Abstract
Background
Many patients are not candidates for liver transplant for non-tumor-related reasons including medical comorbidities and non-adherence. The prognosis of patients with hepatocellular carcinoma (HCC) who are not liver transplant candidates in the era of locoregional therapy (LRT) including y90 is not well defined.
Aims
This study seeks to evaluate outcomes and the natural history of early-stage HCC in patients who were denied liver transplant listing due to non-tumor reasons and instead were treated with LRT.
Methods
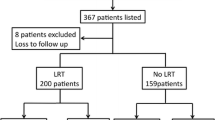
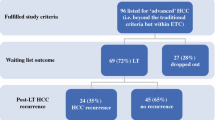
A retrospective evaluation was performed for all patients who completed liver transplant evaluation with their tumor within Milan criteria but were denied due to non-tumor reasons and were treated with LRT at a single tertiary referral center.
Results
The 61 patients included had a favorable overall survival, with a median survival 60.3 months (86.9% at 1 year and 52.7% at 5 years). Patients with Child–Pugh A cirrhosis (n = 34) had significantly longer overall survival compared to those with Child–Pugh B/C cirrhosis (median survival of 70.3 months versus 26.1 months, p = 0.005). Survival in patients with Child–Pugh A at 1, 3, and 5 years was 97%, 80%, and 73%, respectively, compared to 74%, 41%, and 31% in patients with Child–Pugh B/C.
Conclusions
In a small single-center cohort, patients with HCC who were denied liver transplant due to non-tumor reasons and underwent LRT and had Child–Pugh A cirrhosis had survival approaching the national average for patients who undergo liver transplantation. Patients with Child–Pugh B/C cirrhosis had significantly worse outcomes than those with Child–Pugh A.


Similar content being viewed by others
References
White DL, Thrift AP, Kanwal F, Davila J, El-Serag HB. Incidence of hepatocellular carcinoma in all 50 United States, from 2000 through 2012. Gastroenterology. 2017;152:812-20.e5. https://doi.org/10.1053/j.gastro.2016.11.020.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–700. https://doi.org/10.1056/nejm199603143341104.
Organ Procurement and Transplantation Network (OPTN) Policies. https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf. 2018. https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf#nameddest=Policy_09.
Mazzaferro V, Bhoori S, Sposito C, et al. Milan criteria in liver transplantation for hepatocellular carcinoma: an evidence-based analysis of 15 years of experience. Liver Transplant. 2011;17:S44–S57. https://doi.org/10.1002/lt.22365.
Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2016 annual data report: liver. Am J Transplant. 2018;18:172–253. https://doi.org/10.1111/ajt.14559.
Salem R, Gordon AC, Mouli S, et al. Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2016;. https://doi.org/10.1053/j.gastro.2016.08.029.
Lee Cheah Y, Chow PKH. Liver transplantation for hepatocellular carcinoma: an appraisal of current controversies. Liver Cancer. 2012;1:183–189. https://doi.org/10.1159/000343832.
Kutlu OC, Chan JA, Aloia TA, et al. Comparative effectiveness of first-line radiofrequency ablation versus surgical resection and transplantation for patients with early hepatocellular carcinoma. Cancer. 2017;123:1817–1827. https://doi.org/10.1002/cncr.30531.
Arya A, Hernandez-Alejandro R, Marotta P, Uhanova J, Chandok N. Recipient ineligibility after liver transplantation assessment: a single centre experience. Can J Surg. 2013;56:E39–E43. https://doi.org/10.1503/cjs.004512.
Poonja Z, Brisebois A, van Zanten SV, Tandon P, Meeberg G, Karvellas CJ. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clin Gastroenterol Hepatol. 2014;12:692–698. https://doi.org/10.1016/j.cgh.2013.08.027.
Elwir S, Lake J. Current status of liver allocation in the United States. Gastroenterol Hepatol. 2016;12:166–170.
Rahimi RS, Trotter JF. Liver transplantation for hepatocellular carcinoma: outcomes and treatment options for recurrence. Ann Gastroenterol. 2015;28:323–330.
Duvoux C, Roudot-Thoraval F, Decaens T, et al. Liver transplantation for hepatocellular carcinoma: a model including alpha-fetoprotein improves the performance of Milan criteria. Gastroenterology. 2012;143:986-94.e3. https://doi.org/10.1053/j.gastro.2012.05.052. quiz e14-5.
Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011;140:497–507.e2. https://doi.org/10.1053/j.gastro.2010.10.049.
Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1–85.
Khalaf N, Ying J, Mittal S, et al. Natural history of untreated hepatocellular carcinoma in a US cohort and the role of cancer surveillance. Clin Gastroenterol Hepatol. 2017;15:273–81.e1. https://doi.org/10.1016/j.cgh.2016.07.033.
Pelletier SJ, Fu S, Thyagarajan V, et al. An intention-to-treat analysis of liver transplantation for hepatocellular carcinoma using organ procurement transplant network data. Liver Transplant. 2009;15:859–868. https://doi.org/10.1002/lt.21778.
Murali AR, Patil S, Phillips KT, Voigt MD. Locoregional therapy with curative intent versus primary liver transplant for hepatocellular carcinoma: systematic review and meta-analysis. Transplantation. 2017;101:e249–e257. https://doi.org/10.1097/tp.0000000000001730.
D’Avola D, Lnarrairaegui M, Bilbao JI, et al. A retrospective comparative analysis of the effect of Y90-radioembolization on the survival of patients with unresectable hepatocellular carcinoma. Hepato-Gastroenterology. 2009;56:1683–1688.
Tan D, Yopp A, Beg MS, Gopal P, Singal AG. Meta-analysis: underutilisation and disparities of treatment among patients with hepatocellular carcinoma in the United States. Aliment Pharmacol Ther. 2013;38:703–712. https://doi.org/10.1111/apt.12450.
Zaydfudim V, Whiteside MA, Griffin MR, Feurer ID, Wright JK, Pinson CW. Health insurance status affects staging and influences treatment strategies in patients with hepatocellular carcinoma. Ann Surg Oncol. 2010;17:3104–3111. https://doi.org/10.1245/s10434-010-1181-2.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FV, DH, JF, MM, MI, LJ, AZ, and RC were involved in study conception and design. FV, DH, JF, MM, MI, and LJ contributed to acquisition of data. FV performed the statistical analysis. FV and DH drafted the manuscript. AZ and RC provided critical revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zori, A., Villanueva, F., Hatamleh, D. et al. Favorable Survival with Non-curative Treatments for Patients with Early-Stage Hepatocellular Carcinoma After Liver Transplant Denial. Dig Dis Sci 66, 628–635 (2021). https://doi.org/10.1007/s10620-020-06201-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06201-w