Abstract
Background and Aims
The transpapillary approach can be used for draining pancreatic pseudocysts (PPs) with pancreatic-duct abnormalities. The purpose of this study was to analyze prognostic factors for clinical success of transpapillary drainage.
Patients and Methods
Data for all patients who underwent transpapillary drainage between November 2000 and September 2009 were obtained by retrospective review and entered into a computerized database. Patient data were prospectively followed up to determine long-term outcomes.
Results
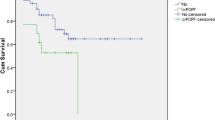
Seventy interventional ERCP procedures were performed for 43 patients. Technical success was 90.7 % (39/43). Overall clinical success was 79.5 % (31/39). Clinical success for pancreatic head pseudocyst was significantly different from that for body or tail pseudocyst (62.5 vs. 91.3 %, P = 0.043). Logistic regression analysis showed that location of the PPs predicted the success of endoscopic transpapillary pseudocyst drainage (P = 0.025).
Conclusion
Transpapillary drainage is the least traumatic approach for drainage of PPs, and is also effective for patients with no communicating pseudocysts. Clinical success for pancreatic body or tail pseudocyst drainage was higher than that for pancreatic head pseudocyst drainage. It was found that the location of PPs predicted the success of transpapillary pseudocyst drainage. None of the other factors tested was a significant predictor of clinical success.
Similar content being viewed by others
References
Soliani P, Franzini C, Ziegler S, et al. Pancreatic pseudocysts following acute pancreatitis: risk factors influencing therapeutic outcomes. JOP. 2004;5:338–347.
Baron TH. Endoscopic drainage of pancreatic fluid collections and pancreatic necrosis. Tech Gastrointest Endosc. 2004;6:91–99.
Rosso E, Alexakis N, Ghaneh P, et al. Pancreatic pseudocyst in chronic pancreatitis: endoscopic and surgical treatment. Dig Surg. 2003;20:397–406.
Nealon WH, Walser E. Duct drainage alone is sufficient in the operative management of pancreatic pseudocyst in patients with chronic pancreatitis. Ann Surg. 2003;237:614–620.
Bhasin DK, Rana SS, Rao C, et al. Endoscopic management of pancreatic injury due to abdominal trauma. JOP. 2012;13:187–192.
Smits ME, Rauws EA, Tytgat GN, Huibregtse K. The efficacy of endoscopic treatment of pancreatic pseudocysts. Gastrointest Endosc. 1995;42:202–207.
Catalano MF, Geenen JE, Schmalz MJ, et al. Treatment of pancreatic pseudocysts with ductal communication by transpapillary pancreatic duct endoprosthesis. Gastrointest Endosc. 1995;42:214–218.
Libera ED, Siqueira ES, Morais M, et al. Pancreatic pseudocysts transpapillary and transmural drainage. HPB Surg. 2000;11:333–338.
Bradley EL III. A clinically based classification system for acute pancreatitis: summary of the international symposium on acute pancreatitis, Atlanta, Ga, September 11 through 13, 1992. Arch Surg. 1993;128:586–590.
Varadarajulu S, Christein JD, Tamhane A, et al. Prospective randomized trial comparing EUS and EGD for transmural drainage of pancreatic pseudocysts (with videos). Gastrointest Endosc. 2008;68:1102–1111.
Lerch MM, Stier A, Wahnschaffe U, Mayerle J. Pancreatic pseudocysts: observation, endoscopic drainage, or resection? Dtsch Arztebl Int. 2009;106:614–621.
Nealon WH, Walser E. Main pancreatic ductal anatomy can direct choice of modality for treating pancreatic pseudocysts (surgery versus percutaneous drainage). Ann Surg. 2002;235:751–758.
Coelho DE, Ardengh JC, Carbalo MT, et al. Clinicopathologic characteristics and endoscopic treatment of post-traumatic pancreatic pseudocysts. Pancreas. 2011;40:469–473.
Güitrón-Cantú A, Adalid-Martínez R, Gutiérrez-Bermúdez JA. Transpapillary and transmural drainage of pancreatic pseudocysts. Rev Gastroenterol Mex. 2005;70:240–246.
Telford JJ, Farrell JJ, Saltzman JR, et al. Pancreatic stent placement for duct disruption. Gastrointest Endosc. 2002;56:18–24.
Barthet M, Sahel J, Bodiou-Bertei C, et al. Endoscopic transpapillary drainage of pancreatic pseudocysts. Gastrointest Endosc. 1995;42:208–213.
Ahearne PM, Baillie JM, Cotton PB, et al. An endoscopic retrograde cholangiopancreatography (ERCP)-based algorithm for the management of pancreatic pseudocysts. Am J Surg. 1992;163:111–115.
Bhasin DK, Rana SS, Nanda M, et al. Endoscopic management of pancreatic pseudocysts at atypical locations. Surg Endosc. 2010;24:1085–1091.
Bhasin DK, Rana SS, Rawal P. Endoscopic retrograde pancreatography in pancreatic trauma: need to break the mental barrier. J Gastroenterol Hepatol. 2009;24:720–728.
Barthet M, Bugallo M, Moreira LS, et al. Management of cysts and pseudocysts complicating chronic pancreatitis: a retrospective study of 143 patients. Gastroenterol Clin Biol. 1993;17:270–276.
Cahen D, Rauws E, Fockens P, et al. Endoscopic drainage of pancreatic pseudocysts: long-term outcome and procedural factors associated with safe and successful treatment. Endoscopy. 2005;37:977–983.
Hariri M, Slivka A, Carr-Locke DL, et al. Pseudocyst drainage predisposes to infection when pancreatic necrosis is unrecognized. Am J Gastroenterol. 1994;89:1781–1784.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, H., Zhan, XB., Jin, ZD. et al. Prognostic Factors for Successful Endoscopic Transpapillary Drainage of Pancreatic Pseudocysts. Dig Dis Sci 59, 459–464 (2014). https://doi.org/10.1007/s10620-013-2924-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2924-2