Abstract
Background
EphA3 is a member of Eph receptors, which is involved in tumorigenesis. The expression and clinical significance of EphA3 in colorectal cancer (CRC) have not been fully investigated.
Methods
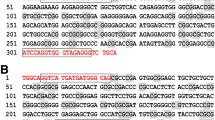
Four colon cancer cell lines and a set of CRC tissues were examined for EphA3 expression. The methylation status of a CpG island within the EphA3 promoter, the presence of four somatic EPHA3 mutations, and EPHA3 gene copy number variations were also analyzed in colon cancer cell lines.
Results
EphA3 expression was lost in all colon cancer cell lines examined. EphA3 expression was lower in tumor tissues when compared with normal intestinal tissues (P < 0.001). A comparison of EphA3 immunohistochemical scores for tumor and matched normal intestinal tissues revealed that the protein was downregulated in 82/164 (50.0%), unchanged in 52/164 (31.7%), and upregulated in 30/164 (18.3%) cases of CRC. EphA3 expression was negatively associated with lymph node metastasis (P =0.014, rs=− 0.192) and TNM stage (P =0.001, rs=− 0.260). Downregulation of expression was more common in older patients (P =0.013, rs=0.193). Methylated promoter DNA was detected in all four colon cancer cell lines. Somatic mutations or EphA3 gene deletion was not detected.
Conclusions
EphA3 was downregulated in the majority of CRC. Hypermethylation of a CpG island within the EPHA3 promoter provides a possible mechanism. Loss of EphA3 expression was associated with lymph node metastasis and TNM stage and may therefore prove useful as a predictor for tumor spread in CRC.





Similar content being viewed by others
References
Surawska H, Ma PC, Salgia R. The role of ephrins and Eph receptors in cancer. Cytokine Growth Factor Rev. 2004;15:419–433. https://doi.org/10.1016/j.cytogfr.2004.09.002.
Eph Nomenclature Committee. Unified nomenclature for Eph family receptors and their ligands, the ephrins. Cell. 1997;90:403–404.
Pasquale EB. Eph–ephrin bidirectional signaling in physiology and disease. Cell. 2008;133:38–52. https://doi.org/10.1016/j.cell.2008.03.011.
Egea J, Klein R. Bidirectional Eph–ephrin signaling during axon guidance. Trends Cell Biol. 2007;17:230–238. https://doi.org/10.1016/j.tcb.2007.03.004.
Batlle E, Henderson JT, Beghtel H, et al. Beta-catenin and TCF mediate cell positioning in the intestinal epithelium by controlling the expression of EphB/ephrinB. Cell. 2002;111:251–263.
Batlle E, Bacani J, Begthel H, et al. EphB receptor activity suppresses colorectal cancer progression. Nature. 2005;435:1126–1130. https://doi.org/10.1038/nature03626.
Li S, Wu Z, Ma P, et al. Ligand-dependent EphA7 signaling inhibits prostate tumor growth and progression. Cell Death Dis. 2017;8:e3122. https://doi.org/10.1038/cddis.2017.507.
Husa AM, Magic Z, Larsson M, Fornander T, Perez-Tenorio G. EPH/ephrin profile and EPHB2 expression predicts patient survival in breast cancer. Oncotarget. 2016;7:21362–21380. https://doi.org/10.18632/oncotarget.7246.
Bai YQ, Zhang JY, Bai CY, et al. Low EphA7 expression correlated with lymph node metastasis and poor prognosis of patients with esophageal squamous cell carcinoma. Acta Histochem Cytochem. 2015;48:75–81. https://doi.org/10.1267/ahc.14054.
Theocharis S, Klijanienko J, Giaginis C, Alexandrou P, Patsouris E, Sastre-Garau X. Ephrin receptor (Eph)-A1, -A2, -A4 and -A7 expression in mobile tongue squamous cell carcinoma: associations with clinicopathological parameters and patients survival. Pathol Oncol Res. 2014;20:277–284. https://doi.org/10.1007/s12253-013-9692-3.
Giaginis C, Tsoukalas N, Bournakis E, et al. Ephrin (Eph) receptor A1, A4, A5 and A7 expression in human non-small cell lung carcinoma: associations with clinicopathological parameters, tumor proliferative capacity and patients’ survival. BMC Clin Pathol. 2014;14:8. https://doi.org/10.1186/1472-6890-14-8.
Boyd AW, Ward LD, Wicks IP, et al. Isolation and characterization of a novel receptor-type protein tyrosine kinase (hek) from a human pre-B cell line. J Biol Chem. 1992;267:3262–3267.
Nasri B, Inokuchi M, Ishikawa T, et al. High expression of EphA3 (erythropoietin-producing hepatocellular A3) in gastric cancer is associated with metastasis and poor survival. BMC Clin Pathol. 2017;17:8. https://doi.org/10.1186/s12907-017-0047-y.
Lu CY, Yang ZX, Zhou L, et al. High levels of EphA3 expression are associated with high invasive capacity and poor overall survival in hepatocellular carcinoma. Oncol Rep. 2013;30:2179–2186. https://doi.org/10.3892/or.2013.2679.
Clifford N, Smith LM, Powell J, Gattenlohner S, Marx A, O’Connor R. The EphA3 receptor is expressed in a subset of rhabdomyosarcoma cell lines and suppresses cell adhesion and migration. J Cell Biochem. 2008;105:1250–1259. https://doi.org/10.1002/jcb.21926.
Wang X, Xu H, Cao G, Wu Z, Wang J. Loss of EphA3 protein expression is associated with advanced TNM stage in clear-cell renal cell carcinoma. Clin Genitourin Cancer. 2017;15:e169–e173. https://doi.org/10.1016/j.clgc.2016.07.028.
Zhuang G, Song W, Amato K, et al. Effects of cancer-associated EPHA3 mutations on lung cancer. J Natl Cancer Inst. 2012;104:1182–1197. https://doi.org/10.1093/jnci/djs297.
Lisabeth EM, Fernandez C, Pasquale EB. Cancer somatic mutations disrupt functions of the EphA3 receptor tyrosine kinase through multiple mechanisms. Biochemistry. 2012;51:1464–1475. https://doi.org/10.1021/bi2014079.
Guan M, Liu L, Zhao X, et al. Copy number variations of EphA3 are associated with multiple types of hematologic malignancies. Clin Lymphoma Myeloma Leuk. 2011;11:50–53. https://doi.org/10.3816/clml.2011.n.006.
Xi HQ, Zhao P. Clinicopathological significance and prognostic value of EphA3 and CD133 expression in colorectal carcinoma. J Clin Pathol. 2011;64:498–503. https://doi.org/10.1136/jcp.2010.087213.
Li M, Yang C, Liu X, et al. EphA3 promotes malignant transformation of colorectal epithelial cells by upregulating oncogenic pathways. Cancer Lett. 2016;383:195–203. https://doi.org/10.1016/j.canlet.2016.10.004.
Andretta E, Carton-Garcia F, Martinez-Barriocanal A, et al. Investigation of the role of tyrosine kinase receptor EPHA3 in colorectal cancer. Sci Rep. 2017;7:41576. https://doi.org/10.1038/srep41576.
Dottori M, Down M, Huttmann A, Fitzpatrick DR, Boyd AW. Cloning and characterization of EphA3 (Hek) gene promoter: DNA methylation regulates expression in hematopoietic tumor cells. Blood. 1999;94:2477–2486.
Wood LD, Calhoun ES, Silliman N, et al. Somatic mutations of GUCY2F, EPHA3, and NTRK3 in human cancers. Hum Mutat. 2006;27:1060–1061. https://doi.org/10.1002/humu.9452.
Davies H, Hunter C, Smith R, et al. Somatic mutations of the protein kinase gene family in human lung cancer. Cancer Res. 2005;65:7591–7595. https://doi.org/10.1158/0008-5472.can-05-1855.
Bardelli A, Parsons DW, Silliman N, et al. Mutational analysis of the tyrosine kinome in colorectal cancers. Science. 2003;300:949. https://doi.org/10.1126/science.1082596.
Uyan O, Omur O, Agim ZS, et al. Genome-wide copy number variation in sporadic amyotrophic lateral sclerosis in the Turkish population: deletion of EPHA3 is a possible protective factor. PLoS ONE. 2013;8:e72381. https://doi.org/10.1371/journal.pone.0072381.
Acknowledgments
The authors wish to thank the patients who participated in this study. This study was supported by Grants from the National Natural Science Foundation of China (81371611) and the National Basic Research Priorities Program 973 Project (2014CB744504) from the Ministry of Science and Technology of China. We thank James Monypenny, PhD, from Liwen Bianji, Edanz Group China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, Y., Xuan, Z., Wang, B. et al. EphA3 Downregulation by Hypermethylation Associated with Lymph Node Metastasis and TNM Stage in Colorectal Cancer. Dig Dis Sci 64, 1514–1522 (2019). https://doi.org/10.1007/s10620-018-5421-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5421-9