Abstract
Background
Endoscopic retrograde cholangiopancreatography (ERCP), as with other fluoroscopic procedures, carries the risk of exposure of staff to radiation. However, over the last two decades, only a few studies have investigated this risk.
Objective
The aim of this work was to evaluate the dose of radiation exposure to staff participating in ERCP procedures in a busy teaching hospital that performs more than 1,850 procedures annually.
Methods
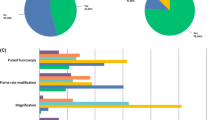
The entire ERCP staff consisted of the experienced endoscopist, the assistant, and two nurses who were responsible for monitoring patients as well as keeping their heads in position during the procedure. RAD DOSE NEB.226 dosimeters, which were provided by the Turkish Atomic Energy Authority, were used for this study.
Results
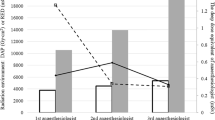
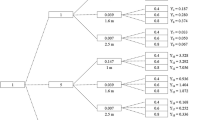
Data on 110 consecutive therapeutic ERCP procedures was recorded. The mean fluoroscopy time was 5.65 ± 4.71 min. The mean fluoroscopy time of the 61 procedures performed by an experienced endoscopist alone was 5.41 ± 4.65 min, whereas the mean fluoroscopy time for the 49 procedures during which an assistant was involved was 5.94 ± 4.81 min (p = 0.56). In terms of median dose of ionizing radiation exposure to the eyes, the dose measurement per procedure in which the primary endoscopist participated alone was 72 microsievert (μSv), compared to 92 μSv when an assistant took part in the proceedings. Considering that the recommended annual equivalent dose limit to the lens of the eye is 150 mSv, by performing 1,850 procedures annually, the primary endoscopist exceeds this limit.
Conclusions
Based on our results, taking into consideration the heavy workload in our hospital, it would seem that more experienced endoscopists are required to help provide training in ERCP, and that the use of lead acrylic goggles is required to decrease radiation exposure to the eyes.

Similar content being viewed by others
References
McCune WS, Shorb PE, Moscovitz H. Endoscopic cannulation of the ampulla of Vater: a preliminary report. Ann Surg. 1968;167:752–756.
Brugge WR, Van Dam J. Pancreatic and biliary endoscopy. N Engl J Med. 1999;341:1808–1816.
Campbell N, Sparrow K, Fortier M, Ponich T. Practical radiation safety and protection for the endoscopist during ERCP. Gastrointest Endosc. 2002;55:552–557.
Amis ES Jr. Risks of radiation exposure in the endoscopy suite: principles, cautions, and risks to patients and endoscopy staff. Tech Gastrointest Endosc. 2007;9:213–217.
International Commission on Radiation Protection. Radiation and your patient: a guide for medical practitioners. Ann ICRP. 2001;31:5–31.
International Commission on Radiation Protection. Chapter 5: The system of radiological protection of humans. Ann ICRP. 2007;37(2–4):81–101.
International Commission on Radiation Protection. Summary of recommendations. Ann ICRP. 1991;21(1–3):67–77.
Germanaud J, Legoux JL, Sabattier R, Causse X, Trinh DH. Radiation protection of operators during endoscopic retrograde cholangiopancreatography. Gastroenterol Clin Biol. 1993;17:259–263.
Martin CJ. A review of radiology staff doses and dose monitoring requirements. Radiat Prot Dosimetry. 2009;136:140–157.
Larkin CJ, Workman A, Wright RE, Tham TC. Radiation doses to patients during ERCP. Gastrointest Endosc. 2001;53:161–164.
Olgar T, Bor D, Berkmen G, Yazar T. Patient and staff doses for some complex x-ray examinations. J Radiol Prot. 2009;29:393–407.
Tsalafoutas IA, Paraskeva KD, Yakoumakis EN, Vassilaki AE, et al. Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Radiat Prot Dosimetry. 2003;106:241–246.
Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM. Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc. 1996;44:287–292.
Buls N, Pages J, Mana F, Osteaux M. Patient and staff exposure during endoscopic retrograde cholangiopancreatography. Br J Radiol. 2002;75:435–443.
Ruiz-Cruces R, Perez-Martinez M, Martin-Palanca A, Flores A, et al. Patient dose in radiologically guided interventional vascular procedures: conventional versus digital systems. Radiology. 1997;205:385–393.
McParland BJ. A study of patient radiation doses in interventional radiological procedures. Br J Radiol. 1998;71:175–185.
Sulieman A, Elzaki M, Khalil M. Occupational exposure to staff during endoscopic retrograde cholangiopancreatography in Sudan. Radiat Prot Dosimetry. 2011;144(1–4):530–533.
Cohen RV, Aldred MA, Paes WS, Fausto AM, et al. How safe is ERCP to the endoscopist? Surg Endosc. 1997;11:615–617.
Naidu LS, Singhal S, Preece DE, Vohrah A, Loft DE. Radiation exposure to personnel performing endoscopic retrograde cholangiopancreatography. Postgrad Med J. 2005;81:660–662.
Aroua A, Besancon A, Buchillier-Decka I, Trueb P, et al. Adult reference levels in diagnostic and interventional radiology for temporary use in Switzerland. Radiat Prot Dosimetry. 2004;111:289–295.
Hausler U, Czarwinski R, Brix G. Radiation exposure of medical staff from interventional X-ray procedures: a multicentre study. Eur Radiol. 2009;19:2000–2008.
Johlin FC, Pelsang RE, Greenleaf M. Phantom study to determine radiation exposure to medical personnel involved in ERCP fluoroscopy and its reduction through equipment and behavior modifications. Am J Gastroenterol. 2002;97:893–897.
Uradomo LT, Lustberg ME, Darwin PE. Effect of physician training on fluoroscopy time during ERCP. Dig Dis Sci. 2006;51:909–914.
Hoskins PR, Williams JR. Influence of radiologist grade on fluoroscopic patient dose. Br J Radiol. 1992;65:1119–1123.
Warren-Forward HM, Haddaway MJ, Temperton DH, McCall IW. Dose-area product readings for fluoroscopic and plain film examinations, including an analysis of the source of variation for barium enema examinations. Br J Radiol. 1998;71:961–967.
Vehmas T, Kuosma E. Influence of radiologists’ sex and training on fluoroscopy doses during barium enema. Br J Radiol. 2001;74:255–258.
Kim E, McLoughlin M, Lam EC, Amar J, et al. Prospective analysis of fluoroscopy duration during ERCP: critical determinants. Gastrointest Endosc. 2010;72:50–57.
Jorgensen JE, Rubenstein JH, Goodsitt MM, Elta GH. Radiation doses to ERCP patients are significantly lower with experienced endoscopists. Gastrointest Endosc. 2010;72:58–65.
http://www.taek.gov.tr/hizmetlerimiz/urunlerimiz/119-radyasyon-dozolcer.html.
Uradomo LT, Goldberg EM, Darwin PE. Time-limited fluoroscopy to reduce radiation exposure during ERCP: a prospective randomized trial. Gastrointest Endosc. 2007;66:84–89.
Chen MY, Van Swearingen FL, Mitchell R, Ott DJ. Radiation exposure during ERCP: effect of a protective shield. Gastrointest Endosc. 1996;43:1–5.
Vehmas T. Hawthorne effect: shortening of fluoroscopy times during radiation measurement studies. Br J Radiol. 1997;70:1053–1055.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oztas, E., Parlak, E., Kucukay, F. et al. The Impact of Endoscopic Retrograde Cholangiopancreatography Education on Radiation Exposure to Experienced Endoscopist: “Trainee Effect”. Dig Dis Sci 57, 1134–1143 (2012). https://doi.org/10.1007/s10620-012-2028-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2028-4