Abstract
Background
Surveillance colonoscopy guidelines following adenomas or sessile serrated adenomas/polyps (SSPs) are based on pathology features known to be associated with risk of future colorectal cancer. A synchronous conventional adenoma may increase the malignant potential of SSP, but current guidelines do not address this combination of pathologies.
Aims
The aim was to assess the risk of advanced neoplasia after SSP with or without synchronous adenoma compared to that following a conventional adenoma.
Methods
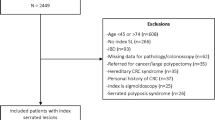
An audit was conducted on colonoscopies performed between 2000 and 2014 as part of a surveillance program. Index colonoscopy findings were classified as: low-risk SSP and high-risk SSP (size ≥ 10 mm or with cytological dysplasia) with and without synchronous adenoma; high-risk adenoma and low-risk adenoma. Risk of advanced neoplasia was determined at subsequent surveillance colonoscopies.
Results
In total, 2157 patients had adenoma or SSP found at index colonoscopy—low-risk adenoma (40%), high-risk adenoma (54%) and SSP (4%). Synchronous adenomas were seen with 47% of SSP. The median follow-up was 50.3 months (interquartile range 28.1–79.3). Compared to an index finding of low-risk adenoma, index findings of high-risk adenoma, as well as SSP with synchronous adenoma, were independent predictors of future advanced neoplasia (high-risk adenoma: hazard ratio (HR) = 2.04 (95% CI 1.70–2.45); high-risk SSP + adenoma HR = 3.20 (95% CI 1.31–7.82); low-risk SSP + adenoma: HR = 2.20 (95% CI 1.03–4.68)).
Conclusions
Synchronous adenoma increases the risk of advanced neoplasia for SSP equivalent to that seen following high-risk adenoma. Guidelines for surveillance should take into account concurrent pathologies with SSP.
Similar content being viewed by others
References
Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088–2100.
Jass JR. Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology. 2007;50:113–130.
Bosman F, World Health Organization. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: International Agency for Research on Cancer; 2010.
Singh R, Zorron Cheng Tao PuL, Koay D, Burt A. Sessile serrated adenoma/polyps: Where are we at in 2016? World J Gastroenterol. 2016;22:7754–7759.
Hassan C, Quintero E, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy. 2013;45:842–851.
Erichsen R, Baron JA, Hamilton-Dutoit SJ, et al. Increased risk of colorectal cancer development among patients with serrated polyps. Gastroenterology. 2016;150:895–902e5.
Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US multi-society task force on colorectal cancer. Gastroenterology. 2012;143:844–857.
Pai RK, Hart J, Noffsinger AE. Sessile serrated adenomas strongly predispose to synchronous serrated polyps in non-syndromic patients. Histopathology. 2010;56:581–588.
Vu HT, Lopez R, Bennett A, Burke CA. Individuals with sessile serrated polyps express an aggressive colorectal phenotype. Dis Colon Rectum. 2011;54:1216–1223.
Schreiner MA, Weiss DG, Lieberman DA. Proximal and large hyperplastic and nondysplastic serrated polyps detected by colonoscopy are associated with neoplasia. Gastroenterology. 2010;139:1497–1502.
Pereyra L, Zamora R, Gomez EJ, et al. Risk of metachronous advanced neoplastic lesions in patients with sporadic sessile serrated adenomas undergoing colonoscopic surveillance. Am J Gastroenterol. 2016;111:871–878.
Bampton PA, Sandford JJ, Young GP. Applying evidence-based guidelines improves use of colonoscopy resources in patients with a moderate risk of colorectal neoplasia. Med J Aust. 2002;176:155–157.
Symonds EL, Simpson K, Coats M, et al. A nurse-led model maintains high adherence with recall guidelines within a colorectal cancer surveillance program at public academic hospitals. Med J Aust. 2018 (in press).
Cancer Council Australia Colonoscopy Surveillance Working Party, Clinical practice guidelines for surveillance colonoscopy—in adenoma follow-up; following curative resection of colorectal cancer; and for cancer surveillance in inflammatory bowel disease. Vol. Sydney. 2011.
Melson J, Ma K, Arshad S, et al. Presence of small sessile serrated polyps increases rate of advanced neoplasia upon surveillance compared with isolated low-risk tubular adenomas. Gastrointest Endosc. 2016;84:307–314.
Anderson JC, Butterly LF, Robinson CM, et al. Risk of metachronous high-risk adenomas and large serrated polyps in individuals with serrated polyps on index colonoscopy: data from the new hampshire colonoscopy registry. Gastroenterology. 2018;154:117–127e2.
Pai RK, Mackinnon AC, Joseph L, Noffsinger A, Hart J. Identification of histologically distinct conventional adenomas that arise predominately in patients with sessile serrated adenomas. Am J Surg Pathol. 2010;34:355–363.
Macaron C, Vu HT, Lopez R, Pai RK, Burke CA. Risk of metachronous polyps in individuals with serrated polyps. Dis Colon Rectum. 2015;58:762–768.
Hassan C, Giorgi Rossi P, Camilloni L, et al. Meta-analysis: adherence to colorectal cancer screening and the detection rate for advanced neoplasia, according to the type of screening test. Aliment Pharmacol Ther. 2012;36:929–940.
Kahi CJ. How does the serrated polyp pathway alter CRC screening and surveillance? Dig Dis Sci. 2015;60:773–780.
Acknowledgments
Author RM was supported by a grant funded by the financial support of Cancer Council SA’s Beat Cancer Project on behalf of its donors and the State Government of South Australia through the Department of Health together with the support of the Flinders Medical Centre Foundation, its donors and partners. The authors would like to acknowledge the assistance of Tony Thomas (TT) for reviewing some of the pathologies.
Funding
Author RM was supported by a grant funded by the financial support of Cancer Council SA’s Beat Cancer Project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Symonds, E., Anwar, S., Young, G. et al. Sessile Serrated Polyps with Synchronous Conventional Adenomas Increase Risk of Future Advanced Neoplasia. Dig Dis Sci 64, 1680–1685 (2019). https://doi.org/10.1007/s10620-019-5454-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-5454-8