Abstract
Background and Aim
The American Association for the Study of Liver Disease (AASLD) recommends screening for esophageal varices (EV) by esophagoduodenoscopy (EGD) in patients with cirrhosis to guide decisions regarding primary prophylaxis for EV hemorrhage. We aimed to identify patient and facility factors associated with EV screening in veterans with hepatitis C (HCV)-associated cirrhosis.
Methods
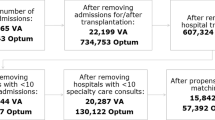
This was a population-based cohort study. Veterans with HCV and newly diagnosed cirrhosis between 1/1/2004 and 12/31/2005 and followed until 12/31/2011 were included. The primary outcome was receipt of EGD within 1 year of cirrhosis diagnosis. Patient- and facility-level factors associated with EV screening were determined.
Results
A total of 4230 patients with HCV cirrhosis were identified. During median follow-up of 6.1 years (IQR: 4.0–8.0), 21.5 % developed a decompensating event, and 38.3 % died. Fifty-four percent received an EGD, and 33.8 % had an EGD within guidelines. Median time from cirrhosis diagnosis to EGD was 72 days (IQR: 12–176). Factors independently associated with receipt of EV screening were a decompensation event (OR 1.16, CI 1.01–1.32) and gastroenterology/hepatology clinic access (OR 2.1, CI 1.73–2.46), whereas cardiovascular (OR 0.81, CI 0.69–0.95), mental health (OR 0.79, CI 0.68–0.91), and respiratory (OR 0.85, CI 0.72–0.99) comorbidities were associated with reduced likelihood of EV screening.
Conclusion
EV screening per AASLD guidelines occurs in only one-third of patients. This missed opportunity was strongly associated with access to gastroenterology/hepatology specialty care. Additionally, providers may be relying on clinical cues (i.e., decompensation) to prompt referral for endoscopy suggesting education to improve compliance with guidelines is needed.

Similar content being viewed by others
References
El-Serag HB, Everhart JE. Improved survival after variceal hemorrhage over an 11-year period in the Department of Veterans Affairs. Am J Gastroenterol. 2000;95:3566–3573.
Carbonell N, Pauwels A, Serfaty L, Fourdan O, Levy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40:652–659.
de Franchis R, Primignani M. Natural history of portal hypertension in patients with cirrhosis. Clin Liver Dis. 2001;5:645–663.
Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, et al. Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–938.
Bernard B, Lebrec D, Mathurin P, Opolon P, Poynard T. Beta-adrenergic antagonists in the prevention of gastrointestinal rebleeding in patients with cirrhosis: a meta-analysis. Hepatology. 1997;25:63–70.
Pascal JP, Cales P. Propranolol in the prevention of first upper gastrointestinal tract hemorrhage in patients with cirrhosis of the liver and esophageal varices. N Engl J Med. 1987;317:856–861.
Khuroo MS, Khuroo NS, Farahat KL, Khuroo YS, Sofi AA, Dahab ST. Meta-analysis: endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol Ther. 2005;21:347–361.
D’Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332–354.
Kovalak M, Lake J, Mattek N, Eisen G, Lieberman D, Zaman A. Endoscopic screening for varices in cirrhotic patients: data from a national endoscopic database. Gastrointest Endosc. 2007;65:82–88.
Buchanan PM, Kramer JR, El-Serag HB, Asch SM, et al. The quality of care provided to patients with varices in the department of Veterans Affairs. Am J Gastroenterol. 2014;109:934–940.
Dominitz JA, Boyko EJ, Koepsell TD, Heagerty PJ, et al. Elevated prevalence of hepatitis C infection in users of United States veterans medical centers. Hepatology. 2005;41:88–96.
Backus LI, Gavrilov S, Loomis TP, Halloran JP, et al. Clinical Case Registries: simultaneous local and national disease registries for population quality management. J Am Med Inform Assoc. 2009;16:775–783.
Davila JA, Morgan RO, Richardson PA, Du XL, McGlynn KA, El-Serag HB. Use of surveillance for hepatocellular carcinoma among patients with cirrhosis in the United States. Hepatology. 2010;52:132–141.
Goldberg D, Lewis J, Halpern S, Weiner M, et al. Validation of three coding algorithms to identify patients with end-stage liver disease in an administrative database. Pharmacoepidemiol Drug Saf. 2012;21:765–769.
Rongey C, Shen H, Hamilton N, Backus LI, Asch SM, Knight S. Impact of rural residence and health system structure on quality of liver care. PLoS One. 2013;8:e84826.
West AN, Lee RE, Shambaugh-Miller MD, Bair BD, et al. Defining “rural” for veterans’ health care planning. J Rural Health. 2010;26:301–309.
Waghray A, Waghray N, Kyprianou A, Menon KVN. Variceal screening in cirrhotic patients. Hepatology 2014; 60(S1); Abstract 1594.
Moodley J, Lopez R, Carey W. Compliance with practice guidelines and risk of a first esophageal variceal hemorrhage in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010;8:703–708.
Berzigotti A, Seijo S, Arena U, Abraldes JG, et al. Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Gastroenterology. 2013;144:102–111.
Zambam de Mattos A, Alves de Mattos A, Daros LF, Musskopf MI. Aspartate aminotransferase-to-platelet ratio index (APRI) for the non-invasive prediction of esophageal varices. Ann Hepatol. 2013;12:810–814.
Tafarel JR, Tolentino LH, Correa LM, Bonilha DR, et al. Prediction of esophageal varices in hepatic cirrhosis by noninvasive markers. Eur J Gastroenterol Hepatol. 2011;23:754–758.
Takuma Y, Nouso K, Morimoto Y, Tomokuni J, et al. Measurement of spleen stiffness by acoustic radiation force impulse imaging identifies cirrhotic patients with esophageal varices. Gastroenterology. 2013;144:92–101.
Saab S, DeRosa V, Nieto J, Durazo F, Han S, Roth B. Costs and clinical outcomes of primary prophylaxis of variceal bleeding in patients with hepatic cirrhosis: a decision analytic model. Am J Gastroenterol. 2003;98:763–770.
Serste T, Melot C, Francoz C, Durand F, et al. Deleterious effects of beta-blockers on survival in patients with cirrhosis and refractory ascites. Hepatology. 2010;52:1017–1022.
Mandorfer M, Bota S, Schwabl P, Bucsics T, et al. Nonselective beta blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology. 2014;146:1680–1690.
Arrowsmith JB, Gerstman BB, Fleischer DE, Benjamin SB. Results from the American Society for Gastrointestinal Endoscopy/U.S. Food and Drug Administration collaborative study on complication rates and drug use during gastrointestinal endoscopy. Gastrointest Endosc. 1991;37:421–427.
Johnson PA, Campbell DR, Antonson CW, Weston AP, Shuler FN, Lozoff RD. Complications associated with endoscopic band ligation of esophageal varices. Gastrointest Endosc. 1993;39:181–185.
Daneshmend TK, Bell GD, Logan RF. Sedation for upper gastrointestinal endoscopy: results of a nationwide survey. Gut. 1991;32:12–15.
Lim RG, Cobell WJ, Theivanayagam S, Kilgore TW, et al. Endoscopy after acute myocardial infarction: an evaluation of safety. South Med J. 2013;106:545–549.
Spier BJ, Said A, Moncher K, Pfau PR. Safety of endoscopy after myocardial infarction based on cardiovascular risk categories: a retrospective analysis of 135 patients at a tertiary referral medical center. J Clin Gastroenterol. 2007;41:462–467.
DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–2107.
Ratib S, Fleming KM, Crooks CJ, Aithal GP, West J. 1 and 5 year survival estimates for people with cirrhosis of the liver in England, 1998–2009: a large population study. J Hepatol. 2014;60:282–289.
Acknowledgments
The authors would like to thank Dr. David Goldberg for his expertise and suggestions regarding the VA CCR. This study was supported in part by the Canadian Association for the Study of the Liver (CASL)/Merck Clinical Hepatology Fellowship (JAF). This publication was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2 TR000143. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Flemming, J.A., Saxena, V., Shen, H. et al. Facility- and Patient-Level Factors Associated with Esophageal Variceal Screening in the USA. Dig Dis Sci 61, 62–69 (2016). https://doi.org/10.1007/s10620-015-3865-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3865-8