Tozzi J. Osteomalacia and insufficiency fractures secondary to intravenous iron therapy: a case report. J Orthop Case Rep. 2020;10:4–7.
Callejas-Moraga EL, Casado E, Gomez-Nuñez M, Caresia-Aroztegui AP. Severe osteomalacia with multiple insufficiency fractures secondary to intravenous iron therapy in a patient with Rendu-Osler-Weber syndrome. Bone Rep. 2020;13:100712.
Klein K, Asaad S, Econs M, Rubin JE. Severe FGF23-based hypophosphataemic osteomalacia due to ferric carboxymaltose administration. BMJ Case Rep. 2018;2018.
Silverstein SB, Rodgers GM. Parenteral iron therapy options. Am J Hematol. 2004;76:74–78.
Ford DC, Dahl NV, Strauss WE et al. Ferumoxytol versus placebo in iron deficiency anemia: efficacy, safety, and quality of life in patients with gastrointestinal disorders. Clin Exp Gastroenterol. 2016;9:151–162.
Bailie GR. Comparison of rates of reported adverse events associated with i.v. iron products in the United States. Am J Health Syst Pharm. 2012;69(4):310–320.
Bruining DH, Loftus EV. Technology insight: new techniques for imaging the gut in patients with IBD. Nat Clin Pract Gastroenterol Hepatol. 2008;5:154–161.
McCullough BJ, Kolokythas O, Maki JH, Green DE. Ferumoxytol in clinical practice: implications for MRI. J Magn Reson Imaging. 2013;37:1476–1479.
Auerbach M, Henry D, DeLoughery TG. Intravenous ferric derisomaltose for the treatment of iron deficiency anemia. Am J Hematol. 2021;96:727–734.
Dahlerup JF, Jacobsen BA, van der Woude J, Bark L, Thomsen LL, Lindgren S. High-dose fast infusion of parenteral iron isomaltoside is efficacious in inflammatory bowel disease patients with iron-deficiency anaemia without profound changes in phosphate or fibroblast growth factor 23. Scand J Gastroenterol. 2016;51:1332–1338.
Stein J, Walper A, Klemm W, Farrag K, Aksan A, Dignass A. Safety and efficacy of intravenous iron isomaltoside for correction of anaemia in patients with inflammatory bowel disease in everyday clinical practice. Scand J Gastroenterol. 2018;53:1059–1065.
Sam K, Khan AI, Khan A, et al. Efficacy and safety of ferric derisomaltose/iron isomaltoside in patients with inflammatory bowel disease: a systematic review. In. Vol 138: Blood; 2021.
Detlie TE, Lindstrøm JC, Jahnsen ME et al. Incidence of hypophosphatemia in patients with inflammatory bowel disease treated with ferric carboxymaltose or iron isomaltoside. Aliment Pharmacol Ther. 2019;50:397–406.
Aksan A, Işık H, Radeke HH, Dignass A, Stein J. Systematic review with network meta-analysis: comparative efficacy and tolerability of different intravenous iron formulations for the treatment of iron deficiency anaemia in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2017;45:1303–1318.
Auerbach M, Gafter-Gvili A, Macdougall IC. Intravenous iron: a framework for changing the management of iron deficiency. Lancet Haematol. 2020;7:e342–e350.
Hambley BC, Anderson KE, Shanbhag SP, Sen AP, Anderson G. Payment incentives and the use of higher-cost drugs: a retrospective cohort analysis of intravenous iron in the Medicare population. Am J Manag Care. 2020;26:516–522.
Moreno López R, Sicilia Aladrén B, Gomollón García F. Use of agents stimulating erythropoiesis in digestive diseases. World J Gastroenterol. 2009;15:4675–4685.
Gasche C, Waldhoer T, Feichtenschlager T et al. Prediction of response to iron sucrose in inflammatory bowel disease-associated anemia. Am J Gastroenterol. 2001;96:2382–2387.
Skikne BS, Cook JD. Effect of enhanced erythropoiesis on iron absorption. J Lab Clin Med. 1992;120:746–751.
Carson JL, Stanworth SJ, Alexander JH et al. Clinical trials evaluating red blood cell transfusion thresholds: an updated systematic review and with additional focus on patients with cardiovascular disease. Am Heart J. 2018;200:96–101.
García-Erce JA, Gomollón F, Muñoz M. Blood transfusion for the treatment of acute anaemia in inflammatory bowel disease and other digestive diseases. World J Gastroenterol. 2009;15:4686–4694.
Mei Z, Cogswell ME, Looker AC et al. Assessment of iron status in US pregnant women from the National Health and Nutrition Examination Survey (NHANES), 1999–2006. Am J Clin Nutr. 2011;93:1312–1320.
Auerbach M. Commentary: iron deficiency of pregnancy—a new approach involving intravenous iron. Reprod Health. 2018;15:96.
Mahadevan U, Robinson C, Bernasko N et al. Inflammatory bowel disease in pregnancy clinical care pathway: a report from the American gastroenterological association IBD parenthood project working group. Inflamm Bowel Dis. 2019;25:627–641.
Achebe MM, Gafter-Gvili A. How I treat anemia in pregnancy: iron, cobalamin, and folate. Blood. 2017;129:940–949.
Kitsati N, Liakos D, Ermeidi E et al. Rapid elevation of transferrin saturation and serum hepcidin concentration in hemodialysis patients after intravenous iron infusion. Haematologica. 2015;100:e80-83.
Kulnigg S, Teischinger L, Dejaco C, Waldhör T, Gasche C. Rapid recurrence of IBD-associated anemia and iron deficiency after intravenous iron sucrose and erythropoietin treatment. Am J Gastroenterol. 2009;104:1460–1467.
Jimenez KM, Gasche C. Management of iron deficiency anaemia in inflammatory bowel disease. Acta Hematol. 2019;142:30–36.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maas, L.A., Krishna, M. & Parian, A.M. Ironing It All Out: A Comprehensive Review of Iron Deficiency Anemia in Inflammatory Bowel Disease Patients. Dig Dis Sci 68, 357–369 (2023). https://doi.org/10.1007/s10620-022-07599-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07599-1