Abstract
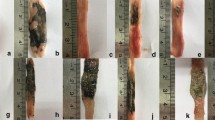
The effect of morphine on intestinal ulcer formation and on the degradation of the host defense barrier was studied. Mice receiving morphine (MRM) showed mucosal ulcer formation in the ileum and in the upper third of the colon. In in vitro studies, morphine enhanced apoptosis of cultured human colonic cells (HCC). Nitric oxide synthase (NOS) inhibitors attenuated the proapoptotic effect of morphine. Moreover, morphine stimulated NO generation by HCCs. MRM also showed a breach in the host defense barrier as well as injury to peritoneal macrophages. Although NOS inhibitors completely prevented morphine-induced intestinal ulcer formation, it provided only partial protection against a breach in the host defense barrier and peritoneal macrophage injury. Propranolol did not inhibit the induction of intestinal ulcer formation in MRM; nevertheless, propranolol prevented a breach in the host defense barrier as well as macrophage injury in MRM, whereas hemin exacerbated macrophage injury as well as the breach in the host defense barrier of MRM. These findings suggest that morphine-induced intestinal injury is mediated through NO generation. However, the degradation of the host defense barrier correlates with macrophage injury, but not intestinal injury.
Similar content being viewed by others
References
Bhaskaran M, Reddy K, Sharma S, et al..: Morphine-induced degradation of the host defense barrier: role of macrophage injury. J Infect Dis 184:1524–1531, 2001
Hilburger ME, Adler MW, Truant AL, et al.: Morphine induces sepsis in mice. J Infect Dis 176:183–187, 1997
Roy S, Cain KJ, Charboneau RG, Barke RA: Morphine accelerates the progression of sepsis in an experimental sepsis model. Adv Exp Med Biol 437:21–31, 1998
Roy S, Charboneau RG, Barke RA: Morphine synergizes with lipopolysaccharide in a chronic endotoxemia model. J Neuroimmunol 95:107–114, 1999
Berg RD: Bacterial translocation from gastrointestinal tract. Adv Exp Med Biol 473:11–30, 1999
Alexander JW, Boyce ST, Babcock GF, et al.: The process of microbial translocation. Ann Surg 212:496–512, 1990
Conn HO: Bacterial translocation: studies of mice and men. Am J Gastroenterol 93:277–278, 1998
Valle L, Pol O, Puig MM: Intestinal inflammation enhances the inhibitory effects of opioids of intestinal permeability in mice. J Pharmacol Exp Ther 296:378–387, 2001
Boughton-Smith NK, Evans SM, Hawkey CJ, et al.: Nitric oxide synthase activity in ulcerative colitis and Crohn's disease. Lancet 342:338–346, 1993
Boughton-Smith NK, Evans SM, Whittle BJR: Elevated nitric oxide synthase activity in inflamed colon from a rat model of colitis. Gut 33(Suppl 2):S12, 1992
Miller MJS, Sadowska-Krowieka A, Chotinaruemol S, Kakkis JL, Clark DA: Amelioration chronic ileitis by nitric oxide synthase inhibition. J Pharmacol Exp Ther 264:11–16, 1993
Parasher G, Frenklakh L, Goodman DR, Siddiqui T, Nandi J, Levine RA: Nitric oxide inhibitors ameliorate indomethacin-induced enteropathy in rats. Dig Dis Sci 46:2536–2541, 2001
Singhal PC, Kapasi AA, Franki N, Reddy K: Morphine-induced macrophage apoptosis: the role of transforming growth factor-beta. Immunology 100:57–62, 2000
Singhal PC, Bhaskaran M, Patel J, et al.: Role of P38 Mitogen-activated protein kinase phosphorylation and Fas-FasL interaction in morphine-induced macrophage apoptosis. J Immunol 168:4025–4033, 200
Singhal PC, Sharma P, Kapasi AA, Reddy K, Franki N, Gibbons N: Morphine enhances macrophage apoptosis. J Immunol 160:1886–1893, 1998
Herrmann H, Lorenz HM, Voll R, Grunke M, Woith W, Kalden JR: A rapid and simple method for the isolation of apoptotic DNA fragments. Nucleic Acids Res 22:5506–5507, 1994
Beckman JS: Oxidative damage and tyrosine nitration from peroxynitrite. Chem Res Toxicol 9:836–844, 1996
Pryor W, Squadrito G: The chemistry of peroxynitrite: a product from the reaction of nitric oxide with superoxide. Am J Physiol 268:L699–L722, 1995
Patel K, Bhaskaran M, Dani D, Reddy K, Singhal PC: Role of heme oxygenase (HO)-1 in morphine-modulated apoptosis and migration of macrophages. J Infect Dis 187:47–54, 2003
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frenklakh, L., Bhat, R.S., Bhaskaran, M. et al. Morphine-Induced Degradation of the Host Defense Barrier. Dig Dis Sci 51, 318–325 (2006). https://doi.org/10.1007/s10620-006-3132-0
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10620-006-3132-0