Abstract
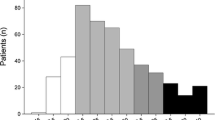
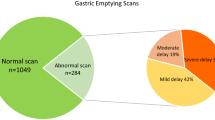
Purpose The natural history and outcome of patients with gastroparesis is not well known. The aim of this study was to identify the clinical or pathophysiological characteristics, if any, that may be helpful in predicting therapeutic response in this condition. Methods This is a retrospective study of a cohort of patients who presented to a tertiary referral center with symptoms suggestive of gastroparesis. All patients were evaluated by scintigraphic measurement of gastric emptying and symptoms were scored using a modification of the Gastroparesis Cardinal Symptom Index (GCSI). Treatment generally included conservative measures such as antiemetics, prokinetics, tricyclic antidepressants, and analgesics as well as various more invasive interventions in selected patients. Response to treatment was defined as a change in the overall GCSI score of two-thirds or more as compared with baseline. Results Out of a total of 93 patients, 69 patients met the eligibility criteria. Of these, 29 patients had diabetes mellitus and 40 patients had gastroparesis of nondiabetic etiology. Out of 69 patients, 49 were responders (71%) and 20 were nonresponders (29%). The cause (diabetic versus nondiabetic) of gastroparesis or the presence of delayed emptying did not correlate with response. However, the severity of stomach distension, bloating subscale score, and the global GCSI score at baseline presentation were predictive of response by multivariate analysis. Conclusion Higher global GCSI score, bloating subscale score, and severity of stomach distension at baseline presentation correlated with an unfavorable response in gastroparetic patients. On the other hand, neither the etiology of gastroparesis nor associated delay in gastric emptying appeared to be important in the clinical response. Patients with symptoms of typical gastroparesis but without delays in gastric emptying may have a distinct syndrome with a greater proportion of males than classical gastroparesis.
Similar content being viewed by others
References
Revicki D, Rentz A, Dubois D, et al. Gastroparesis cardinal symptom index (gcsi): development and validation of a patient reported assessment of severity of gastroparesis symptoms. Aliment Pharmacol Ther. 2003;18:141–150. doi:10.1046/j.1365-2036.2003.01612.x.
Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462. doi:10.1111/j.1572-0241.2000.02076.x.
Hoogerwerf W, Pasricha P, Kalloo A, Schuster M. Pain: the overlooked symptom in gastroparesis. Am J Gastroenterol. 1999;94:1029–1033. doi:10.1111/j.1572-0241.1999.01008.x.
Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352. doi:10.1016/S0016-5085(98)70012-5.
Boeckxstaens G, Hirsch D, Kuiken S, Heisterkamp S, Tytgat G. The proximal stomach and postprandial symptoms in functional dyspeptics. Am J Gastroenterol. 2002;97:40–48. doi:10.1111/j.1572-0241.2002.05421.x.
Kim D, Delgado-Aros S, Camilleri M, et al. Noninvasive measurement of gastric accommodation in patients with idiopathic nonulcer dyspepsia. Am J Gastroenterol. 2001;96:3099–3105. doi:10.1111/j.1572-0241.2001.05264.x.
Sarnelli G, Caenepeel P, Geypens B, Janssens J, Tack J. Symptoms associated with impaired gastric emptying of solids and liquids in functional dyspepsia. Am J Gastroenterol. 2003;98:783–788. doi:10.1111/j.1572-0241.2003.07389.x.
Stanghellini V, Tosetti C, Paternico A, et al. Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology. 1996;110:1036–1042. doi:10.1053/gast.1996.v110.pm8612991.
Simrén M, Vos R, Janssens J, Tack J. Unsuppressed postprandial phasic contractility in the proximal stomach in functional dyspepsia: relevance to symptoms. Am J Gastroenterol. 2003;98:2169–2175.
Tack J, Caenepeel P, Fischler B, Piessevaux H, Janssens J. Symptoms associated with hypersensitivity to gastric distention in functional dyspepsia. Gastroenterology. 2001;121:526–535. doi:10.1053/gast.2001.27180.
Karamanolis G, Caenepeel P, Arts J, Tack J. Association of the predominant symptom with clinical characteristics and pathophysiological mechanisms in functional dyspepsia. Gastroenterology. 2006;130:296–303. doi:10.1053/j.gastro.2005.10.019.
Soykan I, Sivri B, Sarosiek I, Kiernan B, McCallum R. Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci. 1998;43:2398–2404. doi:10.1023/A:1026665728213.
Guo JP, Maurer AH, Fisher RS, Parkman HP. Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci. 2001;46:24–29. doi:10.1023/A:1005697422454.
Lartigue S, Bizais Y, Des Varannes SB, Murat A, Pouliquen B, Galmiche JP. Inter- and intrasubject variability of solid and liquid gastric emptying parameters. A scintigraphic study in healthy subjects and diabetic patients. Dig Dis Sci. 1994;39:109–115. doi:10.1007/BF02090069.
Thomforde GM, Camilleri M, Phillips SF, Forstrom LA. Evaluation of an inexpensive screening scintigraphic test of gastric emptying. J Nucl Med. 1995;36:93–96.
Samsom M, Vermeijden JR, Smout AJ, et al. Prevalence of delayed gastric emptying in diabetic patients and relationship to dyspeptic symptoms: a prospective study in unselected diabetic patients. Diabetes Care. 2003;26:3116–3122. doi:10.2337/diacare.26.11.3116.
Jones KL, Russo A, Stevens JE, Wishart JM, Berry MK, Horowitz M. Predictors of delayed gastric emptying in diabetes. Diabetes Care. 2001;24:1264–1269. doi:10.2337/diacare.24.7.1264.
Vittal H, Farrugia G, Gomez G, Pasricha P. Mechanisms of disease: the pathological basis of gastroparesis—a review of experimental and clinical studies. Nat Clin Pract Gastroenterol Hepatol. 2007;4:336–346. doi:10.1038/ncpgasthep0838.
Karamanolis G, Caenepeel P, Arts J, Tack J. Determinants of symptom pattern in idiopathic severely delayed gastric emptying: gastric emptying rate or proximal stomach dysfunction? Gut. 2007;56:29–36. doi:10.1136/gut.2005.089508.
Bityutskiy L, Soykan I, McCallum R. Viral gastroparesis: a subgroup of idiopathic gastroparesis—clinical characteristics and long-term outcomes. Am J Gastroenterol. 1997;92:1501–1504.
Agrawal A, Houghton L, Lea R, Morris J, Reilly B, Whorwell P. Bloating and distention in irritable bowel syndrome: the role of visceral sensation. Gastroenterology. 2008;134:1882–1889. doi:10.1053/j.gastro.2008.02.096.
Azpiroz F, Malagelada J. The pathogenesis of bloating and visible distension in irritable bowel syndrome. Gastroenterol Clin North Am. 2005;34:257–269. doi:10.1016/j.gtc.2005.02.006.
Stanghellini V, Tosetti C, Paternicò A, et al. Predominant symptoms identify different subgroups in functional dyspepsia. Am J Gastroenterol. 1999;94:2080–2085. doi:10.1111/j.1572-0241.1999.01281.x.
Arts J, Caenepeel P, Verbeke K, Tack J. Influence of erythromycin on gastric emptying and meal related symptoms in functional dyspepsia with delayed gastric emptying. Gut. 2005;54:455–460. doi:10.1136/gut.2003.035279.
Acknowledgments
Dr. Pasricha is partly supported by NIDDK grant U01 DK073983 (PJ Pasricha, PI).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anaparthy, R., Pehlivanov, N., Grady, J. et al. Gastroparesis and Gastroparesis-like Syndrome: Response to Therapy and Its Predictors. Dig Dis Sci 54, 1003–1010 (2009). https://doi.org/10.1007/s10620-009-0717-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0717-4