Abstract
Background and Aims
Leaving against medical advice (LAMA) is an unfortunate occurrence in 1–2% of all hospitalized patients and is associated with worse outcomes. While this has been investigated across multiple clinical conditions, studies on patients with chronic pancreatitis (CP) are lacking. We aimed to determine the prevalence and determinants of this event among patients with CP.
Methods
The Healthcare Cost and Utilization Project-Nationwide Inpatient Sample (NIS), 2007–2014, was used in the study. Patients with LAMA were identified, and the temporal trend of LAMA was estimated and compared among patients with and without CP. We then extracted patients with a discharge diagnosis of CP from the recent years of HCUP-NIS (2012–2014) and described the characteristics of LAMA in these patients. Multivariate logistic regression models were used to evaluate predictors of LAMA.
Results
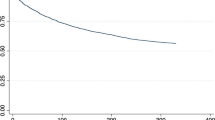
3.39% of patients with CP discharged against medical advice. LAMA rate in CP patients was higher and increased more steeply at quadruple the rate of those without. More likely to self-discharge were patients who were young, males, non-privately insured, or engaged in alcohol and substance abuse, likewise were those with psychosis and those admitted on a weekend or non-electively. The northeast and for-profit hospitals also had higher odds of LAMA. However, patients transferred from other healthcare facilities have reduced LAMA odds. Among all patients with CP, those with LAMA had shorter length of stay (2.74 [2.62–2.85] days vs. 5.78 [5.71–5.83] days) and lower hospitalization cost $23,271 [$22,171–$24,370] versus $45,472 [$44,381–$46,562] compared to the no-LAMA group.
Conclusion
LAMA occurs in approximately 1 in 29 patients with CP and is increasing at almost quadruple the rate of those without. Clinicians need to pay closer attention to the identified at-risk groups for ameliorative targeted interventions.

Similar content being viewed by others
Abbreviations
- LAMA:
-
Leaving against medical advice
- CP:
-
Chronic pancreatitis
- LOS:
-
Length of stay
- THC:
-
Total hospital cost
References
Al-Ghafri M, Al-Bulushi A, Al-Qasmi A. Prevalence of and reasons for patients leaving against medical advice from paediatric wards in Oman. Sultan Qaboos Univ Med J. 2016;16:e74–e77.
Kraut A, Fransoo R, Olafson K, Ramsey CD, Yogendran M, Garland A. A population-based analysis of leaving the hospital against medical advice: incidence and associated variables. BMC Health Serv Res. 2013;13:415.
Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health. 2007;97:2204–2208.
Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ. Leaving Against Medical Advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25:926–929.
Ti L, Ti L. Leaving the hospital against medical advice among people who use illicit drugs: a systematic review. Am J Public Health. 2015;105:e53–59.
Seaborn Moyse H, Osmun WE. Discharges against medical advice: a community hospital’s experience. Can. J. Rural Med. 2004;9:148–153.
Brook M, Hilty DM, Liu W, Hu R, Frye MA. Discharge against medical advice from inpatient psychiatric treatment: a literature review. Psychiatr Serv Wash DC. 2006;57:1192–1198.
Garland A, Ramsey CD, Fransoo R, et al. Rates of readmission and death associated with leaving hospital against medical advice: a population-based study. CMAJ Can Med Assoc J J Assoc Medicale Can. 2013;185:1207–1214.
Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med. 2012;125:594–602.
Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med. 1998;13:568–571.
Anis AH, Sun H, Guh DP, Palepu A, Schechter MT, O’Shaughnessy MV. Leaving hospital against medical advice among HIV-positive patients. CMAJ Can Med Assoc J J Assoc Medicale Can. 2002;167:633–637.
Myers RP, Shaheen AAM, Hubbard JN, Kaplan GG. Characteristics of patients with cirrhosis who are discharged from the hospital against medical advice. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2009;7:786–792.
Baptist AP, Warrier I, Arora R, Ager J, Massanari RM. Hospitalized patients with asthma who leave against medical advice: characteristics, reasons, and outcomes. J Allergy Clin Immunol. 2007;119:924–929.
Saitz R, Ghali WA, Moskowitz MA. Characteristics of patients with pneumonia who are discharged from hospitals against medical advice. Am J Med. 1999;107:507–509.
Fiscella K, Meldrum S, Barnett S. Hospital discharge against advice after myocardial infarction: deaths and readmissions. Am J Med. 2007;120:1047–1053.
Kaplan GG, Panaccione R, Hubbard JN, et al. Inflammatory bowel disease patients who leave hospital against medical advice: predictors and temporal trends. Inflamm Bowel Dis. 2009;15:845–851.
Hayat AA, Ahmed MM, Minhas FA. Patients leaving against medical advice: an inpatient psychiatric hospital-based study. J Coll Phys Surg Pak JCPSP. 2013;23:342–346.
Conwell DL, Lee LS, Yadav D, et al. American Pancreatic Association practice guidelines in chronic pancreatitis: evidence-based report on diagnostic guidelines. Pancreas. 2014;43:1143–1162.
Shuja A, Rahman A, Skef W, Smotherman C, Guan J, Malespin M, de Melo SW Jr. A longitudinal analysis of the epidemiology and economic impact of inpatient admissions for chronic pancreatitis in the United States. Ann Gastroenterol. 2018;31:499–505.
Shah R, Haydek C, Mulki R, Qayed E. Incidence and predictors of 30-day readmissions in patients hospitalized with chronic pancreatitis: A nationwide analysis. Pancreatol Off J Int Assoc Pancreatol IAP Al. 2018;18:386–393.
Enweluzo C, Tlhabano L. Pain management in chronic pancreatitis: taming the beast. Clin Exp Gastroenterol. 2013;6:167–171.
HCUP-US NIS Overview. https://www.hcup-us.ahrq.gov/nisoverview.jsp#data (accessed data on 13 December 2017).
Rothstein MA. Is deidentification sufficient to protect health privacy in research? Am J Bioeth AJOB. 2010;10:3–11.
CFR 46. HHS.gov https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html (2016) (accessed data on 30 July 2018).
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139.
Akanbi O, Adejumo A, Saleem N, Francisque F. Sickle cell disease is associated with higher mortality among patients hospitalized with ischemic bowel disease. Eur J Gastroenterol Hepatol. 2018;30:1027–1032.
Adejumo AC, Akanbi O, Pani L. Among inpatients, ischemic bowel disease predisposes to Clostridium difficile infection with concomitant higher mortality and worse outcomes. Eur. J. Gastroenterol. Hepatol.. 2019;31:109–115.
Adejumo AC, Adejumo KL, Adegbala OM, Chinedozi I, Ndansi J, Akanbi O et al. Protein-energy malnutrition and outcomes of hospitalizations for heart failure in the USA. Am J Cardiol. 2019;123:929–935.
Consumer Price Index Data from 1913 to 2019. US Inflation Calculator https://www.usinflationcalculator.com/inflation/consumer-price-index-and-annual-percent-changes-from-1913-to-2008/ (2008) (accessed data on 23 March 2019).
HCUP Methods Series Calculating National Inpatient Sample (NIS) Variances for Data Years 2012 and Later. https://www.hcup-us.ahrq.gov/reports/methods/2015_09.jsp#appa (accessed data on 23 March 2019).
Hale JJ, Thompson DM, Darden PM. Calculating subset weighted analysis using proc surveyfreq and genmod. https://support.sas.com/resources/papers/proceedings13/272-2013.pdf (accessed data on 23 December 2017).
Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. Discharge against medical advice in the United States, 2002–2011. Mayo Clin Proc. 2017;92:525–535.
Yuan S, Ashmore S, Chaudhary KR, Hsu B, Puumala SE. The role of socioeconomic status in individuals that leave against medical advice. S D Med J S D State Med Assoc. 2018;71:214–219.
Muthusamy AK, Cappell MS, Manickam P, Levine DL. Risk factors for discharge against medical advice in patients with UGI bleeding or abdominal pain: a study of 170 discharges against medical advice among 11,996 emergency department visits. Minerva Gastroenterol Dietol. 2015;61:185–190.
Yong TY, Fok JS, Hakendorf P, Ben-Tovim D, Thompson CH, Li JY. Characteristics and outcomes of discharges against medical advice among hospitalised patients. Intern Med J. 2013;43:798–802.
Menendez ME, van Dijk CN, Ring D. Who leaves the hospital against medical advice in the orthopaedic setting? Clin Orthop. 2015;473:1140–1149.
Schaefer GR, et al. Financial responsibility of hospitalized patients who left against medical advice: medical urban legend? J Gen Intern Med. 2012;27:825–830.
Wigder HN, Propp DA, Leslie K, Mathew A. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010;55:393.
Ling S, Cleverley K, Brennenstuhl S, Bindseil K. Predictors of leaving an inpatient medical withdrawal service against medical advice: a retrospective analysis. J Addict Med. 2018;. https://doi.org/10.1097/ADM.0000000000000431.
Kwok CS, Bell M, Anderson HV, Al Shaibi K, Gulati R, Potts J. Discharge against medical advice after percutaneous coronary intervention in the United States. JACC Cardiovasc Interv. 2018;11:1354–1364.
Jeong J, Song KJ, Kim YJ, et al. The association between acute alcohol consumption and discharge against medical advice of injured patients in the ED. Am J Emerg Med. 2016;34:464–468.
Gonzalez M, Clarke DE, Pereira A, et al. The impact of knowledge on attitudes of emergency department staff towards patients with substance related presentations: a quantitative systematic review protocol. JBI Database Syst Rev Implement Rep. 2015;13:133–145.
Tawk R, Dutton M. Racial differences in length of stay for patients who leave against medical advice from U.S. general hospitals. Int J Environ Res Public Health. 2016;13:95.
Olufajo OA, Metcalfe D, Yorkgitis BK, et al. Whatever happens to trauma patients who leave against medical advice? Am J Surg. 2016;211:677–683.
Marcoux J, Alkutbi M, Lamoureux J, Feyz M, Saluja RS, de Guise E. Discharge against medical advice in traumatic brain injury: follow-up and readmission rate. Can J Neurol Sci. 2017;44:311–317.
Onukwugha E, Saunders E, Mullins CD, Pradel FG, Zuckerman M, Weir MR. Reasons for discharges against medical advice: a qualitative study. Qual Saf Health Care. 2010;19:420–424.
Noohi K, Komsari S, Nakhaee N, Yazdi Feyzabadi V. Reasons for discharge against medical advice: a case study of emergency departments in Iran. Int J Health Policy Manag. 2013;1:137–142.
Xiao AY, Tan ML, Plana MN, Yadav D, Zamora J, Petrov MS. The use of international classification of diseases codes to identify patients with pancreatitis: a systematic review and meta-analysis of diagnostic accuracy studies. Clin Transl Gastroenterol. 2018;9:191.
Moores K, Gilchrist B, Carnahan R, Abrams T. A systematic review of validated methods for identifying pancreatitis using administrative data. Pharmacoepidemiol. Drug Saf.. 2012;21(Suppl 1):194–202.
Yadav D, Dhir R. How Accurate are ICD-9 Codes for Acute (Ap) and Chronic (Cp) Pancreatitis?-A Large VA Hospital Experience. Pancreas. 2006;33:508.
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Contributions
OA and ACA contributed equally to the study concept, design, acquisition, analysis, interpretation of data, and drafting of the manuscript. MS and PK edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no conflicts.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Akanbi, O., Adejumo, A.C., Soliman, M. et al. Chronic Pancreatitis Patients Who Leave Against Medical Advice: Prevalence, Trend, and Predictors. Dig Dis Sci 66, 424–433 (2021). https://doi.org/10.1007/s10620-020-06279-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06279-2