Abstract
Introduction
The role of anorectal and defecatory dysfunction in opioid-related constipation is unclear. We aimed to evaluate the relationship between opioid use and rectal sensation, defecatory function, and balloon expulsion on anorectal physiology testing.
Methods
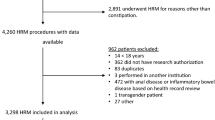
This was a retrospective cohort study of consecutive adults undergoing high-resolution anorectal manometry (HRAM) at a tertiary center for constipation. Clinical characteristics, medication use, and HRAM findings were obtained. Statistical analyses were performed using Fisher-exact/student t-test for univariate analyses and logistic/general linear regression for multivariable analyses to compare patients with no opioid use, recent (< 3 months) use, and distant (> 3 months) use.
Results
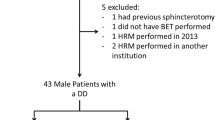
424 patients (49.8 ± 17.2 years; 85.6% female) were included. Compared to those without opioid history, patients with recent use had increased volumes for first rectal sensation (70.4 mL vs 59.4, p = 0.043), urge (120.5 mL vs 101.5, p = 0.017), and maximal tolerance (170.2 mL vs 147.2, p = 0.0018), but not patients with distant use. Recent opioid use was associated with increased risk of dyssynergic defecation (DD) (61.8% vs 46.4%, p = 0.035), but not failed balloon expulsion. On multivariable models controlling for potential confounders, recent opioid use, but not distant use, remained independently correlated with increased volumes for first rectal sensation (β-coefficient 9.78, p = 0.019), urge (β-coefficient 16.7, p = 0.0060), and maximal tolerance (β-coefficient 22.9, p = 0.0032), and higher risk for DD (aOR = 2.18, p = 0.026).
Conclusion
Recent opioid use was an independent risk factor for rectal hyposensitivity and DD on HRAM in patients with constipation, but that effect may decrease with discontinuation of use. Anorectal physiology testing should be considered in patients with opioid-associated constipation.


Similar content being viewed by others
References
Kiang MV, Humphreys K, Cullen MR, Basu S. Opioid prescribing patterns among medical providers in the United States, 2003–17: retrospective, observational study. BMJ 2020;368:l6968. https://doi.org/10.1136/bmj.l6968.
Levy B, Paulozzi L, Mack KA, Jones CM. Trends in Opioid Analgesic-Prescribing Rates by Specialty, U.S., 2007–2012. Am J Prev Med 2015;49(3):409–13. DOI: https://doi.org/10.1016/j.amepre.2015.02.020.
Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician 2008;11(2 Suppl):S105–20. (https://www.ncbi.nlm.nih.gov/pubmed/18443635).
Crockett SD, Greer KB, Heidelbaugh JJ et al. American Gastroenterological Association Institute Guideline on the Medical Management of Opioid-Induced Constipation. Gastroenterology 2019;156:218–226. https://doi.org/10.1053/j.gastro.2018.07.016.
Muller-Lissner S, Bassotti G, Coffin B et al. Opioid-Induced Constipation and Bowel Dysfunction: A Clinical Guideline. Pain Med 2017;18:1837–1863. https://doi.org/10.1093/pm/pnw255.
Andresen V, Banerji V, Hall G, Lass A, Emmanuel AV. The patient burden of opioid-induced constipation: New insights from a large, multinational survey in five European countries. United European Gastroenterol J 2018;6:1254–1266. https://doi.org/10.1177/2050640618786145.
Ducrotte P, Milce J, Soufflet C, Fabry C. Prevalence and clinical features of opioid-induced constipation in the general population: A French study of 15,000 individuals. United European Gastroenterol J 2017;5:588–600. https://doi.org/10.1177/2050640616659967.
Burleigh DE, D'Mello A. Neural and pharmacologic factors affecting motility of the internal anal sphincter. Gastroenterology 1983;84(2):409–17. (https://www.ncbi.nlm.nih.gov/pubmed/6336709).
Bouvier M, Kirschner G, Gonella J. Actions of morphine and enkephalins on the internal anal sphincter of the cat: relevance for the physiological role of opiates. J Auton Nerv Syst 1986;16:219–232. https://doi.org/10.1016/0165-1838(86)90028-7.
Ratuapli SK, Crowell MD, DiBaise JK et al. Opioid-Induced Esophageal Dysfunction (OIED) in Patients on Chronic Opioids. Am J Gastroenterol 2015;110:979–984. https://doi.org/10.1038/ajg.2015.154.
Mehendale SR, Yuan CS. Opioid-induced gastrointestinal dysfunction. Dig Dis 2006;24:105–112. https://doi.org/10.1159/000090314.
Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1). Pain Med 2009;10:35–42. https://doi.org/10.1111/j.1526-4637.2008.00495.x.
Fallon MT, Hanks GW. Morphine, constipation and performance status in advanced cancer patients. Palliat Med 1999;13:159–160. https://doi.org/10.1191/026921699677653615.
Candrilli SD, Davis KL, Iyer S. Impact of constipation on opioid use patterns, health care resource utilization, and costs in cancer patients on opioid therapy. J Pain Palliat Care Pharmacother 2009;23:231–241. https://doi.org/10.1080/15360280903098440.
Sternini C, Patierno S, Selmer IS, Kirchgessner A. The opioid system in the gastrointestinal tract. Neurogastroenterol Motil 2004;16:3–16. https://doi.org/10.1111/j.1743-3150.2004.00553.x.
Galligan JJ, Sternini C. Insights into the Role of Opioid Receptors in the GI Tract: Experimental Evidence and Therapeutic Relevance. Handb Exp Pharmacol 2017;239:363–378. https://doi.org/10.1007/164_2016_116.
Farmer AD, Holt CB, Downes TJ, Ruggeri E, Del Vecchio S, De Giorgio R. Pathophysiology, diagnosis, and management of opioid-induced constipation. Lancet Gastroenterol Hepatol 2018;3:203–212. https://doi.org/10.1016/S2468-1253(18)30008-6.
Mearin F, Lacy BE, Chang L et al. Bowel Disorders. Gastroenterology. 2016. https://doi.org/10.1053/j.gastro.2016.02.031.
Lembo T, Naliboff BD, Matin K et al. Irritable bowel syndrome patients show altered sensitivity to exogenous opioids. Pain 2000;87:137–147. https://doi.org/10.1016/s0304-3959(00)00282-7.
Vollebregt PF, Hooper RL, Farmer AD, Miller J, Knowles CH, Scott SM. Association between opioid usage and rectal dysfunction in constipation: A cross-sectional study of 2754 patients. Neurogastroenterol Motil 2020:e13839. DOI: https://doi.org/10.1111/nmo.13839.
Farmer AD, Drewes AM, Chiarioni G et al. Pathophysiology and management of opioid-induced constipation: European expert consensus statement. United European Gastroenterol J 2019;7:7–20. https://doi.org/10.1177/2050640618818305.
Hanson B, Siddique SM, Scarlett Y, Sultan S, American Gastroenterological Association Institute Clinical Guidelines C. American Gastroenterological Association Institute Technical Review on the Medical Management of Opioid-Induced Constipation. Gastroenterology 2019;156(1):229–253 e5. DOI: https://doi.org/10.1053/j.gastro.2018.08.018.
Besendorfer M, Kohl M, Schellerer V, Carbon R, Diez S. A Pilot Study of Non-invasive Sacral Nerve Stimulation in Treatment of Constipation in Childhood and Adolescence. Front Pediatr 2020;8:169. https://doi.org/10.3389/fped.2020.00169.
Jiang L, Zhang N, Zhang S, Chen JD. Sacral nerve stimulation with optimized parameters improves visceral hypersensitivity in rats mediated via the autonomic pathway. Mol Pain 2019;15:1744806919880651. https://doi.org/10.1177/1744806919880651.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
Study concept and design–NAL, AHG, WWC, Data Acquisition–NAL, LH, AHG, WWC, Paper preparation, and statistical analysis–NAL, WWC, Critical revisions–NAL, LH, AHG, WWC, Administrative support, and overall study supervision–WWC.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This Study Was presented as an oral abstract during the American College of Gastroenterology 2019 Annual Scientific Meeting.
Rights and permissions
About this article
Cite this article
Lodhia, N.A., Horton, L., Thapa, N. et al. Opioid-Associated Anorectal Dysfunction in Chronic Constipation. Dig Dis Sci 67, 3904–3910 (2022). https://doi.org/10.1007/s10620-021-07288-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07288-5