Abstract
Background
The etiology of Crohn’s disease (CD) is still unknown although new theories are based on defects in innate immunity. We have previously shown a decrease in γδ T cells in CD patients. Previous studies have shown a high prevalence of anti-A. simplex immunoglobulins in CD patients. The diminution of γδ T cells in the peripheral blood and intestinal mucosa of CD patients may create a state of immunosuppression that would facilitate A. simplex infection.
Aims
To study the antibody responses to Anisakis antigens in Crohn’s disease patients and its relationship with αβ and γδ T cell subsets.
Methods
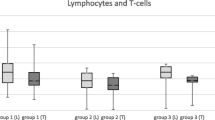
We recruited 81 CD patients and 81 healthy controls. αβ and γδ T cell subsets and anti-A. simplex antibodies were measured.
Results
Levels of anti-A. simplex IgG and IgM were significantly increased in CD patients. Almost 20% of CD patients were positive for IgG and IgM anti-A. simplex versus only 3.7 and 2.5%, respectively, in normal subjects. However, lower specific IgA levels were observed in the group of CD patients versus healthy subjects. We found an association between CD3 + CD8 + γδ subset and IgM anti-A. simplex levels. In ileal cases and stricturing behavior of CD, we observed the highest levels of specific antibodies with the exception of anti-A. simplex IgA.
Conclusions
The relationship of specific antibodies with a γδ T cell deficiency makes these cell candidates to play a role in the immune response against Anisakis. In addition, anti-Anisakis antibodies could be considered as markers of risk of progression in CD.


Similar content being viewed by others
Abbreviations
- CD:
-
Crohn’s disease
References
Korzenik JR. Is Crohn’s disease due to defective immunity. Gut. 2007;56:2–5.
Marks DJ. Defective innate immunity in inflammatory bowel disease: a Crohn’s disease exclusivity? Curr Opin Gastroenterol. 2011;27:328–334.
Saito H, Kranz DM, Takagaki Y, et al. Complete primary structure of a heterodimeric T-cell receptor deduced from cDNA sequences. Nature. 1984;309:757–762.
Goodman T, Lefrançois L. Expression of the gamma-delta T-cell receptor on intestinal CD8 + intraepithelial lymphocytes. Nature. 1988;333:855–858.
Andreu-Ballester JC, Amigó-García V, Catalán-Serra I, et al. Deficit of gammadelta T lymphocytes in the peripheral blood of patients with Crohn’s disease. Dig Dis Sci. 2011;56:2613–2622. doi:10.1007/s10620-011-1636-8.
Lee HB, Kim JH, Yim CY, et al. Differences in immunophenotyping of mucosal lymphocytes between ulcerative colitis and Crohn’s disease. Korean J Intern Med. 1997;12:7–15.
Sartor RB. Microbial factors in the pathogenesis os Crohn’s disease, ulcerative colitis and experimental intestinal inflammation. In: Kirsner JB, Shorter RJ, eds. Inflmmatory Bowel disease. 4rd ed. Baltimore: Williams and Wilkins. 1995:96–124.
Daschner A, Alonso-Gómez A, Cabañas R, et al. Gastroallergic anisakiasis: borderline between food allergy and parasitic disease-clinical and allergologic evaluation of 20 patients with confirmed acute parasitism by Anisakis simplex. J Allergy Clin Immunol. 2000;105:176–181.
Puente P, Anadón AM, Rodero M, et al. Anisakis simplex: the high prevalence in Madrid (Spain) and its relation with fish consumption. Exp Parasitol. 2008;118:271–274.
Sakanari JA. Anisakis-from the platter to the microfuge. Parasitol Today. 1990;6:323–327.
Audicana MT, Kennedy MW. Anisakis simplex: from obscure infectious worm to inducer of immune hypersensitivity. Clin Microbiol Rev. 2008;21:360–379.
Guillén-Bueno R, Gutiérrez-Ramos R, Perteguer-Prieto MJ, et al. Anti-Anisakis Antibodies in the Clinical course of Crohn’s disease. Digestion. 1999; 268–73.
García-Palacios L, González ML, Esteban MI, et al. Enzyme-linked immunosorbent assay, immunoblot analysis and RAST fluoroimmunoassay analysis of serum responses against crude larval antigens of Anisakis simplex in a Spanish random population. J Helminthol. 1996;70:281–289.
Daschner A, Cuéllar C, Sánchez-Pastor S, et al. Gastroallergic anisakiasis as a consequence of simultaneous primary and secondary immune response. Parasite Immunol. 2002;24:243–251.
Gutiérrez R, Cuéllar C. Immunoglobulins anti-Anisakis simplex in patients with gastrointestinal disease. J Helminthol. 2002;76:131–136.
Martínez de Velasco G, Rodero M, Chivato T, et al. Seroprevalence of anti-Kudoa sp. (Myxosporea: Multivalvulida) antibodies in a Spanish population. Parasitol Res. 2006;100:1205–1211.
Andreu-Ballester JC, García-Ballesteros C, Benet-Campos C, et al. Values for αβ and γδ T-lymphocytes and CD4+, CD8+, and CD56+ subsets in healthy adult subjects: assessment by age and gender. Cytometry B Clin Cytom. 2012;82:238–244.
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.
Shivananda S, Lennard-Jones J, Logan R, et al. Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD). Gut. 1996;39:690–697.
Saro-Gismera C, Riestra-Menéndez S, Milla-Crespo A, et al. Incidence and prevalence of inflammatory bowel disease. Asturian study in 5 areas (EIICEA). Spain. An. Med. Interna. 2003;20:3–9.
Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis: a pathologic and clinical entity. JAMA. 1932;99:1323.
ENNA. Encuesta de Presupuestos Familiares. Estudio Nacional de Nutrición y Alimentación 1991. Madrid I.N.I. 1995.
EFSA Panel on Biological Hazards (BIOHAZ); Scientific Opinion on risk assessment of parasites in fishery products. EFSA J. 2010;8:1543–1633.
Valiñas B, Lorenzo S, Eiras A, et al. Prevalence of and risk factors for IgE sensitization to Anisakis simplex in a Spanish population. Allergy. 2001;56:667–671.
Fernandez de Corres L, Del Pozo MD, Aizpuru F, et al. Prevalencia de la sensibilización a Anisakis simplex en tres áreas españolas, en relación a las diferentes tasas de consumo de pescado Relevancia de la alergia a Anisakis simplex. Alergología e Inmunología Clínica. 2001;16:337–346.
Del Rey A, Valero A, Mayorga C, et al. Sensitization to Anisakis simplex s.l. in a healthy population. Acta Trop. 2006;97:265–269.
Andreu-Ballester JC, Pérez-Griera J, Ballester F, et al. Anisakis simplex and Kudoa sp.: evaluation of specific antibodies in appendectomized patients. Exp Parasitol. 2008;119:433–436.
Knoflach P, Park BH, Cunningham R, et al. Serum antibodies to cow’s milk proteins in ulcerative colitis and Crohn’s disease. Gastroenterology. 1987;92:479–485.
Paganelli R, Pallone F, Montano S, et al. Isotypic analysis of antibody response to a food antigen in inflammatory bowel disease. Int Arch Allergy Appl Immunol. 1985;78:81–85.
Main J, McKenzie H, Yeaman GR, et al. Antibody to Saccharomyces cerevisiae (baker’s yeast) in Crohn’s disease. BMJ. 1988;297:1105–1106.
Tanaka K, Kawamura H, Tohgi N, et al. The measurement of Ascaris suum protein by radioimmunoassay in sera from patients with helminthiasis and with gastrointestinal diseases. Parasitology. 1983;86:291–300.
Frehn L, Jansen A, Bennek E, et al. Distinct patterns of IgG and IgA against food and microbial antigens in serum and feces of patients with inflammatory bowel diseases. PLoS ONE. 2014;9:e106750.
Xiong Y, Wang GZ, Zhou JQ, et al. Serum antibodies to microbial antigens for Crohn’s disease progression: a meta-analysis. Eur J Gastroenterol Hepatol. 2014;26:733–742.
Antoni L, Nuding S, Wehkamp J, et al. Intestinal barrier in inflammatory bowel disease. World J Gastroenterol. 2014;20:1165–1179.
Whitacre CC, Reingold SC, O’Looney PA. A gender gap in autoimmunity. Science. 1999;283:1277–1278.
Niewiadomski O, Studd C, Hair C, et al. Prospective population-based cohort of inflammatory bowel disease in the biologics era: disease course and predictors of severity. J Gastroenterol Hepatol. 2015;30:1346–1353.
Romberg-Camps MJ, Dagnelie PC, Kester AD, et al. Influence of phenotype at diagnosis and of other potential prognostic factors on the course of inflammatory bowel disease. Am J Gastroenterol. 2009;104:371–383.
Klebl FH, Bataille F, Bertea CR, et al. Association of perinuclear antineutrophil cytoplasmic antibodies and anti-Saccharomyces cerevisiae antibodies with Vienna classification subtypes of Crohn’s disease. Inflamm Bowel Dis. 2003;9:302–307.
Baron L, Branca G, Trombetta C, et al. Intestinal anisakidosis: histopathological findings and differential diagnosis. Pathol Res Pract. 2014;210:746–750.
Montalto M, Miele L, Marcheggiano A, et al. Anisakis infestation: a case of acute abdomen mimicking Crohn’s disease and eosinophilic gastroenteritis. Dig Liver Dis. 2005;37:62–64.
Bavastrelli M, Riccardo F, Binazzi R, et al. Small intestine anisakiasis. J Ital Med Trop. 2001;6:4950.
Andreu-Ballester JC, Garcia-Ballesteros C, Amigo V, et al. Microsporidia and its relation to Crohn’s disease. A retrospective study. PLoS ONE. 2013;8:e62107.
Compliance with ethical standards
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
C. Benet-Campos and C. Cuellar contributed equally to this work and should be considered equal first authors.
Rights and permissions
About this article
Cite this article
Benet-Campos, C., Cuéllar, C., García-Ballesteros, C. et al. Determination of Anti-Anisakis Simplex Antibodies and Relationship with αβ and γδ Lymphocyte Subpopulations in Patients with Crohn’s Disease. Dig Dis Sci 62, 934–943 (2017). https://doi.org/10.1007/s10620-017-4473-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4473-6