Abstract
Background
Primary biliary cholangitis (PBC) is progressive and can cause end-stage liver disease necessitating a liver transplant (LT). PBC patients may be disadvantaged on LT waitlist due to MELD-based priority listing or other factors.
Aim
The aim was to assess waitlist duration, waitlist mortality, and post-LT outcomes of PBC patients.
Methods
The Scientific Registry of Transplant Recipients data for 1994–2016 was utilized. Adult patients with PBC without hepatocellular carcinoma (HCC) were selected. Their clinico-demographic parameters and waitlist and post-transplant outcomes were compared to those of patients with hepatitis C (HCV) without HCC.
Results
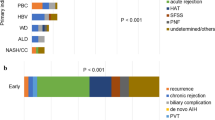
Out of 223,391 listings for LT in 1994–2016, 8133 (3.6%) was for PBC without HCC. Mean age was 55.5 years, 76.9% white, 86.2% female, mean MELD score 21, 6.6% retransplants. There were 52,017 patients with hepatitis C included for comparison. The mean waitlist mortality was 17.9% for PBC and 17.6% for HCV (p > 0.05). The average transplantation rate was 57.7% for PBC and 53.3% for HCV (p < 0.0001), while waitlist dropout (death or removal due to deterioration) rate was 25.0% for PBC and 25.4% for HCV (p > 0.05). There was no significant difference in median waiting duration till transplantation between PBC patients and HCV after 2002 (103 vs. 95 days, p > 0.05). Post-LT mortality and graft loss rates were significantly lower in PBC than in HCV patients (all p < 0.02).
Conclusions
Despite no evidence of impaired waitlist outcomes and favorable post-transplant survival in patients with PBC, there is still a high waitlist dropout rate suggesting the presence of an unmet need for effective treatment.


Similar content being viewed by others
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HRSA:
-
The Health Resources and Services Administration
- LT:
-
Liver transplantation
- MELD:
-
The model for end-stage liver disease
- OCA:
-
Obeticholic acid
- OPTN:
-
Organ procurement and transplantation network
- PBC:
-
Primary biliary cholangitis
- SRTR:
-
Scientific registry of transplant recipients
- UDCA:
-
Ursodeoxycholic acid
References
Kaplan MM, Gershwin ME. Primary biliary cirrhosis. N Engl J Med. 2005;353:1261–1273.
Poupon R. Primary biliary cirrhosis: a 2010 update. J Hepatol. 2010;52:745–758.
Lleo A, Marzorati S, Anaya J-M, Gershwin ME. Primary biliary cholangitis: a comprehensive overview. Hepatol Int. 2017;11:485–499.
Sayiner M, Golabi P, Stepanova M, et al. Primary biliary cholangitis in medicare population: the impact on mortality and resource utilization. Hepatology. 2018. https://doi.org/10.1002/hep.30174.
Selmi C, Bowlus CL, Gershwin ME, Coppel RL. Primary biliary cirrhosis. Lancet. 2011;377:1600–1609.
Boonstra K, Kunst AE, Stadhouders PH, et al. Rising incidence and prevalence of primary biliary cirrhosis: a large population-based study. Liver Int. 2014;34:e31–e38.
Kim WR, Lindor KD, Locke GR 3rd, et al. Epidemiology and natural history of primary biliary cirrhosis in a US community. Gastroenterology. 2000;119:1631–1636.
Locke GR 3rd, Therneau TM, Ludwig J, Dickson ER, Lindor KD. Time course of histological progression in primary biliary cirrhosis. Hepatology. 1996;23:52–56.
Carey EJ, Ali AH, Lindor KD. Primary biliary cirrhosis. Lancet. 2015;386:1565–1575.
Selmi C, Gershwin ME. The etiology mystery in primary biliary cirrhosis. Dig Dis. 2010;28:105–115.
Hirschfield GM, Invernizzi P. Progress in the genetics of primary biliary cirrhosis. Semin Liver Dis. 2011;31:147–156.
Burman BE, Jhaveri MA, Kowdley KV. An update on the treatment and follow-up of patients with primary biliary cholangitis. Clin Liver Dis. 2017;21:709–723.
Lindor KD, Gershwin ME, Poupon R, et al. Primary biliary cirrhosis. Hepatology. 2009;50:291–308.
Akamatsu N, Sugawara Y. Primary biliary cirrhosis and liver transplantation. Intract. Rare Dis. Res. 2012;1:66–80.
Kuiper EMM, Hansen BE, de Vries RA, et al. Improved prognosis of patients with primary biliary cirrhosis that have a biochemical response to ursodeoxycholic acid. Gastroenterology. 2009;136:1281–1287.
Parés A. Treatment of primary biliary cirrhosis: Is there more to offer than ursodeoxycholic acid? Treatment of primary biliary cirrhosis and UDCA. Clin. Liver Dis.. 2014;3:29–33.
Nevens F, Andreone P, Mazzella G, et al. A placebo-controlled trial of obeticholic acid in primary biliary cholangitis. N Engl J Med. 2016;375:631–643.
Khungar V, Goldberg DS. Liver transplantation for cholestatic liver diseases in adults. Clin Liver Dis. 2016;20:191–203.
Golabi P, Bush H, Stepanova M, et al. Liver transplantation (LT) for cryptogenic cirrhosis (CC) and nonalcoholic steatohepatitis (NASH) cirrhosis: data from the scientific registry of transplant recipients (SRTR): 1994 to 2016. Medicine. 2018;97:e11518.
Perumpail RB, Wong RJ, Liu A, et al. Trends in liver transplantation in hepatitis C virus-infected persons, United States. Emerg Infect Dis. 2016;22:565–567.
Younossi ZM, Birerdinc A, Henry L. Hepatitis C infection: a multi-faceted systemic disease with clinical, patient reported and economic consequences. J Hepatol. 2016;65:S109–S119.
Wiesner RH. Patient selection in an era of donor liver shortage: current US policy. Nat Clin Pract Gastroenterol Hepatol. 2005;2:24–30.
Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470.
Singal AK, Fang X, Kaif M, et al. Primary biliary cirrhosis has high wait-list mortality among patients listed for liver transplantation. Transpl Int. 2017;30:454–462.
Shukla A, Vadeyar H, Rela M, Shah S. Liver transplantation: East versus West. J Clin Exp Hepatol. 2013;3:243–253.
Alqahtani SA, Larson AM. Adult liver transplantation in the USA. Curr Opin Gastroenterol. 2011;27:240–247.
Verna EC. Hepatitis viruses and liver transplantation: evolving trends in antiviral management. Clin Liver Dis. 2014;18:575–601.
Lee J, Belanger A, Doucette JT, et al. Transplantation trends in primary biliary cirrhosis. Clin Gastroenterol Hepatol. 2007;5:1313–1315.
Tabibian JH, Lindor KD. Primary biliary cirrhosis: safety and benefits of established and emerging therapies. Expert Opin Drug Saf. 2015;14:1435–1444.
Beuers U, Lindor KD. A major step towards effective treatment evaluation in primary biliary cirrhosis. J Hepatol. 2011;55:1178–1180.
Genda T, Ichida T, Sakisaka S, et al. Waiting list mortality of patients with primary biliary cirrhosis in the Japanese transplant allocation system. J Gastroenterol. 2014;49:324–331.
Heimbach JK, Hirose R, Stock PG, et al. Delayed hepatocellular carcinoma model for end-stage liver disease exception score improves disparity in access to liver transplant in the United States. Hepatology. 2015;61:1643–1650.
Schöning W, Schmeding M, Ulmer F, Andert A, Neumann U. Liver transplantation for patients with cholestatic liver diseases. Viszeralmedizin. 2015;31:194–198.
Kuiper EMM, Hansen BE, Metselaar HJ, et al. Trends in liver transplantation for primary biliary cirrhosis in the Netherlands 1988–2008. BMC Gastroenterol. 2010;10:144.
Staufer K, Kivaranovic D, Rasoul-Rockenschaub S, et al. Waitlist mortality and post-transplant survival in patients with cholestatic liver disease—impact of changes in allocation policy. HPB. 2018;20:916–924.
Younossi Z, Stepanova M, Golabi P, et al. Factors associated with progressive course of patients with primary biliary cholangitis in the United States: data from a large-real world database. Gastroenterology. 2018;154:S-1097.
Ding X, Xu Y, Wang Y, et al. Nonalcoholic fatty liver disease and associated metabolic risks of hypertension in type 2 diabetes: a cross-sectional community-based study. Int J Endocrinol. 2017;2017:5262560.
Webb GJ, Rana A, Hodson J, et al. Twenty-year comparative analysis of patients with autoimmune liver diseases on transplant waitlists. Clin Gastroenterol Hepatol. 2018;16:278–287.
Milkiewicz P, Wunsch E, Elias E. Liver transplantation in chronic cholestatic conditions. Front Biosci. 2012;17:959–969.
Lu M, Zhou Y, Haller IV, et al. Increasing prevalence of primary biliary cholangitis and reduced mortality with treatment. Clin Gastroenterol Hepatol.. 2018;16(8):1342–1350.
Singal AK, Guturu P, Hmoud B, et al. Evolving frequency and outcomes of liver transplantation based on etiology of liver disease. Transplantation. 2013;95:755–760.
Levy C. Primary biliary cholangitis guidance update: implications for liver transplantation. Liver Transpl. 2018;1:1. https://doi.org/10.1002/lt.25321.
Kashyap R, Safadjou S, Chen R, et al. Living donor and deceased donor liver transplantation for autoimmune and cholestatic liver diseases–an analysis of the UNOS database. J Gastrointest Surg. 2010;14:1362–1369.
Adam R, Karam V, Delvart V, et al. Improved survival in liver transplant recipients receiving prolonged-release tacrolimus in the European Liver Transplant Registry. Am J Transpl. 2015;15:1267–1282.
Egawa H, Sakisaka S, Teramukai S, et al. Long-term outcomes of living-donor liver transplantation for primary biliary cirrhosis: a Japanese multicenter study. Am J Transpl. 2016;16:1248–1257.
Acknowledgments
The data reported here have been supplied by the Minneapolis Medical Research Foundation (MMRF) as the contractor for the Scientific Registry of Transplant Recipients (SRTR). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Funding
The study was funded by Intercept Pharmaceutical and the Center for Outcomes Research in Liver Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ZMY is a consultant to BMS, Gilead, AbbVie, Intercept, and GSK. All other authors of this manuscript have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sayiner, M., Stepanova, M., De Avila, L. et al. Outcomes of Liver Transplant Candidates with Primary Biliary Cholangitis: The Data from the Scientific Registry of Transplant Recipients. Dig Dis Sci 65, 416–422 (2020). https://doi.org/10.1007/s10620-019-05786-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05786-1