Abstract
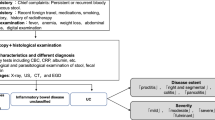
Background
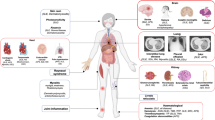
Patients with inflammatory bowel disease (IBD) may present extraintestinal manifestations (EIMs) that affect the joints, skin, eyes, and hepatobiliary area, among others.
Aims
Our aim was to analyse the prevalence and characteristics of EIMs in patients with IBD and to identify the possible risk factors associated with the development of EIMs in the largest series published to date.
Methods
Observational, cross-sectional study including patients from the Spanish ENEIDA registry promoted by GETECCU. We retrospectively identified all cases of EIMs in the ENEIDA registry until January 2018.
Results
The study included 31,077 patients, 5779 of whom had at least one EIM (global prevalence 19%; 95% CI 18.2–19.0). Among the different types of EIMs, rheumatic manifestations had a prevalence of 13% (95% CI 12.9–13.7; 63% of EIMs), with a prevalence of 5% (95% CI 4.7–5.2) for mucocutaneous manifestations, 2.1% (95% CI 1.9–2.2) for ocular manifestations, and 0.7% (95% CI 0.6–0.8) for hepatobiliary manifestations. The multivariable analysis showed that the type of IBD (Crohn’s disease, p < 0.001), gender (female, p < 0.001), the need for an immunomodulator (p < 0.001) or biologic drugs (p < 0.001), a previous family history of IBD (p < 0.001), and an extensive location of IBD (p < 0.001) were risk factors for the presence of EIMs.
Conclusions
One-fifth of patients with IBD may have associated EIMs, with rheumatic manifestations as the most frequent (> 60% of EIMs). Female patients with severe Crohn’s disease represent the group with the highest risk of developing EIMs. These patients should therefore be specially monitored and referred to the corresponding specialist when suggestive symptoms appear.

Similar content being viewed by others
References
Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohn’s Colitis. 2017;11:649–670. https://doi.org/10.1093/ecco-jcc/jjx008.
Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 2—surgical management and special situations. J Crohn’s Colitis. 2017;11:135–149. https://doi.org/10.1093/ecco-jcc/jjw169.
Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1982–1992. https://doi.org/10.1097/MIB.0000000000000392.
Karmiris K, Avgerinos A, Tavernaraki A, et al. Prevalence and characteristics of extra-intestinal manifestations in a large cohort of Greek patients with inflammatory bowel disease. J Crohn’s Colitis. 2016;10:429–436. https://doi.org/10.1093/ecco-jcc/jjv232.
Repiso A, Alcantara M, Munoz-Rosas C, et al. Extraintestinal manifestations of Crohn’s disease: prevalence and related factors. Revista espanola de enfermedades digestivas: organo oficial de la Sociedad Espanola de Patologia Digestiva. 2006;98:510–517.
Vavricka SR, Rogler G, Gantenbein C, et al. Chronological order of appearance of extraintestinal manifestations relative to the time of IBD diagnosis in the Swiss inflammatory bowel disease cohort. Inflamm Bowel Dis. 2015;21:1794–1800. https://doi.org/10.1097/MIB.0000000000000429.
Greuter T, Vavricka SR. Extraintestinal manifestations in inflammatory bowel disease—epidemiology, genetics, and pathogenesis. Expert Rev Gastroenterol Hepatol. 2019;13:307–317. https://doi.org/10.1080/17474124.2019.1574569.
Ardizzone S, Puttini PS, Cassinotti A, Porro GB. Extraintestinal manifestations of inflammatory bowel disease. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2008;40:S253–S259. https://doi.org/10.1016/S1590-8658(08)60534-4.
Mendoza JL, Lana R, Taxonera C, Alba C, Izquierdo S, Diaz-Rubio M. Extraintestinal manifestations in inflammatory bowel disease: differences between Crohn’s disease and ulcerative colitis. Med Clin. 2005;125:297–300.
Sturm A, Maaser C, Calabrese E, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 2: IBD scores and general principles and technical aspects. J Crohn’s Colitis. 2019;13:273–284. https://doi.org/10.1093/ecco-jcc/jjy114.
Greenstein AJ, Janowitz HD, Sachar DB. The extra-intestinal complications of Crohn’s disease and ulcerative colitis: a study of 700 patients. Medicine. 1976;55:401–412.
Monsen U, Sorstad J, Hellers G, Johansson C. Extracolonic diagnoses in ulcerative colitis: an epidemiological study. Am J Gastroenterol. 1990;85:711–716.
Rankin GB, Watts HD, Melnyk CS, Kelley ML Jr. National Cooperative Crohn’s Disease Study: extraintestinal manifestations and perianal complications. Gastroenterology. 1979;77:914–920.
Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001;96:1116–1122. https://doi.org/10.1111/j.1572-0241.2001.03756.x.
Ricart E, Panaccione R, Loftus EV Jr, et al. Autoimmune disorders and extraintestinal manifestations in first-degree familial and sporadic inflammatory bowel disease: a case-control study. Inflamm Bowel Dis. 2004;10:207–214.
Su CG, Judge TA, Lichtenstein GR. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Clin N Am. 2002;31:307–327.
Veloso FT, Carvalho J, Magro F. Immune-related systemic manifestations of inflammatory bowel disease. A prospective study of 792 patients. J Clin Gastroenterol. 1996;23:29–34.
Hernandez-Tejero M, Granja Navacerrada A, Bernal Checa P, et al. Prevalence, risk factors and response to treatment of extra-intestinal manifestations in patients with inflammatory bowel disease. Revista espanola de enfermedades digestivas: organo oficial de la Sociedad Espanola de Patologia Digestiva. 2017;109:627–633. https://doi.org/10.17235/reed.2017.4845/2017.
Zippi M, Corrado C, Pica R, et al. Extraintestinal manifestations in a large series of Italian inflammatory bowel disease patients. World J Gastroenterol. 2014;20:17463–17467. https://doi.org/10.3748/wjg.v20.i46.17463.
Vavricka SR, Brun L, Ballabeni P, et al. Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol. 2011;106:110–119. https://doi.org/10.1038/ajg.2010.343.
Lakatos L, Pandur T, David G, et al. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J Gastroenterol. 2003;9:2300–2307.
Isene R, Bernklev T, Hoie O, et al. Extraintestinal manifestations in Crohn’s disease and ulcerative colitis: results from a prospective, population-based European inception cohort. Scand J Gastroenterol. 2015;50:300–305. https://doi.org/10.3109/00365521.2014.991752.
Malaty HM, Lo GH, Hou JK. Characterization and prevalence of spondyloarthritis and peripheral arthritis among patients with inflammatory bowel disease. Clin Exp Gastroenterol. 2017;10:259–263. https://doi.org/10.2147/CEG.S136383.
Fatemi A, Jazi HH, Emami MH, Kazemizadeh A, Tavakkoli H, Smiley A. Relationship between articular and nonarticular manifestations in inflammatory bowel diseases. J Res Med Sci Off J Isfahan Univ Med Sci. 2016;21:48. https://doi.org/10.4103/1735-1995.183989.
Rodriguez VE, Costas PJ, Vazquez M, et al. Prevalence of spondyloarthropathy in Puerto Rican patients with inflammatory bowel disease. Ethnic Dis. 2008;18:S2-225-9.
Orchard TR, Wordsworth BP, Jewell DP. Peripheral arthropathies in inflammatory bowel disease: their articular distribution and natural history. Gut. 1998;42:387–391.
Palm O, Moum B, Jahnsen J, Gran JT. The prevalence and incidence of peripheral arthritis in patients with inflammatory bowel disease, a prospective population-based study (the IBSEN study). Rheumatology. 2001;40:1256–1261.
Yuksel I, Ataseven H, Basar O, et al. Peripheral arthritis in the course of inflammatory bowel diseases. Dig Dis Sci. 2011;56:183–187. https://doi.org/10.1007/s10620-010-1260-z.
Suh CH, Lee CH, Lee J, et al. Arthritic manifestations of inflammatory bowel disease. J Korean Med Sci. 1998;13:39–43. https://doi.org/10.3346/jkms.1998.13.1.39.
Protzer U, Duchmann R, Hohler T, et al. Enteropathic spondylarthritis in chronic inflammatory bowel diseases: prevalence, manifestation pattern and HLA association. Med Klin. 1996;91:330–335.
Ditisheim S, Fournier N, Juillerat P, et al. Inflammatory articular disease in patients with inflammatory bowel disease: result of the Swiss IBD Cohort Study. Inflamm Bowel Dis. 2015;21:2598–2604. https://doi.org/10.1097/MIB.0000000000000548.
Karreman MC, Luime JJ, Hazes JMW, Weel A. The prevalence and incidence of axial and peripheral spondyloarthritis in inflammatory bowel disease: a systematic review and meta-analysis. J Crohn’s Colitis. 2017;11:631–642. https://doi.org/10.1093/ecco-jcc/jjw199.
Ossum AM, Palm O, Lunder AK, et al. Ankylosing spondylitis and axial spondyloarthritis in patients with long-term inflammatory bowel disease: results from 20 years of follow-up in the IBSEN study. J Crohn’s Colitis. 2018;12:96–104. https://doi.org/10.1093/ecco-jcc/jjx126.
Rodriguez-Reyna TS, Martinez-Reyes C, Yamamoto-Furusho JK. Rheumatic manifestations of inflammatory bowel disease. World J Gastroenterol. 2009;15:5517–5524.
Keyal U, Liu Y, Bhatta AK. Dermatologic manifestations of inflammatory bowel disease: a review. Discov Med. 2018;25:225–233.
Hagen JW, Swoger JM, Grandinetti LM. Cutaneous manifestations of Crohn disease. Dermatol Clin. 2015;33:417–431. https://doi.org/10.1016/j.det.2015.03.007.
Roth N, Biedermann L, Fournier N, et al. Occurrence of skin manifestations in patients of the Swiss Inflammatory Bowel Disease Cohort Study. PloS ONE. 2019;14:e0210436. https://doi.org/10.1371/journal.pone.0210436.
Lebwohl M, Lebwohl O. Cutaneous manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 1998;4:142–148.
Troncoso LL, Biancardi AL, de Moraes HV Jr, Zaltman C. Ophthalmic manifestations in patients with inflammatory bowel disease: a review. World J Gastroenterol. 2017;23:5836–5848. https://doi.org/10.3748/wjg.v23.i32.5836.
Santeford A, Wiley LA, Park S, et al. Impaired autophagy in macrophages promotes inflammatory eye disease. Autophagy. 2016;12:1876–1885. https://doi.org/10.1080/15548627.2016.1207857.
Costa Duarte C, Abreu ML, Lemos S, Nascimento E, Parreiras MA, Sales da Cunha A. A cross-sectional study of 130 Brazilian patients with Crohn’s disease and ulcerative colitis: analysis of articular and ophthalmologic manifestations. Clin Rheumatol. 2008;27(4):503–509. https://doi.org/10.1007/s10067-007-0797-5. Epub 2007 Dec 21.
Paroli MP, Spinucci G, Bruscolini A, La Cava M, Abicca I. Uveitis preceding Crohn’s disease by 8 years. Int Ophthalmol. 2011;31:413–415. https://doi.org/10.1007/s10792-011-9470-8.
Evans PE, Pardi DS. Extraintestinal manifestations of inflammatory bowel disease: focus on the musculoskeletal, dermatologic, and ocular manifestations. MedGenMed Medscape Gen Med. 2007;9:55.
Rojas-Feria M, Castro M, Suarez E, Ampuero J, Romero-Gomez M. Hepatobiliary manifestations in inflammatory bowel disease: the gut, the drugs and the liver. World J Gastroenterol. 2013;19:7327–7340. https://doi.org/10.3748/wjg.v19.i42.7327.
Molodecky NA, Kareemi H, Parab R, et al. Incidence of primary sclerosing cholangitis: a systematic review and meta-analysis. Hepatology. 2011;53:1590–1599. https://doi.org/10.1002/hep.24247.
Hirschfield GM, Karlsen TH, Lindor KD, Adams DH. Primary sclerosing cholangitis. Lancet. 2013;382:1587–1599. https://doi.org/10.1016/S0140-6736(13)60096-3.
Guerra I, Bujanda L, Castro J, et al. Clinical characteristics, associated malignancies and management of primary sclerosing cholangitis in inflammatory bowel disease patients: a multicentre retrospective cohort study. J Crohn’s Colitis. 2019;13:1492–1500. https://doi.org/10.1093/ecco-jcc/jjz094.
Acknowledgments
We thank Montero Traducciones, S.L. (Brunete, Spain), for his invaluable help in improving the English. Alicia Algaba has served as a speaker and has received research grant or advisory fees from MSD, Lilly, Roche, Takeda, and Janssen. Iván Guerra has served as speaker or consultant for Takeda, Kern Pharma, Abbvie, and Janssen. Elena Ricart has served as speaker, has received research funding, or has participated in educational and advisory events for MSD, AbbVie, Takeda, Pfizer, Janssen, Frezenius Kabi, Chiesi, and Ferring. Eva Iglesias has served as speaker, a consultant, an advisory member for, or has received research funding from MSD, Abbvie, Kern Pharma, Takeda, and Janssen. Miriam Mañosa has served as a speaker or has received research or education funding from MSD, Abbvie, Hospira, Pfizer, Takeda, Janssen, Ferring, Shire Pharmaceuticals, Dr. Falk Pharma, and Tillotts Pharma. Javier Gisbert has served as a speaker, a consultant, and advisory member for or has received research funding from MSD, Abbvie, Hospira, Pfizer, Kern Pharma, Biogen, Takeda, Janssen, Roche, Sandoz, Celgene, Ferring, Faes Farma, Shire Pharmaceuticals, Dr. Falk Pharma, Tillotts Pharma, Chiesi, Casen Fleet, Gebro Pharma, Otsuka Pharmaceutical, and Vifor Pharma. Jordi Guardiola has served as a speaker, a consultant, an advisory member for, or has received research funding from MSD, Abbvie, Kern Pharma, Takeda, Janssen, Pfizer, Ferring, and GE Healthcare. Ruth de Francisco has served as a speaker or has received research or education funding from MSD, Abbvie, Takeda, Janssen, Faes, Tillots, and Ferring. Pilar Nos has served as speaker, has received research funding, or has participated in educational events for MSD, AbbVie, Takeda, Pfizer, Janssen, Faes, Otsuka, Chiesi, and Ferring. Jesús Barrio has served as a speaker or has received research funding or advisory fees from MSD, AbbVie, Takeda, Janssen, and Ferring. María Dolores Martín-Arranz has received fees as a speaker, consultant, and advisory member for or has received research funding from MSD, AbbVie, Hospira, Pfizer, Takeda, Janssen, Shire Pharmaceuticals, Tillotts Pharma, and Faes Pharma. Xavier Calvet has received grants for research from Abott, MSD, and Vifor or fees for advisory boards from Abott, MSD, Takeda, Pfizer, Janssen, and Vifor and has given lectures for Abott, MSD, Janssen, Pfizer, Takeda, Shire, and Allergan. Santiago García-López has served as speaker, has received research funding, or has participated in educational and advisory events for MSD, AbbVie, Takeda, Pfizer, Janssen, Chiesi, and Ferring. María Esteve reports personal fees from Janssen, Pfizer, Menarini, Tillots Pharma, Takeda, and grants from MSD and Abbvie, outside the submitted work. José L Pérez-Calle has served as speaker, has received research funding from MSD, AbbVie, Janssen, Pfizer, and Takeda, Dr. Falk, and Ferring. Mariana García-Sepulcre has served as speaker, has received research funding, or has participated in educational events for MSD, AbbVie, Takeda, and Janssen. Rufo Lorente has served as speaker, has received research funding, or has participated in educational events for MSD, AbbVie, Takeda, Pfizer, Janssen, Dr Falk, and Ferring. Isabel Blázquez Gómez has served as a speaker or has received research or educational funding from AbbVie and Kern Pharma. Pedro Almela has served as a speaker, a consultant, and advisory member for or has received research funding from MSD, Abbvie, Takeda, Janssen, Gebro Pharma, and Tillotts Pharma. Eugeni Domènech has served as a speaker or has received research or education funding or advisory fees from MSD, AbbVie, Takeda, Kern Pharma, Pfizer, Janssen, Celgene, Adacyte Therapeutics, Otsuka Pharmaceuticals, Ferring, Shire Pharmaceuticals, Tillots, Thermofisher, Grifols, and Gebro. Fernando Bermejo has served as a speaker, a consultant, and advisory member for or has received research funding from MSD, Abbvie, Pfizer, Takeda Janssen, and Gebro.
Funding
The Eneida Registry is funded by AbbVie, Takeda, Pfizer, AMGEN, Kern Pharmaceuticals, and Merck Sharp and Dohme.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the ENEIDA Committee and by the Ethics Committee of the Hospital Universitario de Fuenlabrada. The ENEIDA project was approved by the ethics committees of each participating hospital. Informed consent was obtained in writing from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Algaba, A., Guerra, I., Ricart, E. et al. Extraintestinal Manifestations in Patients with Inflammatory Bowel Disease: Study Based on the ENEIDA Registry. Dig Dis Sci 66, 2014–2023 (2021). https://doi.org/10.1007/s10620-020-06424-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06424-x