Abstract
Background
Acute pancreatitis (AP) is a common and expensive condition. Improving quality of care in AP is vital to minimizing cost and improving patient outcomes. However, there has been little work accomplished toward developing and validating explicit quality indicators (QIs) in AP.
Aims
To define quality of care in patients with AP by developing explicit QIs using standardized techniques.
Methods
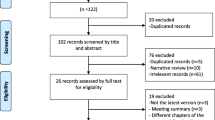
We used the UCLA/RAND Delphi panel approach to combine a comprehensive literature review with the collective judgment of experts to identify a defined set of process measures for AP.
Results
We produced 164 candidate QIs after a comprehensive literature review. After Delphi review, 75 had a median rating ≥ 7. We excluded 11 QIs where the disagreement index exceeded 1.0 and combined indicators overlapping in content to produce a final list of 22 QIs. Overall, 8 QIs related to diagnosis, prevention, or determination of etiology, 2 QIs focused on determination of severity, 3 QIs captured fluid resuscitation, 2 QIs measured nutrition, 1 QI use of antibiotics, and 6 QIs captured endoscopic or surgical management.
Conclusions
We have developed 22 QIs spanning the spectrum of AP management including diagnosis, risk stratification, and pharmacological and endoscopic therapy. These QIs will facilitate future quality improvement by practitioners and organizations who treat patients with AP and further identify areas that are amenable to improvement to enhance patient care. We anticipate that this QI set will represent the first step in determining a framework for demonstrating value in the care of patients with AP.
Similar content being viewed by others
Abbreviations
- AP:
-
Acute pancreatitis
- Apache:
-
Acute Physiology and Chronic Health Examination
- ACG:
-
American College of Gastroenterology
- AGA:
-
American Gastroenterological Association
- APA:
-
American Pancreatic Association
- ASGE:
-
American Society for Gastrointestinal Endoscopy
- BISAP:
-
Bedside index for severity in acute pancreatitis
- BUN:
-
Blood urea nitrogen
- CRP:
-
C-reactive protein
- CECT:
-
Contrast-enhanced CT
- Cr:
-
Creatinine
- DI:
-
Disagreement index
- EMR:
-
Electronic medical records
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- HCT:
-
Hematocrit
- IAP:
-
International Association of Pancreatology
- PN:
-
Parenteral nutrition
- PEP:
-
Post-ERCP pancreatitis
- QIs:
-
Quality indicators
- SIRS:
-
Systemic inflammatory response syndrome
- WON:
-
Walled-off necrosis
References
Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187. e3.
Lowenfels AB, Sullivan T, Fiorianti J, Maisonneuve P. The epidemiology and impact of pancreatic diseases in the United States. Curr Gastroenterol Rep. 2005;7:90–95.
Brown A, Young B, Morton J, Behrns K, Shaheen N. Are health related outcomes in acute pancreatitis improving? An analysis of national trends in the U.S. from 1997 to 2003. JOP. 2008;9:408–414.
Shaheen NJ, Hansen RA, Morgan DR, et al. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 2006;101:2128–2138.
Krishna SG, Kamboj AK, Hart PA, Hinton A, Conwell DL. The changing epidemiology of acute pancreatitis hospitalizations: a decade of trends and the impact of chronic pancreatitis. Pancreas. 2017;46:482–488.
Forsmark CE, Baillie J, Practice AGAIC, Economics C, Board AGAIG. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–2044.
Committee ASoP, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of cystic pancreatic neoplasms. Gastrointest Endosc. 2016;84:1–9.
Working Group IAPAPAAPG. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013;13:e1–e15.
Tenner S, Baillie J, DeWitt J, Vege SS, American College of G. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415. 16.
Vlada AC, Schmit B, Perry A, Trevino JG, Behrns KE, Hughes SJ. Failure to follow evidence-based best practice guidelines in the treatment of severe acute pancreatitis. HPB (Oxford). 2013;15:822–827.
Sun E, Tharakan M, Kapoor S, et al. Poor compliance with ACG guidelines for nutrition and antibiotics in the management of acute pancreatitis: a North American survey of gastrointestinal specialists and primary care physicians. JOP. 2013;14:221–227.
Asch SM, McGlynn EA, Hiatt L, et al. Quality of care for hypertension in the United States. BMC Cardiovasc Disord. 2005;5:1.
Asch SM, Kerr EA, Lapuerta P, Law A, McGlynn EA. A new approach for measuring quality of care for women with hypertension. Arch Intern Med. 2001;161:1329–1335.
Feachem RG, Sekhri NK, White KL. Getting more for their dollar: a comparison of the NHS with California’s Kaiser Permanente. BMJ. 2002;324:135–141.
Ragnarsson T, Andersson R, Ansari D, Persson U, Andersson B. Acute biliary pancreatitis: focus on recurrence rate and costs when current guidelines are not complied. Scand J Gastroenterol. 2017;52:264–269.
Lawson EH, Gibbons MM, Ko CY, Shekelle PG. The appropriateness method has acceptable reliability and validity for assessing overuse and underuse of surgical procedures. J Clin Epidemiol. 2012;65:1133–1143.
Kanwal F, Barkun A, Gralnek IM, et al. Measuring quality of care in patients with nonvariceal upper gastrointestinal hemorrhage: development of an explicit quality indicator set. Am J Gastroenterol. 2010;105:1710–1718.
Kanwal F, Kramer J, Asch SM, et al. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010;8:709–717.
Melmed GY, Siegel CA, Spiegel BM, et al. Quality indicators for inflammatory bowel disease: development of process and outcome measures. Inflamm Bowel Dis. 2013;19:662–668.
Santana MJ, Stelfox HT, Trauma Quality Indicator Consensus P. Development and evaluation of evidence-informed quality indicators for adult injury care. Ann Surg. 2014;259:186–192.
Mazzone PJ, Vachani A, Chang A, et al. Quality indicators for the evaluation of patients with lung cancer. Chest. 2014;146:659–669.
Sharma P, Katzka DA, Gupta N, et al. Quality indicators for the management of Barrett’s esophagus, dysplasia, and esophageal adenocarcinoma: international consensus recommendations from the American Gastroenterological Association Symposium. Gastroenterology. 2015;149:1599–1606.
Edwards JJ, Khanna M, Jordan KP, Jordan JL, Bedson J, Dziedzic KS. Quality indicators for the primary care of osteoarthritis: a systematic review. Ann Rheum Dis. 2015;74:490–498.
Shekelle PG, Chassin MR, Park RE. Assessing the predictive validity of the RAND/UCLA appropriateness method criteria for performing carotid endarterectomy. Int J Technol Assess Health Care. 1998;14:707–727.
The Rand/UCLA appropriateness method user’s manual. Santa Monica, CA: RAND Corporation. 2001.
Lankisch PG, Assmus C, Lehnick D, Maisonneuve P, Lowenfels AB. Acute pancreatitis: does gender matter? Dig Dis Sci. 2001;46:2470–2474. https://doi.org/10.1023/A:1012332121574.
Gullo L, Migliori M, Olah A, et al. Acute pancreatitis in five European countries: etiology and mortality. Pancreas. 2002;24:223–227.
Wang SS, Lin XZ, Tsai YT, et al. Clinical significance of ultrasonography, computed tomography, and biochemical tests in the rapid diagnosis of gallstone-related pancreatitis: a prospective study. Pancreas. 1988;3:153–158.
Steinberg W, Tenner S. Acute pancreatitis. N Engl J Med. 1994;330:1198–1210.
Ammann RW. The natural history of alcoholic chronic pancreatitis. Intern Med. 2001;40:368–375.
Fortson MR, Freedman SN, Webster PD 3rd. Clinical assessment of hyperlipidemic pancreatitis. Am J Gastroenterol. 1995;90:2134–2139.
Chait A, Brunzell JD. Severe hypertriglyceridemia: role of familial and acquired disorders. Metabolism. 1983;32:209–214.
Levy MJ, Geenen JE. Idiopathic acute recurrent pancreatitis. Am J Gastroenterol. 2001;96:2540–2555.
Kohler H, Lankisch PG. Acute pancreatitis and hyperamylasaemia in pancreatic carcinoma. Pancreas. 1987;2:117–119.
Lin A, Feller ER. Pancreatic carcinoma as a cause of unexplained pancreatitis: report of ten cases. Ann Intern Med. 1990;113:166–167.
Mujica VR, Barkin JS, Go VL. Acute pancreatitis secondary to pancreatic carcinoma. Study Group Participants. Pancreas. 2000;21:329–332.
Choudhary CPFE, Sherman S, Lehman GA. Idiopathic pancreatitis: yield of ERCP correlated with patient age. Am J Gastroenterol. 1998;93:1654A.
DiMagno MJ, Dimagno EP. Pancreas divisum does not cause pancreatitis, but associates with CFTR mutations. Am J Gastroenterol. 2012;107:318–320.
Koziel D, Gluszek S, Kowalik A, Chlopek M, Pieciak L. Genetic mutations in SPINK1, CFTR, CTRC genes in acute pancreatitis. BMC Gastroenterol. 2015;15:70.
Tran DD, Cuesta MA. Evaluation of severity in patients with acute pancreatitis. Am J Gastroenterol. 1992;87:604–608.
Papachristou GI, Muddana V, Yadav D, et al. Comparison of BISAP, Ranson’s, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol. 2010;105:435–441. quiz 42.
Garg PK, Madan K, Pande GK, et al. Association of extent and infection of pancreatic necrosis with organ failure and death in acute necrotizing pancreatitis. Clin Gastroenterol Hepatol. 2005;3:159–166.
Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990;174:331–336.
London NJ, Leese T, Lavelle JM, et al. Rapid-bolus contrast-enhanced dynamic computed tomography in acute pancreatitis: a prospective study. Br J Surg. 1991;78:1452–1456.
Wu BU, Hwang JQ, Gardner TH, et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:710–717. e1.
Brown A, Orav J, Banks PA. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas. 2000;20:367–372.
Lankisch PG, Mahlke R, Blum T, et al. Hemoconcentration: an early marker of severe and/or necrotizing pancreatitis? A critical appraisal. Am J Gastroenterol. 2001;96:2081–2085.
Koutroumpakis E, Wu BU, Bakker OJ, et al. Admission hematocrit and rise in blood urea nitrogen at 24 h outperform other laboratory markers in predicting persistent organ failure and pancreatic necrosis in acute pancreatitis: a post hoc analysis of three large prospective databases. Am J Gastroenterol. 2015;110:1707–1716.
Eckerwall GE, Tingstedt BB, Bergenzaun PE, Andersson RG. Immediate oral feeding in patients with mild acute pancreatitis is safe and may accelerate recovery—a randomized clinical study. Clin Nutr. 2007;26:758–763.
Meng WB, Li X, Li YM, Zhou WC, Zhu XL. Three initial diets for management of mild acute pancreatitis: a meta-analysis. World J Gastroenterol. 2011;17:4235–4241.
Yi F, Ge L, Zhao J, et al. Meta-analysis: total parenteral nutrition versus total enteral nutrition in predicted severe acute pancreatitis. Intern Med. 2012;51:523–530.
Al-Omran M, Albalawi ZH, Tashkandi MF, Al-Ansary LA. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst Rev. 2010;1:CD002837.
Li JY, Yu T, Chen GC, et al. Enteral nutrition within 48 hours of admission improves clinical outcomes of acute pancreatitis by reducing complications: a meta-analysis. PLoS ONE. 2013;8:e64926.
Bakker OJ, van Brunschot S, van Santvoort HC, et al. Early versus on-demand nasoenteric tube feeding in acute pancreatitis. N Engl J Med. 2014;371:1983–1993.
Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011;46:261–270.
Tse F, Yuan Y. Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev. 2012;5:CD009779.
Moretti A, Papi C, Aratari A, et al. Is early endoscopic retrograde cholangiopancreatography useful in the management of acute biliary pancreatitis? A meta-analysis of randomized controlled trials. Dig Liver Dis. 2008;40:379–385.
Larson SD, Nealon WH, Evers BM. Management of gallstone pancreatitis. Adv Surg. 2006;40:265–284.
Gurusamy KS, Nagendran M, Davidson BR. Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev. 2013;9:CD010326.
Davidson BR, Neoptolemos JP, Carr-Locke DL. Endoscopic sphincterotomy for common bile duct calculi in patients with gall bladder in situ considered unfit for surgery. Gut. 1988;29:114–120.
Freeman ML, Werner J, van Santvoort HC, et al. Interventions for necrotizing pancreatitis: summary of a multidisciplinary consensus conference. Pancreas. 2012;41:1176–1194.
Committee ASoP, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of inflammatory pancreatic fluid collections. Gastrointest Endosc. 2016;83:481–488.
van Santvoort HC, Besselink MG, Bakker OJ, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med. 2010;362:1491–1502.
Gurusamy KS, Belgaumkar AP, Haswell A, Pereira SP, Davidson BR. Interventions for necrotising pancreatitis. Cochrane Database Syst Rev. 2016;4:CD011383.
Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366:1414–1422.
Levenick JM, Gordon SR, Fadden LL, et al. Rectal indomethacin does not prevent post-ERCP pancreatitis in consecutive patients. Gastroenterology. 2016;150:911–917. quiz e19.
Luo H, Zhao L, Leung J, et al. Routine pre-procedural rectal indometacin versus selective post-procedural rectal indometacin to prevent pancreatitis in patients undergoing endoscopic retrograde cholangiopancreatography: a multicentre, single-blinded, randomised controlled trial. Lancet. 2016;387:2293–2301.
Thiruvengadam NR, Forde KA, Ma GK, et al. Rectal indomethacin reduces pancreatitis in high- and low-risk patients undergoing endoscopic retrograde cholangiopancreatography. Gastroenterology. 2016;151:288–297. e4.
Wall I, Badalov N, Baradarian R, Iswara K, Li JJ, Tenner S. Decreased mortality in acute pancreatitis related to early aggressive hydration. Pancreas. 2011;40:547–550.
Gardner TB, Vege SS, Chari ST, et al. Faster rate of initial fluid resuscitation in severe acute pancreatitis diminishes in-hospital mortality. Pancreatology. 2009;9:770–776.
Warndorf MG, Kurtzman JT, Bartel MJ, et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:705–709.
Green R, Charman SC, Palser T. Early definitive treatment rate as a quality indicator of care in acute gallstone pancreatitis. Br J Surg. 2017;104:1686–1694.
Author information
Authors and Affiliations
Contributions
Gyanprakash Ketwaroo MD involved in study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis. Robert Jay Sealock MD took part in study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis. Steven Freedman MD PhD contributed to acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Phil A. Hart MD took part in acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Mohamed Othman MD involved in acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Wahid Wassef MD took part in acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Peter Banks MD contributed to acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Santhi Swaroop Vege MD contributed to acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Timothy Gardner MD MS involved in acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Dhiraj Yadav MD contributed to acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Sunil Sheth MD involved in acquisition of data; analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Fasiha Kanwal MD, MSHS took part in study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ketwaroo, G., Sealock, R.J., Freedman, S. et al. Quality of Care Indicators in Patients with Acute Pancreatitis. Dig Dis Sci 64, 2514–2526 (2019). https://doi.org/10.1007/s10620-019-05674-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05674-8