Abstract
Aim
Complication rates after laparoscopic cholecystectomy vary but are still reported to be up to 17 %. Identifying risk factors for an adverse complication outcome could help to reduce morbidity after laparoscopic cholecystectomy. Our aim was to analyze whether surgeon volume is a vital issue for complication outcome.
Methods
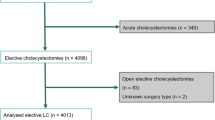
All complications—minor, major, local and general—were reviewed in a single institution between January 2004 and December 2008 and recorded in a database. Patient’s variables, disease related variables and surgeon’s variables were noted. The role of surgeon’s individual volume per year was analyzed. A stepwise logistic regression model was used.
Results
A total of 942 patients were analyzed, among which 70 (7 %) patients with acute cholecystitis and 52 (6 %) patients with delayed surgery for acute cholecystitis. Preoperative endoscopic retrograde cholangiography (ERC) had been performed in 142 (15 %) patients. Complication rates did not differ significantly for surgeon’s individual volume (≤10 vs. >10 LC/year, 5.2 vs. 8.2 %, p = 0.203) nor for specialization (laparoscopic vs. non-laparoscopic; 9.2 vs. 6.4 %, p = 0.085) and experience (specialty registration ≤5 vs. >5 years; 5.1 vs. 8.7 %, p = 0.069). The only significant predictors for complications were acute surgery (OR 3.9, 95 % CI 1.8–8.7, p = 0.001) and a history preceding laparoscopic cholecystectomy (LC) (ERC and delayed surgery for cholecystitis) (OR 8.1, 95 % CI 4.5–14.6: p <0.001).
Conclusion
Complications after LC were not significantly associated with a surgeon’s individual volume, but most prominently determined by the type of biliary disease.




Similar content being viewed by others
References
Finlayson EV, Goodney PP, Birkmeyer JD. Hospital volume and operative mortality in cancer surgery: a national study. Arch Surg. 2003;138:721–725.
Murphy MM, Ng SC, Simons JP, Csikesz NG, Shah SA, Tseng JF. Predictors of major complications after laparoscopic cholecystectomy: surgeon, hospital, or patient? J Am Coll Surg. 2010;211:73–80.
Shea JA, Healey MJ, Berlin JA, et al. Mortality and complications associated with laparoscopic cholecystectomy. A meta-analysis. Ann Surg. 1996;224:609–620.
Boerma D, Rauws EA, Keulemans YC, et al. Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: a prospective analysis. Ann Surg. 2001;234:750–757.
Connor S, Garden OJ. Bile duct injury in the era of laparoscopic cholecystectomy. Br J Surg. 2006;93:158–168.
de Reuver PR, Grossmann I, Busch OR, Obertop H, van Gulik TM, Gouma DJ. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Ann Surg. 2007;245:763–770.
Giger UF, Michel JM, Opitz I, Th ID, Kocher T, Krahenbuhl L. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg. 2006;203:723–728.
Murphy MM, Shah SA, Simons JP, et al. Predicting major complications after laparoscopic cholecystectomy: a simple risk score. J Gastrointest Surg. 2009;13:1929–1936.
de Vries A, Donkervoort SC, van Geloven AA, Pierik EG. Conversion rate of laparoscopic cholecystectomy after endoscopic retrograde cholangiography in the treatment of choledocholithiasis: does the time interval matter? Surg Endosc. 2005;19:996–1001.
Donkervoort SC, Dijksman LM, de Nes LC, Versluis PG, Derksen J, Gerhards MF. Outcome of laparoscopic cholecystectomy conversion: is the surgeon’s selection needed? Surg Endosc. 2012;26:2360–2366.
Boddy AP, Bennett JM, Ranka S, Rhodes M. Who should perform laparoscopic cholecystectomy? A 10-year audit. Surg Endosc. 2007;21:1492–1497.
Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 2006;93:844–853.
Kortram K, Reinders JS, Van RB, Wiezer MJ, Go PM, Boerma D. Laparoscopic cholecystectomy for acute cholecystitis should be performed by a laparoscopic surgeon. Surg Endosc. 2010;24:2206–2209.
Donkervoort SC, Van RO, Dijksman LM, van Geloven AA, Pierik EG. Identification of risk factors for an unfavorable laparoscopic cholecystectomy course after endoscopic retrograde cholangiography in the treatment of choledocholithiasis. Surg Endosc. 2010;24:798–804.
Dindo D, Dermartines N, Clavien PA. Classification of surgical complications. A new proposal with evaluation in a cohort of 6336 patients and results of survey. Ann Surg. 2004;240:205–213.
Brune IB, Schonleben K, Omran S. Complications after laparoscopic and conventional cholecystectomy: a comparative study. HPB Surg. 1994;8:19–25.
Csikesz N, Ricciardi R, Tseng JF, Shah SA. Current status of surgical management of acute cholecystitis in the United States. World J Surg. 2008;32:2230–2236.
Shamiyeh A, Danis J, Wayand W, Zehetner J. A 14-year analysis of laparoscopic cholecystectomy: conversion—when and why? Surg Laparosc Endosc Percutan Tech. 2007;17:271–276.
Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg. 1994;81:1362–1365.
Hasukic S, Mesic D, Dizdarevic E, Keser D, Hadziselimovic S, Bazardzanovic M. Pulmonary function after laparoscopic and open cholecystectomy. Surg Endosc. 2002;16:163–165.
Hendolin HI, Paakonen ME, Alhava EM, Tarvainen R, Kemppinen T, Lahtinen P. Laparoscopic or open cholecystectomy: a prospective randomised trial to compare postoperative pain, pulmonary function, and stress response. Eur J Surg. 2000;166:394–399.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donkervoort, S.C., Dijksman, L.M., Versluis, P.G. et al. Surgeon’s Volume Is Not Associated with Complication Outcome After Laparoscopic Cholecystectomy. Dig Dis Sci 59, 39–45 (2014). https://doi.org/10.1007/s10620-013-2885-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2885-5