Abstract
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is generally recommended for removal of CBD stones. There were no studies focusing on the role of symptoms related to CBD stone in performing endoscopic stone removal. The aim of our study was to compare outcomes and complications of ERCP between asymptomatic and symptomatic CBD stones.
Methods
The medical records of 568 patients with naïve papilla who underwent ERCP for treatment of CBD stone from Jan 2009 to Aug 2014 were reviewed and analyzed retrospectively. Patients were divided as asymptomatic group (n = 32) and symptomatic group (n = 536).
Results
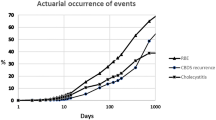
Age and gender were not significantly different between the two groups (p > 0.005). Mean sizes of CBD and CBD stones were not significantly different between asymptomatic and symptomatic group (p > 0.05). No differences in performance of needle knife fistulotomy, endoscopic sphincterotomy, and endoscopic papillary balloon dilatation were observed between the two groups (p > 0.05). Unintentional injection into the pancreatic duct was not significantly different between the two groups (p > 0.05). The overall complete stone removal rate was 96.9 % in the asymptomatic group and 94.4 % in the symptomatic group (p = 0.295). Requirement of mechanical lithotripsy was not significantly different between asymptomatic and symptomatic group (18.8 vs 8.4 %, p = 0.057). Significantly higher incidence of post-ERCP pancreatitis was observed in the asymptomatic group than in the symptomatic group (12.5 vs 3.9 %, p = 0.045).
Conclusion
The overall success rates of CBD stone removal were comparable between asymptomatic and symptomatic patients. However, risk of post-ERCP pancreatitis appears to be increased in patients with asymptomatic CBD stones.
Similar content being viewed by others
References
Murison MS, Gartell PC, McGinn FP. Does selective peroperative cholangiography result in missed common bile duct stones? J R Coll Surg Edinb. 1993;38:220–224.
Caddy GR, Kirby J, Kirk SJ, et al. Natural history of asymptomatic bile duct stones at time of cholecystectomy. Ulst Med J. 2005;74:108–112.
Frossard JL, Hadengue A, Amouyal G, et al. Choledocholithiasis: a prospective study of spontaneous common bile duct stone migration. Gastrointest Endosc. 2000;51:175–179.
Moller M, Gustafsson U, Rasmussen F, et al. Natural course vs interventions to clear common bile duct stones: data from the Swedish Registry for Gallstone Surgery and Endoscopic Retrograde Cholangiopancreatography (GallRiks). JAMA Surg. 2014;149:1008–1013.
Internal Clinical Guidelines T. National Institute for Health and Clinical Excellence: Guidance. Gallstone Disease: Diagnosis and Management of Cholelithiasis, Cholecystitis and Choledocholithiasis. London: National Institute for Health and Care Excellence (UK), Copyright (c) National Clinical Guideline Centre; 2014.
Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781–1788.
Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393.
Vitek L, Carey MC. New pathophysiological concepts underlying pathogenesis of pigment gallstones. Clin Res Hepatol Gastroenterol. 2012;36:122–129.
Wang P, Li ZS, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31–40.
Cotton PB, Garrow DA, Gallagher J, et al. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80–88.
Glomsaker T, Hoff G, Kvaloy JT, et al. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013;100:373–380.
Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423.
Christensen M, Matzen P, Schulze S, et al. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721–731.
Katsinelos P, Chatzimavroudis G, Tziomalos K, et al. Impact of periampullary diverticula on the outcome and fluoroscopy time in endoscopic retrograde cholangiopancreatography. Hepatobiliary Pancreat Dis Int. 2013;12:408–414.
Choudhary A, Bechtold ML, Arif M, et al. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: a meta-analysis and systematic review. Gastrointest Endosc. 2011;73:275–282.
Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139–147.
Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425–434.
Acknowledgments
This work was supported by the 2014 Yeungnam University Research Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Kim, S.B., Kim, K.H. & Kim, T.N. Comparison of Outcomes and Complications of Endoscopic Common Bile Duct Stone Removal Between Asymptomatic and Symptomatic Patients. Dig Dis Sci 61, 1172–1177 (2016). https://doi.org/10.1007/s10620-015-3965-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3965-5