Abstract
Background
Eosinophilic gastroenteritis (EGE) is a rare, chronic inflammatory condition of the gastrointestinal tract. Little is known about its natural history and treatment outcomes. The aims of our analysis were to describe clinical presentation, response to current medical treatments, and to evaluate the response of refractory EGE to anti-integrin therapy.
Methods
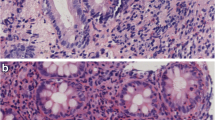
Patients with confirmed diagnosis of EGE fulfilling the diagnostic criteria: (1) the presence of gastrointestinal symptoms, (2) dense eosinophilic infiltration of the gastrointestinal mucosa, and (3) exclusion of other conditions leading to gastrointestinal eosinophilia were included in this analysis. In patients non-responding to corticosteroids and/or anti-TNF treatment the integrin blocker vedolizumab was used.
Results
EGE patients (n = 22) were predominantly female (63%) with a median age at diagnosis of 41.5 years. The most frequent symptoms were abdominal pain (100%), diarrhea (59%), nausea/vomiting (36%), and bloating (27%). No pathognomonic endoscopic alterations were found. Eosinophilic infiltration was observed in the majority of patients in more than one segment. Patients were treated with systemic steroids, topical, and enteral release steroids in 21/22 (95%) patients, proton pump inhibitors in 7/22 (32%), TNFα inhibitors in 3/22 (14%), and vedolizumab in 4/22 (18%) patients. In 3/4 of steroid-refractory patients vedolizumab induced a clinical and histological improvement.
Conclusions
The combination of highly variable clinical presentation, subtle endoscopic abnormalities, and involvement of several GI segments undermines the difficulty to diagnose EGE and the need for structured biopsy sampling. Corticosteroids were efficient in the majority of patients to induce remission. Response to the integrin blocker vedolizumab suggests further assessment in refractory cases.




Similar content being viewed by others
Abbreviations
- EoE:
-
Eosinophilic esophagitis
- EGE:
-
Eosinophilic gastroenteritis
- EGIDS:
-
Eosinophilic gastrointestinal diseases
- HPF:
-
High power field
- IgE:
-
Immunoglobulin E
- PGA:
-
Patient global assessment
- PPI:
-
Proton pump inhibitor
- TNFα:
-
Tumor necrosis factor alpha
References
Klein NC, Hargrove RL, Sleisenger MH, et al. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299–319.
Zur Kenntnis der allergischen RK. Affektionen des Verdaungskanal von Standpunkt des Chirurgen aus. Arch Klin Chir. 1937;188.
Yan BM, Shaffer EA. Primary eosinophilic disorders of the gastrointestinal tract. Gut. 2009;58:721–732.
Mansoor E, Saleh MA, Cooper GS. Prevalence of eosinophilic gastroenteritis and colitis in a population-based study, from 2012 to 2017. Clin Gastroenterol Hepatol. 2017;15:1733–1741.
Reed C, Woosley JT, Dellon ES. Clinical characteristics, treatment outcomes, and resource utilization in children and adults with eosinophilic gastroenteritis. Dig Liver Dis. 2015;47:197–201.
Walker MM, Potter M, Talley NJ. Eosinophilic gastroenteritis and other eosinophilic gut diseases distal to the oesophagus. Lancet Gastroenterol Hepatol. 2018;3:271–280.
DeBrosse CW, Case JW, Putnam PE, et al. Quantity and distribution of eosinophils in the gastrointestinal tract of children. Pediatr Dev Pathol. 2006;9:210–218.
Lwin T, Melton SD, Genta RM. Eosinophilic gastritis: histopathological characterization and quantification of the normal gastric eosinophil content. Mod Pathol. 2011;24:556–563.
Matsushita T, Maruyama R, Ishikawa N, et al. The number and distribution of eosinophils in the adult human gastrointestinal tract: a study and comparison of racial and environmental factors. Am J Surg Pathol. 2015;39:521–527.
Pineton de Chambrun G, Gonzalez F, Canva JY, et al. Natural history of eosinophilic gastroenteritis. Clin Gastroenterol Hepatol. 2011;9:950–956.
Kinoshita Y, Furuta K, Ishimaura N, et al. Clinical characteristics of Japanese patients with eosinophilic esophagitis and eosinophilic gastroenteritis. J Gastroenterol. 2013;48:333–339.
Ko HM, Morotti RA, Yershov O, et al. Eosinophilic gastritis in children: clinicopathological correlation, disease course, and response to therapy. Am J Gastroenterol. 2014;109:1277–1285.
Bischoff SC, Mayer J, Nguyen QT, et al. Immunnohistological assessment of intestinal eosinophil activation in patients with eosinophilic gastroenteritis and inflammatory bowel disease. Am J Gastroenterol. 1999;94:3521–3529.
Kephart GM, Alexander JA, Arora AS, et al. Marked deposition of eosinophil-derived neurotoxin in adult patients with eosinophilic esophagitis. Am J Gastroenterol. 2010;105:298–307.
Torpier G, Colombel JF, Mathieu-Chandelier C, et al. Eosinophilic gastroenteritis: ultrastructural evidence for a selective release of eosinophil major basic protein. Clin Exp Immunol. 1988;74:404–408.
Zhang L, Duan L, Ding S, et al. Eosinophilic gastroenteritis: clinical manifestations and morphological characteristics, a retrospective study of 42 patients. Scand J Gastroenterol. 2011;46:1074–1080.
Attar A, Cazals-Hatem D, Ponsot P. Videocapsule endoscopy identifies stenoses missed by other imaging techniques in a patient with eosinophilic gastroenteritis. Clin Gastroenterol Hepatol. 2011;9:A28.
Pasha SF, Leighton JA, Williams JW, et al. Capsule retention in a patient with eosinophilic gastroenteritis mimicking diaphragm disease of the small bowel. Endoscopy. 2009;41:E290–E291.
Talley NJ, Walker MM, Aro P, et al. Non-ulcer dyspepsia and duodenal eosinophilia: an adult endoscopic population-based case-control study. Clin Gastroenterol Hepatol. 2007;5:1175–1183.
Egan M, Furuta GT. Eosinophilic gastrointestinal diseases beyond eosinophilic esophagitis. Ann Allergy Asthma Immunol. 2018;121:162–167.
Collins MH, Capocelli K, Yang GY. Eosinophilic gastrointestinal disorders pathology. Front Med (Lausanne). 2017;4:261.
Greuter T, Bussmann C, Safroneeva E, et al. Long-term treatment of eosinophilic esophagitis with swallowed topical corticosteroids: development and evaluation of a therapeutic concept. Am J Gastroenterol. 2017;112:1527–1535.
Muir A, Surrey L, Kriegermeier A, et al. Severe eosinophilic gastroenteritis in a Crohn’s disease patient treated with infliximab and adalimumab. Am J Gastroenterol. 2016;111:437–438.
Redondo-Cerezo E, Cabello MJ, Gonzalez Y, et al. Eosinophilic gastroenteritis: our recent experience: one-year experience of atypical onset of an uncommon disease. Scand J Gastroenterol. 2001;36:1358–1360.
Turner D, Wolters VM, Russell RK, et al. Anti-TNF, infliximab, and adalimumab can be effective in eosinophilic bowel disease. J Pediatr Gastroenterol Nutr. 2013;56:492–497.
Amiot A, Grimaud JC, Peyrin-Biroulet L, et al. Effectiveness and safety of vedolizumab induction therapy for patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2016;14:e2.
Feagan BG, Rutgeerts P, Sands BE, et al. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369:699–710.
Loftus EV Jr, Colombel JF, Feagan BG, et al. Long-term efficacy of vedolizumab for ulcerative colitis. J Crohns Colitis. 2017;11:400–411.
Sandborn WJ, Feagan BG, Rutgeerts P, et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2013;369:711–721.
Vermeire S, Loftus EV Jr, Colombel JF, et al. Long-term efficacy of vedolizumab for Crohn’s disease. J Crohns Colitis. 2017;11:412–424.
Rieder F, Biancani P, Harnett K, et al. Inflammatory mediators in gastroesophageal reflux disease: impact on esophageal motility, fibrosis, and carcinogenesis. Am J Physiol Gastrointest Liver Physiol. 2010;298:G571–G581.
Kim HP, Reed CC, Herfarth HH, et al. Vedolizumab treatment may reduce steroid burden and improve histology in patients with eosinophilic gastroenteritis. Clin Gastroenterol Hepatol. 2018;16:1992–1994.
Author information
Authors and Affiliations
Contributions
PH and AS conceptualized and designed the clinical question and drafted the initial manuscript; TG and LB evaluated the patient data and drafted the initial manuscript; CB performed histological analysis and critically reviewed the manuscript. All authors read and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Grandinetti, T., Biedermann, L., Bussmann, C. et al. Eosinophilic Gastroenteritis: Clinical Manifestation, Natural Course, and Evaluation of Treatment with Corticosteroids and Vedolizumab. Dig Dis Sci 64, 2231–2241 (2019). https://doi.org/10.1007/s10620-019-05617-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05617-3