Abstract
Background
Secondary infection is an important factor affecting mortality and quality of life in patients with severe acute pancreatitis. The characteristics of secondary infection, which are well known to clinicians, need to be re-examined in detail, and their understanding among clinicians needs to be updated accordingly.
Aim
This study aims to investigate the characteristics and drug resistance of pathogens causing severe acute pancreatitis (SAP) secondary infection, to objectively present infection situation, and to provide reference for improved clinical management.
Methods
A retrospective analysis was performed on 55 consecutive patients with SAP who developed secondary infection with an accurate evidence of bacterial/fungal culture from 2016 to 2018. The statistics included the spectrum and distribution of pathogens, the drug resistance of main pathogens, and associations between multiple infectious parameters and mortality.
Results
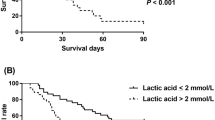
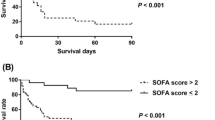
A total of 181 strains of pathogens were isolated from (peri)pancreas; bloodstream; and respiratory, urinary, and biliary systems in 55 patients. The strains included 98 g-negative bacteria, 58 g-positive bacteria, and 25 fungi. Bloodstream infection (36.5%) was the most frequent infectious complication, followed by (peri)pancreatic infection (32.0%). Acinetobacter baumannii, Pseudomonas aeruginosa, Klebsiella pneumoniae, Escherichia coli, and Stenotrophomonas maltophilia were predominant among gram-negative bacteria. Gram-positive bacterial infections were mainly caused by Enterococcus faecium and Staphylococcus spp. Fungal infections were predominantly caused by Candida spp. The drug resistance of pathogens causing SAP secondary infection was generally higher than the surveillance level. Patients in the death group were older (55 ± 13 years vs. 46 ± 14 years; p = 0.039) and had longer intensive care unit (ICU) stay (14 vs. 8; p = 0.026) than those in the survival group. A. baumannii infection (68.4% vs. 33%; p = 0.013), number of pathogens ≥ 4 (10 vs. 6; p = 0.005), pancreatic infection (14 vs. 15, p = 0.024), and urinary infection (8 vs. 5; p = 0.019) were significantly associated with mortality.
Conclusion
Gram-negative bacteria are the main pathogens causing SAP secondary infection, in which nosocomial infections play a major role. The drug resistance profile of gram-negative bacteria is seriously threatening, and the commonly used antibiotics in SAP are gradually losing their effectiveness. Much attention should be paid to the rational use of antibiotics, and strategies should be established for infection prevention in SAP.


Similar content being viewed by others
References
Choi JH, Kim MH, Oh D, et al. Clinical relevance of the revised Atlanta classification focusing on severity stratification system. Pancreatology. 2014;14:324–329.
Fernandes SR, Carvalho J, Santos P, et al. Atlanta, revised Atlanta, and determinant-based classification–application in a cohort of Portuguese patients with acute pancreatitis. Eur J Gastroenterol Hepatol. 2016;28:20–24.
Brown LA, Hore TA, Phillips AR, et al. A systematic review of the extra-pancreatic infectious complications in acute pancreatitis. Pancreatology. 2014;14:436–443.
van Brunschot S, Bakker OJ, BesseIink MG, et al. Treatment of necrotizing pancreatitis. Clin Gastroenterol Hepatol. 2012;10:1190–1201.
Werge M, Novovic S, Schmidt PN. Infection increases mortality in necrotizing pancreatitis: A systematic review and meta-analysis. Pancreatology. 2016;16:698–707.
van Santvoort HC, Besselink MG, Bakker OJ, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. NEJM. 2010;362:1491–1502.
Aparna D, Kumar S. Mortality and morbidity in necrotizing pancreatitis managed on principles of step-up approach: 7 years experience from a single surgical unit. World J Gastrointest Surg. 2017;9:200–208.
Wereszczynska-Siemiatkowska U, Swidnicka-Siergiejko A, Siemiatkowski A. Early enteral nutrition is superior to delayed enteral nutrition for the prevention of infected necrosis and mortality in acute pancreatitis. Pancreas. 2013;42:640–646.
Peng YB, Huang J, Qin S, et al. Investigation of distribution of bacteria and fungi in severe acute pancreatitis. Chin J Surg. 2010;48:496–501.
Noor MT, Radhakrishna Y, Kochhar R, et al. Bacteriology of infection in severe acute pancreatitis. JOP. 2011;12:19–25.
Su MS, Lin MH, Zhao QH, et al. Clinical study of distribution and drug resistance of pathogens in patients with severe acute pancreatitis. Chin Med J (Engl). 2012;125:1772–1776.
Ma HX, He L, Cai SW, et al. Analysis of the spectrum and resistance of pathogen causing sepsis in patients with severe acute pancreatitis. Chin J Surg. 2017;55:378–383.
Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
van Baal MC, Bollen TL, Bakker OJ, et al. The role of routine fine-needle aspiration in the diagnosis of infected necrotizing pancreatitis. Surgery. 2014;155:442–448.
Jorgensen JH, Pfaller MA, Carroll KC, et al. Manual of Clinical Microbiology. 11th ed. Washington, DC: ASM Press; 2015.
Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. M100 27th ed. Wayne, PA; 2017.
Hu FP, Guo Y, et al. CHINET surveillance of bacterial resistance across China: report of the results in 2016. Chin J Infect Chemother. 2017;17:481–491.
Petrov MS, Shanbhag S, Chakraborty M, et al. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology. 2010;139:813–820.
Fritz S, Hackert T, Hartwig W, et al. Bacterial translocation and infected pancreatic necrosis in acute necrotizing pancreatitis derives from small bowel rather than from colon. Am J Surg. 2010;200:111–117.
Dellinger EP, Tellado JM, Soto NE, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Ann Surg. 2007;245:674–683.
Besselink MG, van Santvoort HC, Boermeester MA, et al. Timing and impact of infections in acute pancreatitis. Br J Surg. 2009;96:267–273.
Foitzik T, Fernández-del Castillo C, Ferraro MJ, et al. Pathogenesis and prevention of early pancreatic infection in experimental acute necrotizing pancreatitis. Ann Surg. 1995;222:179–185.
Xue P, Deng LH, Zhang ZD, et al. Infectious complications in patients with severe acute pancreatitis. Dig Dis Sci. 2009;54:2748–2753. https://doi.org/10.1007/s10620-008-0668-1.
Liu L, Yan H, Liu W, et al. Abdominal paracentesis drainage does not increase infection in severe acute pancreatitis: a prospective study. J Clin Gastroenterol. 2015;49:757–763.
Zerem E, Imamovic G, Omerović S. Randomized controlled trial on sterile fluid collections management in acute pancreatitis: should they be removed? Surg Endosc. 2009;23:2770–2777.
Trikudanathan G, Navaneethan U. Intra-abdominal fungal infections complicating acute pancreatitis: a review. Am J Gastroenterol. 2011;106:1188–1192.
Moka P, Goswami P, Kapil A, et al. Impact of antibiotic-resistant bacterial and fungal infections in outcome of acute pancreatitis. Pancreas. 2018;47:489–494.
Schepers NJ, Bakker OJ, Besselink MG, et al. Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis. Gut. 2018;68:1044–1051.
Pavlidis P, Crichton S, Lemmich Smith J, et al. Improved outcome of severe acute pancreatitis in the intensive care unit. Crit Care Res Pract. 2013;2013:897107.
Alberti C, Brun-Buisson C, Burchardi H, et al. Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med. 2002;28:108–121.
Feretzakis G, Loupelis E, Sakagianni A, et al. A 2-year single-centre audit on antibiotic resistance of, and strains from an intensive care unit and other wards in a general public hospital in Greece. Antibiotics (Basel). 2019;8:62.
Chiang CH, Pan SC, Yang TS, et al. Healthcare-associated infections in intensive care units in Taiwan, South Korea, and Japan: recent trends based on national surveillance reports. Antimicrob Resist Infect Control. 2018;7:129.
Párniczky A, Lantos T, Tóth EM, et al. Antibiotic therapy in acute pancreatitis: from global overuse to evidence based recommendations. Pancreatology. 2019;19:488–499.
Ibn Saied W, Mourvillier B, Cohen Y, et al. A comparison of the mortality risk associated with ventilator-acquired bacterial pneumonia and nonventilator ICU-acquired bacterial pneumonia. Crit Care Med. 2019;47:345–352.
Párniczky A, Kui B, Szentesi A, et al. Prospective, multicentre, nationwide clinical data from 600 cases of acute pancreatitis. PLoS ONE. 2016;11:e0165309.
Carvalho JR, Fernandes SR, Santos P, et al. Acute pancreatitis in the elderly: a cause for increased concern? Eur J Gastroenterol Hepatol. 2018;30:337–341.
Pando E, Alberti P, Hidalgo J, et al. The role of extrapancreatic infections in the prediction of severity and local complications in acute pancreatitis. Pancreatology. 2018;18:486–493.
Cacopardo B, Pinzone M, Berretta S, et al. Localized and systemic bacterial infections in necrotizing pancreatitis submitted to surgical necrosectomy or percutaneous drainage of necrotic secretions. BMC Surg. 2013;13:S50.
Reuken PA, Albig H, Rödel J, et al. Fungal infections in patients with infected pancreatic necrosis and pseudocysts: risk factors and outcome. Pancreas. 2018;47:92–98.
De Waele JJ, Vogelaers D, Hoste E, et al. Emergence of antibiotic resistance in infected pancreatic necrosis. Arch Surg. 2004;139:1371–1375.
Isenmann R, Rünzi M, Kron M, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology. 2004;126:997–1004.
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–e15.
Yokoe M, Takada T, Mayumi T, et al. Japanese guidelines for the management of acute pancreatitis: Japanese guidelines 2015. J Hepatobiliary Pancreat Sci. 2015;22:405–432.
Ukai T, Shikata S, Inoue M, et al. Early prophylactic antibiotics administration for acute necrotizing pancreatitis: a meta-analysis of randomized controlled trials. J Hepatobiliary Pancreat Sci. 2015;22:316–321.
Acknowledgments
We thank Dr. Ming Ma from Clinical Laboratory Department of the First Affiliated Hospital of China Medical University for his microbiological consultation in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tian, H., Chen, L., Wu, X. et al. Infectious Complications in Severe Acute Pancreatitis: Pathogens, Drug Resistance, and Status of Nosocomial Infection in a University-Affiliated Teaching Hospital. Dig Dis Sci 65, 2079–2088 (2020). https://doi.org/10.1007/s10620-019-05924-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05924-9