Abstract
Background
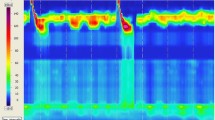
A novel three-dimensional high-resolution esophageal manometry provides a dynamic 360° representation of the pressure at the esophagogastric junction.
Aims
To describe the three-dimensional high-resolution esophageal manometry patterns of achalasia.
Methods
We retrospectively included all consecutive patients who underwent three-dimensional high-resolution esophageal manometry before and after treatment (pneumatic dilatation or per-oral endoscopic myotomy) for achalasia between November 2016 and July 2017. The distribution of the pressures at the esophagogastric junction on three-dimensional high-resolution esophageal manometry was determined.
Results
Eighteen patients were included. Mean integrated relaxation pressure was 20.7 mmHg, and median (range) Eckardt score was 7 (4–10). Nine patients were treated by pneumatic dilatation and seven by myotomy. Nine patients underwent three-dimensional high-resolution esophageal manometry after treatment. Before treatment, the esophagogastric junction pressure distribution was best observed at end expiration and during the 4 s of the integrated relaxation pressure measurement. During the integrated relaxation pressure, the lower esophageal sphincter was asymmetric in 12 patients with a high-pressure zone between the left and the posterior side of the esophagogastric junction. After treatment, five patients had a residual high-pressure point on the left or the posterior side of the esophagogastric junction.
Conclusions
Three-dimensional high-resolution esophageal manometry allows a simple assessment of the pressure topography at the EGJ. In patients with achalasia, we found the esophagogastric junction pressure to be asymmetric with a peak pressure on the greater curvature side. Three-dimensional high-resolution esophageal manometry has the potential to guide initial and redo treatments.




Similar content being viewed by others
Abbreviations
- CD:
-
Crural diaphragm
- CT:
-
Computerized tomography
- EGJ:
-
Esophagogastric junction
- LES:
-
Lower esophageal sphincter
- IRP:
-
Integrated relaxation pressure
- 3D-HRM:
-
Three-dimensional high-resolution manometry
References
Roman S, Huot L, Zerbib F, et al. High-resolution manometry improves the diagnosis of esophageal motility disorders in patients with dysphagia: a randomized multicenter study. Am J Gastroenterol. 2016;111:372–380.
Mittal RK, Balaban DH. The esophagogastric junction. N Engl J Med. 1997;336:924–932.
Mittal RK, Zifan A, Kumar D, Ledgerwood-Lee M, Ruppert E, Ghahremani G. Functional morphology of the lower esophageal sphincter and crural diaphragm determined by three-dimensional high-resolution esophago-gastric junction pressure profile and CT imaging. Am J Physiol Gastrointest Liver Physiol. 2017;313:G212–G219.
Kwiatek MA, Pandolfino JE, Kahrilas PJ. 3D-high resolution manometry of the esophagogastric junction. Neurogastroenterol Motil Off J Eur Gastrointest Motil Soc. 2011;23:461–469.
Nicodème F, Soper NJ, Lin Z, Pandolfino JE, Kahrilas PJ. Calculation of esophagogastric junction vector volume using three-dimensional high-resolution manometry. Dis Esophagus Off J Int Soc Dis Esophagus. 2015;28:684–690.
Swift GL, Smith PM, McKirdy HC, Lowndes RH. Vector volume analysis of the lower esophageal sphincter in achalasia and the effect of balloon dilation. Dis Esophagus Off J Int Soc Dis Esophagus. 2001;14:54–56.
Nicodème F, Pandolfino JE, Lin Z, Xiao Y, Escobar G, Kahrilas PJ. Adding a radial dimension to the assessment of esophagogastric junction relaxation: validation studies of the 3D-eSleeve. Am J Physiol Gastrointest Liver Physiol. 2012;303:G275–G280.
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet Lond Engl. 2014;383:83–93.
Heniford BT, Matthews BD, Kercher KW, et al. Laparoscopic anterior esophageal myotomy and toupet fundoplication for achalasia. Am Surg. 2001;67:1059–1065.
Mattioli S, Pilotti V, Felice V, Di Simone MP, D’Ovidio F, Gozzetti G. Intraoperative study on the relationship between the lower esophageal sphincter pressure and the muscular components of the gastro-esophageal junction in achalasic patients. Ann Surg. 1993;218:635–639.
Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg Chic Ill. 1960;2003:490–495.
Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271.
Khashab MA, Sharaiha RZ, Saxena P, et al. Novel technique of auto-tunneling during peroral endoscopic myotomy (with video). Gastrointest Endosc. 2013;77:119–122.
Rieder E, Swanström LL, Perretta S, Lenglinger J, Riegler M, Dunst CM. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27:400–405.
Teitelbaum EN, Boris L, Arafat FO, et al. Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc. 2013;27:4547–4555.
Onimaru M, Inoue H, Ikeda H, et al. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217:598–605.
Ramchandani M, Nabi Z, Reddy DN, et al. Outcomes of anterior myotomy versus posterior myotomy during POEM: a randomized pilot study. Endosc Int Open. 2018;6:E190–E198.
Tan Y, Lv L, Wang X, et al. Efficacy of anterior versus posterior per-oral endoscopic myotomy for treating achalasia: a randomized, prospective study. Gastrointest Endosc. 2018;88:46–54.
Onimaru M, Inoue H, Ikeda H, et al. Greater curvature myotomy is a safe and effective modified technique in per-oral endoscopic myotomy (with videos). Gastrointest Endosc. 2015;81:1370–1377.
Acknowledgments
The authors thank the Medtronic Company for gratuitously providing the 3D high-resolution manometry probe.
Author information
Authors and Affiliations
Contributions
M-AG performed the 3D-HRM, collected the data, and wrote the article. CL performed the 3D-HRM. MB analyzed the data, designed the research study, and wrote the paper. SL, RC, FP, and SC made significant comments and modifications to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guillaumot, MA., Léandri, C., Leblanc, S. et al. Three-Dimensional High-Resolution Esophageal Manometry Study of the Esophagogastric Junction in Patients with Achalasia. Dig Dis Sci 65, 1092–1098 (2020). https://doi.org/10.1007/s10620-019-05824-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05824-y