Abstract
Background and Aims
Various gastrointestinal societies have released guidelines on the evaluation of asymptomatic pancreatic cysts (PCs). These guidelines differ on several aspects, which create a conundrum for clinicians. The aim of this study was to evaluate preferences and practice patterns in the management of incidental PCs in light of these societal recommendations.
Methods
An electronic survey distributed to members of the American Society for Gastrointestinal Endoscopy (ASGE). Main outcomes included practice setting (academic vs. community), preferences for evaluation, management, and surveillance strategies for PCs.
Results
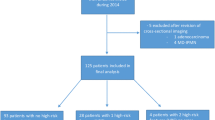
A total of 172 subjects completed the study (52% academic-based endoscopists). Eighty-six (50%) and 138 (80%) of the participants responded that they would recommend EUS surveillance of incidental PCs measuring less than 2 cm and 3 cm, respectively. Nearly half of the endosonographers (42.5% community and 44% academic; p = 1.0) would routinely perform FNA on PCs without any high-risk features. More academic-based endoscopists (57% academic vs. 32% community; p = 0.001) would continue incidental PC surveillance indefinitely.
Conclusions
There is significant variability in the approach of incidental PCs among clinicians, with practice patterns often diverging from the various GI societal guideline recommendations. Most survey respondents would routinely recommend EUS-FNA and indefinite surveillance for incidental PCs without high-risk features. The indiscriminate use of EUS-FNA and indefinite surveillance of all incidental PCs is not cost-effective, exposes the patient to unnecessary testing, and can further perpetuate diagnostic uncertainty. Well-designed studies are needed to improve our diagnostic and risk stratification accuracy in order to formulate a consensus on the management of these incidental PCs.



Similar content being viewed by others
Abbreviations
- AGA:
-
American Gastroenterological Association
- ASGE:
-
American Society of Gastrointestinal Endoscopy
- CT:
-
Computed tomography
- EUS:
-
Endoscopic ultrasound
- EUS-FNA:
-
Endoscopic ultrasound with fine-needle aspiration
- MRI:
-
Magnetic resonance imaging
- PCs:
-
Pancreatic cysts
References
Lee KS, Sekhar A, Rofsky NM, Pedrosa I. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010;105:2079–2084.
Canto MI, Hruban RH, Fishman EK, et al. Frequent detection of pancreatic lesions in asymptomatic high-risk individuals. Gastroenterology. 2012;142:796–804.
Brugge WR, Lauwers GY, Sahani D, Fernandez-del Castillo C, Warshaw AL. Cystic neoplasms of the pancreas. N Engl J Med. 2004;351:1218–1226.
Khashab MA, Kim K, Lennon AM, et al. Should we do EUS/FNA on patients with pancreatic cysts? The incremental diagnostic yield of EUS over CT/MRI for prediction of cystic neoplasms. Pancreas. 2013;42:717–721.
Scheiman JM, Hwang JH, Moayyedi P. American gastroenterological association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148:824–848.e22.
Elta GH, Enestvedt BK, Sauer BG, Lennon AM. ACG clinical guideline: diagnosis and management of pancreatic cysts. Am J Gastroenterol. 2018;113(4):464–479.
Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–197.
Lee KH, Kim EY, Cho J, et al. Risk Factors associated with adverse events during endoscopic ultrasound-guided tissue sampling. PLoS ONE. 2017;12:e0189347.
Siddiqui AA, Shahid H, Shah A, et al. High risk of acute pancreatitis after endoscopic ultrasound-guided fine needle aspiration of side branch intraductal papillary mucinous neoplasms. Endoscopic Ultrasound. 2015;4:109.
Pergolini I, Sahora K, Ferrone CR, et al. Long-term risk of pancreatic malignancy in patients with branch duct intraductal papillary mucinous neoplasm in a referral center. Gastroenterology. 2017;153:1284.e1–1294.e1.
Kwong WT, Hunt GC, Fehmi SM, et al. Low rates of malignancy and mortality in asymptomatic patients with suspected neoplastic pancreatic cysts beyond 5 years of surveillance. Clin Gastroenterol Hepatol. 2016;14:865–871.
Han Y, Lee H, Kang JS, et al. Progression of pancreatic branch duct intraductal papillary mucinous neoplasm associates with cyst size. Gastroenterology. 2017;154:576–584.
Lawrence SA, Attiyeh MA, Seier K, et al. Should patients with cystic lesions of the pancreas undergo long-term radiographic surveillance? Ann Surg. 2017;266:536–544.
Imbe K, Nagata N, Hisada Y, et al. Validation of the American Gastroenterological Association guidelines on management of intraductal papillary mucinous neoplasms: more than 5 years of follow-up. Eur Radiol. 2018;28:170–178.
Alkaade S, Chahla E, Levy M. Role of endoscopic ultrasound-guided fine-needle aspiration cytology, viscosity, and carcinoembryonic antigen in pancreatic cyst fluid. Endosc. Ultrasound. 2015;4:299.
Brugge WR, Lewandrowski K, Lee-Lewandrowski E, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004;126:1330–1336.
Samarasena J, Chen C, Chin M, Chang K, Lee J. Successful closure of a cryotherapy-induced bleeding jejunal perforation with the over-the-scope clip system. Gastrointest Endosc. 2017;85:451.
Coman RM, Schlachterman A, Esnakula AK, Draganov PV, Yang D. EUS-guided, through-the-needle forceps: clenching down the diagnosis. Gastrointest Endosc. 2016;84:372–373.
Attili F, Pagliari D, Rimbaș M, et al. Endoscopic ultrasound-guided histological diagnosis of a mucinous non-neoplastic pancreatic cyst using a specially designed through-the-needle microforceps. Endoscopy. 2016;48:E188–E189.
Huelsen A, Cooper C, Saad N, Gupta S. Endoscopic ultrasound-guided, through-the-needle forceps biopsy in the assessment of an incidental large pancreatic cystic lesion with prior inconclusive fine-needle aspiration. Endoscopy. 2017;49:E109–E110.
Mittal C, Obuch JC, Hammad H, et al. Technical feasibility, diagnostic yield, and safety of microforceps biopsies during EUS evaluation of pancreatic cystic lesions (with video). Gastrointest Endosc. 2018;87:1263–1269.
Author information
Authors and Affiliations
Contributions
DW, DY, and PD conceived of the presented idea and developed the theory. DW and DY wrote the survey questions. NK, VK, JF, and AG computed and ran the statistics. DW, PD, DY, and CF wrote the manuscript and all revisions. DY gave final approval.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have relevant disclosures or conflicts of interest to declare related to this study.
Rights and permissions
About this article
Cite this article
Westerveld, D., Goddard, A., Harris, N. et al. Survey Study on the Practice Patterns of the Evaluation and Management of Incidental Pancreatic Cysts. Dig Dis Sci 64, 689–697 (2019). https://doi.org/10.1007/s10620-018-5368-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5368-x