Abstract
Prenatal maternal stress is linked to offspring outcomes; however, there is little research on adolescents, behavioral, transdiagnostic outcomes, or the mechanisms through which relations operate. We examined, in N = 268 adolescents (Mage = 15.31 years; SD = 1.063; 57.8% boys) whether prenatal maternal stress is associated with adolescent affective outcomes; whether this association is mediated, serially, by childhood home atmosphere and adolescent behavioral inhibition system (BIS) sensitivity; and whether mediational effects are moderated by adolescent attention-deficit/hyperactivity disorder or maternal internalizing symptomology. Prenatal maternal daily stress and major life events were associated with adolescent outcomes through childhood negative atmosphere/neglect and BIS sensitivity, with no evidence of moderation. Results have implications regarding the effect of prenatal maternal stress on offspring outcomes and regarding corresponding sensitive periods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Across the globe, the prevalence of pediatric mental health disorders and problems has been increasing [1] and currently, up to 20% of adolescents experience a mental health disorder, with the third leading cause of death among adolescents (ages 15–19 years) being suicide [2]. The personal and societal burden of mental disorders are great; 7% of all burden of disease as measured in disability adjusted life years (DALYs) and 19% of all years-lived-with-disability are due to such disorders [3]. Of note, 50% of mental health disorders develop by the age of 14 years and for 75% of mental disorders, age-of-onset is before 24 years [4]. Accordingly, international policy guidelines underscore the importance of early identification and prevention of precursors or signs of psychopathology. Early intervention is cost-effective, can improve adult economic productivity [5] and adult health [6], as well as lessen the risk of adult psychopathology [7].
A sensitive and relevant developmental period in this regard is the prenatal period; as a result of the brain’s plasticity and sensitivity to environmental influences, prenatal maternal experiences can affect offspring development and functioning [8]. For example, prenatal maternal pharmacological treatment, maternal exposure to various chemical and non-chemical stressors (e.g., NO2, opioids), maternal preconception and prenatal nutrition are each associated with childhood cognitive outcomes [9], externalizing behaviors [10], developmental disorders [11] and neurodevelopment [12], and motor development [13]. Another aspect of the prenatal period, maternal exposure to stress, has also been linked to offspring outcomes. In animals, a large body of research indicates prenatal maternal stress affects offspring brain development, across preclinical [14,15,16] and non-human primate studies [17, 18]. Specifically, in utero stress exposure affects amygdala, corpus callosum, frontal cortex, hippocampus, and rostral anterior cingulate cortex development [19] and, in accordance with the functional neuroanatomy of these regions, results in attention deficits and behaviors linked to anxiety and depression (e.g., learned helplessness and alterations in circadian rhythm) [19]. Notably, in animals, prenatal stress effects endure throughout the lifespan [20]. In humans, although there are considerable differences across studies in methodology, e.g., with regard to the operationalization of stressFootnote 1 and also in terms of the exact findings, the literature is consistent in indicating that prenatal maternal stress is associated with increased risk for offspring behavioral, cognitive, and mental health problems [21]. Difficulties include cognitive deficits, a difficult temperament (low effortful control, high negative affectivity, and atypical reward sensitivity) and psychiatric disorders [21,22,23].
Regarding pathways, although the precise mechanisms via which gestational stress is associated with neurodevelopment and increases risk for offspring behavioral and cognitive problems have yet to be elucidated [19], prenatal maternal stress (and its proxies, such as anxiety and depression) impact development of the amygdala, limbic system, frontal lobes [24,25,26,27] and, via fetal exposure to elevated cortisol, brain systems related to stress processing and regulation, i.e., the hypothalamus [22] and hypothalamic-pituitary (HPA) axis [28] as well as the septohippocampal system [29].
The HPA axis is a neuroendocrine axis comprised of a brain system (the hypothalamus), the non-neural part of the pituitary (adenohypophysis) and the adrenal cortex. These interact with each other via a complex set of direct influences and feedback interactions to regulate bodily reactions to stress. The hypothalamus releases corticotrophin-releasing factor (CRF), thereby affecting the pituitary gland, which, in response releases adrenocorticotropic hormone (ACTH), which causes the adrenal cortex to release glucocorticoids, e.g., cortisol. Cortisol, in turn, affects HPA axis regulation [30]. Prenatal maternal stress, via hypoactivity of a placental enzyme 11-beta hydroxysteroid dehydrogenase-2 (11ß-HSD2) responsible for regulating the amount of cortisol passing through the placenta, may result in elevated fetal exposure to cortisol [31,32,33] and this may affect fetal HPA-axis development and results in offspring HPA-axis hyperresponsiveness [34]. The septohippocampal system comprises the hippocampus and the septum [35] and is implicated in the resolution of goal conflict [36]. Specifically, the septohippocampal system, and its monoaminergic brainstem afferents are implicated in sensitivity of the behavioral inhibition system (BIS) [36, 37].
The BIS is part of a larger architecture of attention- and motivation-regulating systems involving the behavioral activation system (BAS), the BIS, and the fight/flight/freeze system (FFFS) [38]. The functioning of this architecture of systems rests on functional distinctions between behaviors; e.g., behaviors that remove an organism from a source of danger (e.g., flight, fight, or freezing), a function governed by the FFFS, are different from those that allow it to assess a potential source of danger so as to determine an appropriate response, a function governed by the BIS [29]. As such, the BIS is a conflict detecting, monitoring, and resolving system that functions as a comparator of inputs to determine course of action [29, 36, 37]. Accordingly, although termed the ‘behavioral inhibition system’, the BIS both inhibits pre-potent behavior and generates additional outputs of attention and arousal to support exploratory behavior designed to resolve conflict [29]. Therefore, a function of the BIS is making assessments in situations involving approach-avoidance, approach-approach, and avoidance-avoidance conflicts [29, 36, 37]. The BIS is not only associated with anxiety and stress but its sensitivity is positively associated with ‘neuroticism’, or variously termed negative affectivity (NA) [39], i.e., the stable tendency to experience negative emotions [40].
Taken together, evidence indicates maternal prenatal stress is associated with offspring outcomes, and it stands to reason that the former exerts its effects on the latter including via its impact on the offspring stress systems, such as the septohippocampal system and its bio-behavioral correlate, the BIS. However, gaps in knowledge remain.
First, focus with regard to offspring outcomes has mostly been on infants and young children, without consideration of long-term effects observable in adolescence. Adolescence is a sensitive period from the perspective of brain development, as during this developmental period, enhanced neuroplasticity and structural and functional changes confer both advantages (e.g., skill learning facility) [41] and vulnerabilities (e.g., psychopathology risk) [41, 42]. Adolescent events of neuromaturation indicate this developmental phase may be a relatively sensitive window into the effects of earlier influences on neurodevelopment; adolescent developmental processes may reveal differences that were masked previously [43]. Better understanding the relation between prenatal maternal stress and adolescent offspring outcomes may be particularly relevant in this regard, as a host of mental health difficulties emerge in adolescence [44]. Early life adversity may set forth a “cascade” of molecular, cellular and/ or network-level effects in the developing brain [19, 45, 46], yet these may not manifest until later [47,48,49], such as in adolescence. In studies where adolescent or adult outcomes of prenatal maternal stress were examined, associations and differences on both a neural and a behavioral level were observed. On a neural level, prenatal maternal stress has been linked to adolescent offspring lower overall grey matter volume, especially in cortical regions associated with depression [50], adolescent offspring enhanced event-related potentials during endogenous cognitive control [51], and young adult offspring enhanced functional brain connectivity (which, in turn, correlated with depressive symptoms) [52]. On a behavioral level, prenatal maternal stress has been related to both higher externalizing [53, 54] and internalizing [53, 55,56,57] symptoms, ADHD and impulsivity [58,59,60] and differences in endogenous/exogenous control [51, 61].
Second, although there has been focus on offspring externalizing and internalizing disorders, there is a relative paucity of studies focused on transdiagnostic characteristics (but see the studies by [50] indicating prenatal maternal stress was associated with adult offspring affect dysregulation; by [51, 61, 62] and [63] indicating prenatal maternal stress was associated with differences in neuropsychological outcomes including inhibition and working memory). Transdiagnostic characteristics would be key to study in relation to prenatal maternal stress, as they are applicable, beyond clinical samples, to the general population and might result in adverse outcomes for youth, even in the absence of a diagnosable psychopathology [22].
Third, there are examinations of biological moderators (e.g., 5-HTTLPR [64] and mediators (e.g., DNA methylation [65,66,67], glucocorticoids [68]) of the link between prenatal maternal stress and offspring biological outcomes (i.e., offspring BMI and central adiposity [66], c-peptide secretion [67], cytokine production [65]). However, when it comes to individual differences in bio-behavioral and affective functioning, the majority of the literature is focused on bivariate associations, without consideration of boundary conditions (moderators; for whom or when effects operate) and mechanisms (mediators; how effects operate) of the relation between prenatal maternal stress and offspring outcomes [69]. Exceptions are a handful of studies assessing moderation, with mixed results. Across these studies, moderators tested were brain-derived neurotrophic factor (BDNF) genotype [57], COMT genotype [60], serotonin transporter polymorphism 5-HTTLPR [64] and maternal stress [70]. Outcomes of interest were offspring ADHD symptoms/working memory [60], behavioral disturbance [64], and internalizing symptoms [57, 70]. Across studies, the predictor was prenatal maternal anxiety [70]. Further exceptions are a comparably small number of investigations of mediation. Mediators tested were offspring childhood maltreatment [71, 72], executive functioning [73], HPA axis regulation [74], and temperamental negativity [75], as well as maternal general anxiety and mindful parenting [69]. Outcomes were offspring emotion regulation at three and 6 months of age [75]; internalizing problems in childhood [69]; academic achievement [73], antisocial behavior [72], and depression [74] in adolescence; and depression in adulthood [71]. Across studies, the predictor was prenatal maternal anxiety and/or depression [72].
To begin filling gaps in knowledge about adolescent affective outcomes of prenatal maternal stress, including more minor stress (and not only at more severe levels, as in anxiety and depression), with consideration of bio-behavioral mechanisms, our aim in the current study was to examine the relations between prenatal maternal stress, indices of adolescent emotion processing, specifically, affectivity, aggression, and emotion regulation, and how individual differences in adolescent BIS sensitivity affect these relations.
Beyond BIS sensitivity however, a conceptually and empirically relevant variable that prenatal maternal stress is related to and that might mediate or modulate the effects of such stress is the postnatal/early childhood home environment. Data show, for example, a positive association between prenatal stress and postnatal hostile-reactive parenting (Hentges et al. 2019) and that compared to non-exposed offspring, adult offspring exposed to prenatal maternal depression are over twice as likely to have experienced child maltreatment (Plant et al. [71]).
The negative effects of prenatal maternal stress through the postnatal home environment may operate through a diathesis-stress effect where negative outcomes result from an interaction between a predispositional vulnerability, i.e., the diathesis (e.g., prenatal maternal stress), and stress caused by life experiences (e.g., negative postnatal home environment) [76,77,78].
An alternative is that prenatal maternal stress may not only function as a diathesis but also as a source of developmental plasticity [78]. The differential susceptibility hypothesis extends the diathesis-stress model in positing that not only are certain individuals more vulnerable to the “risk” effects of negative environments but that certain individuals are (also) more vulnerable to the “protective effects” of positive environments, i.e., they are developmentally plastic [79]. Experimental findings with animals and observational data with humans support this hypothesis [71, 78, 80,81,82,83]. In humans, data show negative affectivity and physiological reactivity are well documented consequences of prenatal maternal stress. Individuals high on negative affectivity and physiological reactivity, when in aversive rearing environments, exert greatest deficits and difficulties across a variety of behavioral and psychological phenotypes but when in a supporting environment, exert greatest benefits on such measures (with individuals lower on negative affectivity falling in-between these extremes) [78].
In addition to findings indicating an association between prenatal maternal stress and postnatal home environment, results also suggest childhood maltreatment may affect child reinforcement sensitivity and emotion regulation; results show that young adults who were chronically mistreated as children exhibit greater threat sensitivity than their nonchronically mistreated or non-mistreated counterparts (Thompson et al. 84). Also, adults with a history of childhood interpersonal trauma exhibit higher punishment and lower reward sensitivity as well as greater BIS sensitivity (Miu et al. [85]). Accordingly, it stands to reason that prenatal maternal stress exerts its influence on adolescent outcomes through the early childhood environment which, in turn, alters the child’s reinforcement, i.e., BIS sensitivity, which, in turn is what results in negative outcomes.
Current Study
Our aims in the current study were to examine, for the first time, in a large sample of middle-late adolescents, whether (1) prenatal maternal stress—using measures of both more minor, daily stressors and of more major, life events stressors—is associated with indices of emotion processing, specifically, affectivity, aggression, and emotion regulation and (2) these associations are mediated, serially, by differences in the postnatal home environment and by reinforcement sensitivity, indexed by behavioral inhibition system (BIS) sensitivity. (3) Furthermore, given that parental psychopathology may affect the examined relations, insofar as it may affect the postnatal home environment, e.g., in the form of parenting style [86], and as it is a proxy for genetic predisposition to offspring psychopathology [87], our goal was to examine whether any of the mediational effects are moderated by maternal internalizing problems.
Method
Procedures
Data were collected in the context of a larger longitudinal project, the (BLINDED) study, aimed at identifying behavioral and biological protective and risk factors of behavior problems and functional impairments in adolescents exhibiting a range of attention-deficit/hyperactivity disorder (ADHD) symptoms but oversampled for ADHD. Data were obtained during the second year (baseline assessments) in the current study.
Adolescents between the ages of 14 and 17 years were recruited mainly from public middle-, technical and vocational-, and high schools as well as two child and adolescent psychiatry clinics in Budapest, Hungary. In case of schools, research staff visited classrooms and presented on the opportunity to participate in a research program. In case of clinics, research staff distributed an e-mail and fliers with information on the research program. Exclusionary criteria were cognitive ability at or below the percentile rank corresponding to an FSIQ of 80 across administered indices; autism spectrum disorder (severity ≥ 2); neurological illness; and having visual impairment as defined by impaired vision < 50 cm, unless corrected by glasses or contact lenses.
Parents and participants (i.e., adolescents) provided written informed consent (and assent). Adolescents underwent a series of tests, including assessment of cognitive ability and a structured clinical interview, followed by buccal swab and passive drool genetic sampling, and completion of questionnaires across two sessions. Self-report questionnaires completed by adolescents (detailed below) were assessments of affectivity, emotion dysregulation, reinforcement sensitivity, aggression and of the early childhood home environment. Questionnaires completed by parents involved parent-report measures of adolescent behavior and functioning (including ADHD) and parental self-report measures of prenatal maternal stress and parental psychopathology. All questionnaires were completed digitally, on a computer or tablet, using the Psytoolkit platform [88, 89] and the Qualtrics software, Version June 2020–March 2021 (Qualtrics, Provo, UT). This research was approved by the National Institute of Pharmacy and Nutrition (OGYÉI/17089-8/2019) and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
All (but ADHD and externalizing) diagnoses were determined using a combination of the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI Kid) [90] and the Structured Clinical Interview for DSM-5 Disorders, Clinical Version (SCID-5 CV) [91]. ADHD diagnoses were determined using parent-report on the ADHD Rating Scale-5 (ARS-5) [92]. For an ADHD diagnosis, adolescents had to meet a total of five (in case of youth < 17 years old) or six (in case of youth ≥ 17 years old) (or more) of the Diagnostic and Statistical Manual of Mental Disorders (5th ed; DSM-5) [93] inattention or hyperactivity/impulsivity symptoms and exhibit impairment (i.e., rating of 2 = moderate impairment or 3 = severe impairment) in at least three areas of functioning (G. DuPaul, personal communication, July 19, 2021). Unanimous agreement by two licensed child psychiatrists was required for ADHD diagnoses.
Participants
Participants included in the current study were 268 adolescents between the ages of 14 and 18 years (Mage = 15.31 years; SD = 1.063; 57.8% boys), n = 66 met criteria for ADHD. The majority (96.3%) identified as White and 3.7% identified as part of an ethnic minority group in Hungary. Average cognitive ability was in the 61.79th percentile (SD = 20.86), with estimated VCI percentile rank: M = 66.42, SD = 22.98, estimated PRI percentile rank M = 57.16, SD = 26.33. Participants were from an above-average socioeconomic background based on parental income (average family net income fell in the 5 001–700 000 HUF/month range, with average net income in Hungary being 289 000 HUF/month) [94].
Measures
For detailed description of measures, see Supplement. Cognitive functioning was estimated using abbreviated versions of the Wechsler Intelligence Scales [95, 96]. Minor prenatal stress was measured using the perceived stress scale (PSS) [97] and major prenatal stress using the prenatal life event scale (PLES) [98]. Affectivity, aggression, and emotion regulation were assessed via the positive and negative affect schedule (PANAS) [99], the difficulties in emotion regulation scale (DERS) [100] and the Buss-Perry aggression questionnaire (BPAQ) [101], respectively. The postnatal home environment was measured with the Neglect/Negative Home Atmosphere subscale of the child abuse and trauma scale (CATS) [102]. BIS sensitivity was measured with the BIS subscale of the Reinforcement Sensitivity Theory of Personality Questionnaire (RST-PQ) [103]. Maternal internalizing problems were assessed on the Internalizing Problems subscale of the Adult Self-Report 18–59 [104]. Adolescent ADHD status was determined using the home version of the ADHD rating scale-5 (ARS 5) [92].
Analytic Plan
We collected questionnaire data digitally, which requested a response for all questions. Due to sensitive issues, however, items from the CATS questionnaire were not mandatory, thus data on some items were missing for some participants; of the 38 CATS items 24 had missing data from ≥ one participant. Of the 268 adolescents, 242 responded to all CATS questions and 9 had missing data on ≥ one (typically, one to four) item, with a total of 88 missing CATS data points. Multiple imputation was used to substitute missing data; consistent with this method, five alternative iterations were created for possible responses to missing data points and the mean of these five iterations were used for imputation.
To examine the association among study variables, bivariate correlations were computed. To examine whether associations between prenatal maternal stress (as indexed by maternal report on the PLES and PSS) and adolescent offspring outcomes of interest (i.e., self-report affectivity, ED, and aggression) are mediated by childhood maltreatment variables (as indexed by CATS subscales) and BIS sensitivity as serial mediators, we used PROCESS Version 3.5 [105] to calculate 95% CIs around the indirect effect with 5000 bootstrap resamples,Footnote 2 implementing a heteroscedasticity-consistent standard error estimator. For all mediation findings, we report the completely standardized indirect effect(s).
Bivariate correlations were repeated with the subsample where the mother completed the Adult Self-Report (as interest was in maternal internalizing symptoms; n = 244). In addition to maternal internalizing psychopathology, as (1) our sample was oversampled for ADHD and (2) there are sex differences in the effects of prenatal stress [106], and sex differences in the incidence and prevalence of mental disorders begin to emerge during adolescence [107, 108], we also examined whether adolescent ADHD status and sex moderate the mediational effect of CATS neglect/negative atmosphere and BIS sensitivity. To this end, we conducted follow-up moderated mediational analyses in case of models that were supported in the serial mediational analyses. Adult Self-Report Internalizing Problems T Score, adolescent ADHD diagnosis, and adolescent sex were examined as moderators of the indirect path (from prenatal maternal stress to adolescent outcomes through CATS neglect/negative atmosphere and BIS sensitivity) and the direct path (from prenatal maternal stress to adolescent outcomes) in the mediational model, also using PROCESS Version 3.5 [105] and 5000 bootstrap resamples, implementing a heteroscedasticity-consistent standard error estimator.
For all mediation findings, we report the completely standardized indirect effect(s). Indirect effect 1 corresponds to the effect of the prenatal maternal stress variable(s) on the outcome through childhood maltreatment variable(s), Indirect effect 2 corresponds to the effect of the prenatal maternal stress variable(s) on the outcome through BIS sensitivity, and Indirect effect 3 corresponds to the serial mediation effect, i.e., the effect of the prenatal maternal stress variable(s) on the outcome through childhood maltreatment variable(s) and BIS sensitivity operating serially.
Results
Descriptive Analyses
Regarding prenatal maternal substance use, 19 (7.09%) mothers reported any kind of substance use while pregnant; 70 (26.12%) mothers reported their child was not born to term (i.e., was more than a week either pre-term or late term), 81 (30.22%) reported they experienced some form of complication during or after giving birth, 70 (26.12%) reported they had a high risk pregnancy, 18 (6.72%) reported they had an inflammatory disease while pregnant, and 16 (5.97%) reported their child was born with a lower than average birth weight (see Supplementary Table S1).
On the PLES, items most frequently endorsed and rated as at least “moderately negative or undesirable” were: “13. Did you have serious arguments several times with someone?” (n = 44 [16.30%]); “9. Did you have unusual financial pressures or trouble with money?” (n = 32 (11.80%)); “24. During your pregnancy, did you or a close family member or friend experience serious physical injury, illness, or hospitalization?” (n = 27 (10%)); “8. Did you have unusually big pressures or conflicts at work?” (n = 22 (8.20%)); (see Supplementary Table S2).
On the PSS, items most frequently endorsed as at least ‘fairly often’ (or ‘sometimes’ in case of reverse-scored items) were: “12. found yourself thinking about things that you have to accomplish?” (n = 105 (38.90%)); “1. been upset because of something that happened unexpectedly?” (n = 47 (17.40%)); “3. felt nervous and “stressed”?” (n = 41 (15.20%)); “8. found that you could not cope with all the things that you had to do?” (n = 40 (14.90%)); “11. been angered because of things that were outside of your control?” (n = 40 (14.80%)); (see Supplementary Table S2).
Bivariate Correlation Analyses
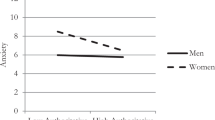
The prenatal maternal stress variables were positively correlated, with the correlation coefficient corresponding to a medium effect (Table 1). Greater PLES scores were associated with greater CATS neglect/negative atmosphere and BIS sensitivity—all small effects; PSS scores were associated with these variables as well as positively associated with greater ED and NA—also a small effect (Table 1). The two hypothesized mediators, CATS neglect/negative atmosphere and BIS sensitivity were positively correlated with each other, with the correlation coefficient corresponding to a medium effect, and both were positively correlated with all hypothesized outcomes (i.e., NA, ED, and aggression—CATS neglect/negative atmosphere and outcomes: medium to large effects and BIS sensitivity and outcomes: also medium (aggression) to large (NA, ED) effects) indicating the proposed mediator-outcome combinations are suitable for mediation analysis [109] (Table 1). NA, ED, and aggression were also positively related—all medium to large effects (Table 1). Girls reported greater CATS neglect/negative atmosphere, ED, NA and greater BIS sensitivity and older age was associated with greater ED, NA and BIS sensitivity (small effects).
When repeating bivariate correlations restricted to the portion of the sample whose mothers completed the Adult Self-Report (as interest was in maternal internalizing symptoms; n = 244), the pattern of correlations among hypothesized predictor, mediator, outcome, sex, and age variables was the same as in the overall sample (Table 2). Maternal internalizing symptoms were positively associated with PLES (r = 0.229, p < 0.001) and PSS (r = 0.475, p < 0.001) scores (a small and a medium effect, respectively) and also with adolescent offspring BIS sensitivity (r = 0.236, p < 0.001) and NA (r = 0.256, p < 0.001) (medium effects) and ED (r = 0.253 p < 0.001) (a borderline medium effect) and CATS neglect/negative atmosphere (r = 0.168 p = 0.009) (Table 2).
Mediation Analyses with the PLES as the Predictor
Negative Affectivity as the Outcome
CATS neglect/negative atmosphere (NNA) and BIS sensitivity mediated the association between PLES and NA (effect = 0.042; SE = 0.018; 95%CIs (0.011; 0.080)). Greater PLES was associated with greater CATS neglect/negative atmosphere and higher scores on CATS neglect/negative atmosphere were associated with greater BIS sensitivity which, in turn, was positively associated with NA. CATS neglect/negative atmosphere was also positively associated with NA but the association between PLES and NA was not significant. Jointly, PLES, CATS NAA, and BIS sensitivity accounted for 52% of the variance in NA (Table 3). Indirect effect 1 was (effect = 0.096; SE = 0.042; 95%CIs (0.017; 0.180)), but Indirect effect 2 was not (effect = 0.029; SE = 0.014; 95%CIs (0.007; 0.062)) supported.
Emotion Dysregulation as the Outcome
CATS neglect/negative atmosphere and BIS sensitivity mediated the association between PLES and DERS (effect = 0.043; SE = 0.017; 95%CIs (0.012; 0.079)). Greater PLES was associated with greater CATS neglect/negative atmosphere and higher scores on CATS neglect/negative atmosphere was associated with greater BIS sensitivity which, in turn, was positively associated with greater ED. CATS neglect/negative atmosphere was also associated with greater ED but the associations between PLES and BIS and PLES and ED were not significant. Jointly, PLES, CATS neglect/negative atmosphere, and BIS sensitivity accounted for 52% of the variance in ED (Table 3). Indirect effect 1 was (effect = 0.028; SE = 0.014; 95%CIs (0.006; 0.060)), but Indirect effect 2 was not (effect = 0.025; SE = 0.033; 95%CIs (− 0.038; 0.095)) supported.
Aggression as the Outcome
CATS neglect/negative atmosphere and BIS sensitivity mediated the association between PLES and aggression (effect = 0.017; SE = 0.010; 95%CIs (0.002; 0.042)). Greater PLES was associated with greater CATS neglect/negative atmosphere and higher scores on CATS neglect/negative atmosphere was associated with greater BIS sensitivity which, in turn, was positively associated with aggression. CATS neglect/negative atmosphere was also positively associated with aggression but the associations between PLES and BIS and PLES and aggression were not significant. Jointly, PLES, CATS neglect/negative atmosphere, and BIS sensitivity accounted for 17% of the variance in aggression (Table 3). Indirect effect 1 was (effect = 0.034; SE = 0.020; 95%CIs (0.004; 0.081)), but Indirect effect 2 was not (effect = 0.012; SE = 0.014; 95%CIs (− 0.016; 0.039)) supported.
Mediation Analyses with the PSS as the Predictor
Negative Affectivity as the Outcome
CATS neglect/negative atmosphere and BIS sensitivity mediated the association between PSS and NA (effect = 0.070; SE = 0.020; 95%CIs (0.031; 0.112)). Greater PSS was associated with greater CATS neglect/negative atmosphere and CATS neglect/negative atmosphere was positively associated with BIS sensitivity (the association between PSS and BIS sensitivity was not significant) which, in turn, was positively associated with NA (the association between PSS and NA was not significant but CATS neglect/negative atmosphere was positively associated with NA). Jointly, PSS, CATS neglect/negative atmosphere, and BIS sensitivity accounted for 52% of the variance in NA (Table 4). Indirect effect 1 was (effect = 0.049; SE = 0.020; 95%CIs (0.016; 0.091)) but Indirect effect 2 was not (effect = 0.024; SE = 0.032; 95%CIs (− 0.036; 0.088)) supported.
Emotion Dysregulation as the Outcome
CATS neglect/negative atmosphere and BIS sensitivity mediated the association between PSS and DERS (effect = 0.072; SE = 0.021; 95%CIs (0.034; 0.114)). Greater PLES was associated with greater CATS neglect/negative atmosphere and higher scores on both were associated with greater BIS sensitivity which, in turn, was positively associated with ED (the associations between PLES and ED and CATS neglect/negative atmosphere and ED were not significant). Jointly, PLES, CATS neglect/negative atmosphere, and BIS sensitivity accounted for 54% of the variance in ED (Table 4). Indirect effect was 1 (effect = 0.041; SE = 0.018; 95%CIs (0.010; 0.081)) but Indirect effect 2 was not (effect = 0.024; SE = 0.032; 95%CIs (−0.035; 0.089)) supported.
Aggression as the Outcome
CATS neglect/negative atmosphere and BIS sensitivity mediated the association between PSS and DERS (effect = 0.028; SE = 0.015; 95%CIs (0.006; 0.062)). Greater PSS was associated with greater CATS neglect/negative atmosphere and higher scores on CATS neglect/negative atmosphere were associated with greater BIS sensitivity (the association between PSS and BIS sensitivity was not significant) which, in turn, was positively associated with aggression. CATS neglect/negative atmosphere was also positively associated with aggression but the associations between PSS and aggression was not significant). Jointly, PSS, CATS neglect/negative atmosphere, and BIS sensitivity accounted for 17% of the variance in aggression (Table 4). Indirect effect 1 was (effect = 0.059; SE = 0.025; 95%CIs (0.016; 0.112)), but Indirect effect 2 was not (effect = 0.013; SE = 0.014; 95%CIs (− 0.013; 0.041)) supported.
For a visual summary of mediation results, see Fig. 1.
Visual summary of serial mediation results with childhood neglect/ negative atmosphere (NNA) and adolescent behavioral inhibition system (BIS) sensitivity operating in serial and mediating the association between prenatal maternal stress and adolescent affective outcomes, with A the prenatal life events scale (PLES) and B the perceived stress scale (PSS) as indices of prenatal stress. Solid lines indicate models with indirect effects supported (indirect effects 1 and 3, across models) and dashed lines indicate models with indirect effects not supported (indirect effect 2, across models). Coefficients are standardized regression weights. NA negative affectivity, ED emotion dysregulation, AGG aggression. ***p < 0.001; **p < 0.01; *p < 0.05; 0.1 > p < 0.05
Follow-up Moderated Mediation Analyses
Adolescent ADHD status did not moderate the direct or indirect effect (through CATS neglect/negative atmosphere) of PLES on BIS (index = − 1.205; SE = 0.702; 95%CIs (− 2.599; 0.153)), on NA (index = − 0.592; SE = 0.360; 95%CIs (− 1.326; 0.114)), on ED (index = 1.855; SE = 1.124; 95%CIs (− 4.134; 0.404)), or on aggression (index = 1.007; SE = 0.700; 95%CIs [− 2.256; 0.567)). Maternal internalizing symptoms also did not moderate the direct or indirect effect (through CATS neglect/negative atmosphere) of PSS on BIS (index = − 0.081; SE = 0.106; 95%CIs (−0.287; 0.130)) on NA (index = − 0.040; SE = 0.053; 95%CIs (−0.143; 0.071)), on ED (index = − 0.040; SE = 0.109; 95%CIs (−0.261; 0.177)), or on aggression (index = − 0.040; SE = 0.109; 95%CIs (− 0.261; 0.177)).
Maternal internalizing symptoms did not moderate the direct or indirect effect (through CATS neglect/negative atmosphere) of PLES on BIS (index = − 0.042; SE = 0.032; 95%CIs (− 0.112; 0.017)), on NA (index = − 0.021; SE = 0.017; 95%CIs (− 0.060; 0.008)), on ED (index = − 0.065; SE = 0.052; 95%CIs (− 0.182; 0.025)), or on aggression (index = − 0.025; SE = 0.041; 95%CIs (− 0.111; 0.052)). Maternal internalizing symptoms also did not moderate the direct or indirect effect (through CATS neglect/negative atmosphere) of PSS on BIS (index = − 0.006; SE = 0.004; 95%CIs (− 0.014; 0.001)) on NA (index = − 0.003; SE = 0.002; 95%CIs (− 0.007; 0.001)), on ED (index = − 0.009; SE = 0.006; 95%CIs (− 0.021; 0.002)), or on aggression (index = − 0.004; SE = 0.004; 95%CIs (− 0.014;0.004)).
Adolescent sex status did not moderate the direct or indirect effect (through CATS neglect/negative atmosphere (NNA)) of PLES on BIS (index = 0.677; SE = 0.653; 95%CIs (− 0.528; 2.018)), on NA (index = 0.373; SE = 0.369; 95%CIs (− 0.309; 1.146)), on ED (index = 1.150; SE = 1.159; 95%CIs (− 1.001;3.560)), or on aggression (index = 1.145; SE = 0.852; 95%CIs (− 0.317; 3.002)). Adolescent sex also did not moderate the direct or indirect effect (through CATS neglect/negative atmosphere (NNA)) of PSS on BIS (index = 0.068; SE = 0.085; 95%CIs (− 0.096; 0.242)), on NA (index = 0.037; SE = 0.047; 95%CIs (− 0.052; 0.136)), on ED (index = 0.109; SE = 0.138; 95%CIs (− 0.140; 0.400)), or on aggression (index = 0.101; SE = 0.100; 95%CIs (− 0.087; 0.295)).
Discussion
Our goals in this study were to assess, in middle-late adolescents, whether prenatal maternal stress—conceptualized and measured as both relatively minor, daily stressors and as relatively major, life events stressors—is associated with indices of affective processing, specifically, affectivity, aggression, and emotion dysregulation and whether these associations are mediated, serially, by differences in the childhood home environment and adolescent BIS sensitivity. We also examined whether adolescent ADHD diagnosis or maternal internalizing symptoms moderated any of the mediational effects.
This study is one of a handful of examinations of transdiagnostic outcomes of prenatal maternal stress, with findings applicable across the general and clinical populations. To the best of our knowledge, this was the first evaluation of a serial mediational effect and of the mediational effect of adolescent BIS sensitivity.
Findings of bivariate correlation analyses were generally as expected, with a positive association of PLES scores with BIS sensitivity [110] and with NA [110, 111]. These findings are not only consistent with earlier results, but extend those to the transdiagnostic characteristics of negative affectivity, aggression, and emotion dysregulation, in a relatively understudied developmental group, middle-late adolescents. Interestingly, there was a differential pattern, where prenatal maternal stress caused by major life events was associated with all measured adolescent outcomes but ED whereas prenatal maternal stress caused by minor daily stressors was not associated with any of the adolescent outcomes but ED. All of these relations corresponded to small effects, perhaps because several third variables influence such relations (including the ones assessed here) and/ or because prenatal maternal stress was mother-reported whereas adolescent outcomes were self-reported.
Also as expected, the hypothesized mediators, CATS neglect/negative atmosphere and BIS sensitivity were positively correlated with each other [85] and also with all assessed outcomes [40, 112,113,114,115,116]. These relations corresponded to medium to large effects, likely driven by their relative phenomenological and temporal proximity and/ or partly due to shared method variance. In line with what is known about age and sex differences, older age was associated with greater BIS sensitivity [117, 118] and girls reported greater BIS sensitivity. Others have previously found a curvilinear relation between age and aggression, where aggression increased until early-middle adolescence and declined by late adolescence [119, 120] and no sex-difference with regard to emotional neglect and abuse [121] whereas here, we wound older age was associated with greater aggression and girls reported greater CATS neglect/negative atmosphere. Perhaps most importantly, prenatal maternal stress caused by major life events was positively associated with prenatal maternal stress caused by minor daily stressors but with the correlation coefficient corresponded to a small effect, indicating that although the two variables are associated, they are not isomorphic (or redundant) and thus represent related but distinct phenomena.
When examined in greater complexity, i.e., in a serial mediation model, both indices of prenatal maternal stress were associated with adolescent affective outcomes, through the serial effects of differences in the early childhood home atmosphere/environment and in adolescent BIS sensitivity. Of import, the effect of prenatal stress on the herein assessed adolescent affective outcomes was only significant in the presence of a mediational effect of childhood neglect/ negative atmosphere and BIS sensitivity (i.e., full mediation). The mediational effect of childhood neglect/ negative atmosphere (indirect effect 1) was significant even in the absence of the subsequent mediational effect of BIS sensitivity. This is consistent with earlier findings indicating an association between prenatal maternal stress and subsequent difficulties with parenting [122] and child maltreatment [71]. Our finding further extends these prior results insofar as it suggests an effect of these variables on adolescent affective outcomes. The mediational effect of BIS sensitivity (indirect effect 2) was only significant in the presence of a preceding mediational effect of childhood neglect/ negative atmosphere. This set of results have both conceptual and clinical implications.
Regarding conceptual implications, first, these findings underscore the importance of examining the effect of mechanisms—when examined in the context of mediators, the direct path between prenatal maternal stress and outcomes was not significant, indicating the observed relation was fully mediated by the assessed mechanisms. This finding is consistent with contemporary thinking about the complexity of relations between variables indexing human development and psychology; that accounting for relevant mechanisms and influences may reveal small or otherwise undetected effects [123].
Second, as noted, although the mechanisms via which gestational stress is associated with neurodevelopment and increases risk for offspring behavioral problems have yet to be elucidated [19], a leading hypothesis is that prenatal maternal stress impacts, via fetal exposure to elevated cortisol, offspring brain systems related to stress processing and regulation, such as the septohippocampal system. Our results are consistent with this hypothesis insofar as they show that prenatal maternal stress is associated with adolescent offspring affective problems through greater BIS sensitivity, with the septohippocampal system, and its monoaminergic brainstem afferents hypothesized to be implicated in BIS sensitivity [124].
Regarding clinical implications, establishing that an early-emerging characteristic may be a protective or risk factor for later functional impairments, behavioral problems, or psychopathology enhances conceptualization of developmental trajectories to such outcomes. Arguably, however, the practical significance of such a characteristic and its role is closely linked to the degree to which it is a promising intervention—prevention or treatment—target and that is largely determined by the degree to which it is malleable [125]. It is against this backdrop that we discuss the relevance of the current set of results for prevention of adolescent affective problems such as negative affectivity, aggression, and ED and the sequalea of such problems, including diagnosable psychopathology [126,127,128]. In the context of the variables examined here, the first point of intervention would need to be during the prenatal period and focus on decreasing maternal stress. Such preventions and treatments are available and include cognitive-behavioral, interpersonal, and psychoeducational strategies, with data indicating short-term efficacy of cognitive and psychoeducational techniques for reducing prenatal maternal stress [129,130,131]. Early evidence shows Both mindfulness-based interventions and yoga may also effectively decrease prenatal maternal stress, but methodologically rigorous studies are needed to confirm observed effects [131,132,133,134]. Virtual reality, although also promising, is less available than these approaches and more research is needed to establish its efficacy [135]. In case of children for whom prenatal maternal stress had already occurred (e.g., who present to clinical care during early childhood or later), consistent with a differential susceptibility framework, an alternative point of intervention would be during childhood and focus on decreasing neglect/ negative atmosphere and improving the early childhood home atmosphere/environment (e.g., through parent training; [136]. In terms of scientific rigor, studies on parenting programs are heterogeneous, with some methodologically sound designs assessing efficacy of e.g., Group Family Nurse Partnership [137], REAL Fathers Initiative [138], and SOS Help for Parents [139]. In case of children for whom both the prenatal maternal stress and the negative childhood home atmosphere/environment had occurred (e.g., who present to clinical care during early adolescence or later), there is yet an alternative point and focus of intervention. In such cases, intervention would be indicated during adolescence and to aim at attenuating BIS sensitivity. Data show the BIS may be malleable as environmental (vs. genetic) effects contribute to changes in BIS sensitivity [140]. Although to our knowledge, no interventions explicitly target BIS sensitivity, certain interventions target and have been observed to alter reinforcement sensitivity (e.g., Cognitive Remediation Therapy targets punishment sensitivity and Transcranial Magnetic Stimulation targets reward sensitivity) [141, 142]. Other interventions do not target reinforcement sensitivity but have been shown to reduce BIS sensitivity (e.g., Behavioral Activation Therapy and certain mindfulness types) [143, 144]. Pharmacological treatments, e.g., anxiolytic drugs also reduce BIS sensitivity [36]. Of note, BIS sensitivity is not to be conflated with anxiety. There is certainly overlap between BIS hyperactivity and excessive anxiety, as BIS hyperactivity may result in excessive focus on environmental threat and, as an indirect consequence, on threatening associations with previous stimuli [36]. Nonclinical and clinically anxious individuals exhibit an automatic, preferential attention to threat (i.e., attentional bias) [145]. Despite this overlap, the response of the defense system of which the BIS is part is context- or state-dependent. In contrast, individuals with elevated levels of anxiety stably perceive the environment as dangerous; as such, elevated trait anxiety is associated with negative schema, hyper-vigilance to threatening information, and at the memory level, hyper-recall of threatening information [146].
Limitations and Future Directions
Prenatal maternal stress was assessed via retrospective report, which is associated with potential biases, including, but not limited to biases resulting from current psychological disorders or functioning. Three lines of evidence lend credence to the validity of assessing prenatal maternal stress via retrospective report.
First, although past 6 months maternal internalizing symptoms were positively associated with both measures of prenatal maternal stress (prenatal stress caused by major life events and prenatal stress caused by minor daily stressors) and these two measures of prenatal stress were also positively associated with each other, the magnitude of these relations were mostly small. This arguably indicates, on one hand, that current maternal internalizing symptoms did not to a confounding extent influence maternal report of prenatal stress. Further, that mothers differentiated between the two types of stressors suggests absence of a systematic bias.
Second, earlier data evince the accuracy of retrospective report of relevant characteristics and information, such as descriptions of the family environment 25 years ago validated against prospective measures of such environment (moderate correlations of 0.30–0.45 [147]; maternal report of breastfeeding history from 20 years ago validated against clinic charts (strong correlations of 0.86) [148]; maternal report about a range of pre and peri-natal factors (e.g., infant birth weight, infant admission to special care baby unit, method of delivery, smoking during pregnancy, high blood pressure/oedema during pregnancy) from four to nine years ago validated against antenatal records [149] and against maternal report 6 months postpartum [150]; or parental report of child birth information from 12 years ago validated against hospital records [151].
Third, we repeated our analyses conducted with the “mean prenatal life events distress score” using “the number of prenatal life events” as the PLES predictor and replicated our findings (see Supplement). This is meaningful as the former score comprises items assessing the extent to which one was negatively affected by events that occurred whereas the latter comprises items assessing whether or not such events occurred. Arguably, the former is considerably more subject to recall bias than the latter. Although these data lend credence to the herein obtained retrospective report of prenatal stress, a recall bias cannot be completely ruled out. As such, our data are best conceptualized as preliminary indication that the herein observed relations are worthy of examination in considerably more resource-consuming longitudinal, prospective designs.
Given poor internal consistency of the other CATS subscales, only one aspect of the early childhood home atmosphere/environment was examined in our research (i.e., neglect/negative atmosphere), future research may examine whether our findings generalize to other aspects of the childhood home environment, such as physical abuse and neglect or sexual abuse. Similarly, only one aspect of reinforcement sensitivity was tested in this study (i.e., BIS sensitivity). Evidence shows prenatal maternal nutrition and stress affect offspring mesocorticolimbic system [152], and such prenatal programming of offspring mesocorticolimbic system appears to play a role in the development of traits related to behavioral activation system (BAS) sensitivity, such as attention toward salient stimuli, reward sensitivity as well as extraversion, novelty seeking, and impulsivity [153]. Accordingly, future research may examine whether the herein obtained results generalize to other aspects of reinforcement sensitivity, such as BAS sensitivity.
Mediation can be demonstrated in cross-sectional research [154], but only via statistical criteria [123, 155,156,157,158]. Accordingly, we established atemporal mediation, mathematically/ statistically. As we tested but did not find support for reversed models—as recommended e.g., in cross-sectional designs, where temporal precedence is not definitively established [159,160,161,162,163], our findings evince unidirectionality of observed effects and indicate additional research is warranted, e.g., experimental or prospective studies to establish temporal mediation and thus causation [161, 164].
We examined relations across a set of a priori chosen variables, selected based on theory and prior empirical data. Certainly, the relations between prenatal maternal stress and adolescent outcomes is complex, with several additional variables also influencing such relations. Although we aimed to assess some of these variables, including maternal smoking or drug use during pregnancy, only a small number of mothers reported they smoked or used alcohol or drugs, indicating there may be need in the future to oversample mothers who engage in substance use. Examples of pertinent variables not assessed here include child genetic predisposition or life events, and parental emotion regulation or parenting style. In support, there is evidence that prenatal maternal stress may have greatest impact on areas of functioning in which the offspring has a genetic vulnerability; in one study, prenatal maternal anxiety was associated with adolescent offspring ADHD outcome at age 15 years only in children with a specific variation of the COMT gene [60].
In intending to assess the moderational effect of maternal internalizing symptomology, we assessed maternal anxiety and depressive symptoms as experienced during the past 6 months. Current and past 6 months internalizing symptoms may not be related to maternal internalizing symptomology during pregnancy or after, however, it is a good proxy for the likelihood of maternal anxiety or depression as well as for genetic predisposition to offspring psychopathology [87]. Nevertheless, to be able to make stronger claims about the moderational effect of maternal psychopathology, it will be important to collect data on this variable during and after pregnancy.
As noted, we found outcomes were differentially associated with prenatal maternal stress caused by major life events vs. daily stressors; the former was associated NA and aggression whereas the latter was only associated with ED. It would be premature to speculate on this pattern based on the current findings, but whether these differential effects replicate (and what might be driving them) may be conceptually relevant to explore in the future.
We defined adolescence based on chronological age without accounting for biological age or pubertal status, though these may not necessarily correspond. It thus remains an outstanding question whether these findings replicate if adolescence is defined based on biological maturity.
Finally, the current sample was a community-based sample, with the majority of youth White. It will be important to examine whether results generalize to clinical populations, ethnic minorities and other racial groups as well as to collect data on symptoms, beyond children and parents, from teachers. Related, as described in Methods, adolescents were oversampled for ADHD. As such, sampling was not random and findings may not correspond to what would be observed in a randomly selected group of adolescents. Although we assessed and did not find evidence for a moderational effect of ADHD status, there are associated features of ADHD (e.g., at the group level, differences in IQ or SES) that were not evaluated in this manner but may have a bearing on the results.
Summary
In this first study assessing the serial mediational effect of differences in the childhood home environment and adolescent behavioral inhibition system sensitivity on the association between prenatal maternal stress and adolescent affective outcomes, we found that the relation between prenatal maternal stress and adolescent affective outcomes is mediated by both childhood neglect/negative atmosphere and adolescent behavioral inhibition system sensitivity. These relations held across types of maternal stress, i.e., across stress caused by major, life events stressors and stress caused by minor, daily stressors and were not moderated by adolescent ADHD diagnosis or by current/recent maternal internalizing symptomology. On its own, neither childhood neglect/negative atmosphere nor adolescent behavioral inhibition system sensitivity exerted a mediational effect, indicating it is in the modeled and tested serial order that they account for the relation between prenatal maternal stress and adolescent negative affectivity, aggression, and ED. Prevention and intervention efforts aimed at reducing negative adolescent affective outcomes and the potential psychiatric sequelae of such outcomes are to be tailored, with regard to their focus and target, to the developmental phase during which the intervention occurs.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Notes
Mainly as maternal psychiatric symptoms, such as anxiety and depression, major life events, military invasion, natural disasters.
The macros provide a 95% CI around the indirect effect. When zero is not in the 95% CI, the indirect effect is different from zero at p < 0.05 (two tailed).
References
Baranne ML, Falissard B (2018) Global burden of mental disorders among children aged 5–14 years. Child Adolesc Psychiatry Ment Health 12(1):1–9. https://doi.org/10.1186/s13034-018-0225-4
UNICEF (United Nations International Children’s Emergency Fund) (2019) Increase in child and adolescent mental disorders spurs new push for action by UNICEF and WHO. UNICEF
Rehm J, Shield KD (2019) Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. https://doi.org/10.1007/s11920-019-0997-0
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 62(6):593–602
Heckman JJ (2006) Skill formation and the economics of investing in disadvantaged children. Science 312(5782):1900–1902. https://doi.org/10.1126/science.1128898
Campbell F et al (2014) Early childhood investments substantially boost adult health. Science 343(6178):1478–1485. https://doi.org/10.1126/science.1248429
Dodge KA et al (2015) Impact of early intervention on psychopathology, crime, and well-being at age 25. Am J Psychiatry 172(1):59–70. https://doi.org/10.1176/appi.ajp.2014.13060786
Dua T et al (2016) Global research priorities to accelerate early child development in the sustainable development era. Lancet Global Health. https://doi.org/10.1016/S2214-109X(16)30218-2
Nelson LF, Yocum VK, Patel KD, Qeadan F, Hsi A, Weitzen S (2020) Cognitive outcomes of young children after prenatal exposure to medications for opioid use disorder a systematic review and meta-analysis. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2020.1195
Nilsen FM, Frank J, Tulve NS (2020) Environmental protection agency, office of research and development. IJERPH. https://doi.org/10.3390/ijerph17072361
Li M, Francis E, Hinkle SN, Ajjarapu AS, Zhang C (2019) Preconception and prenatal nutrition and neurodevelopmental disorders: a systematic review and meta-analysis. Nutrients. https://doi.org/10.3390/nu11071628
Shang L et al (2019) Effects of prenatal exposure to NO 2 on children’s neurodevelopment: a systematic review and meta-analysis. Environ Sci Pollut Res. https://doi.org/10.1007/s11356-020-08832-y
Grove K, Lewis AJ, Galbally M (2018) Prenatal antidepressant exposure and child motor development: a meta-analysis. Pediatrics. https://doi.org/10.1542/peds.2018-0356
Hayashi A, Nagaoka M, Yamada K, Ichitani Y, Miake Y, Okado N (1998) Maternal stress induces synaptic loss and developmental disabilities of offspring. Int J Dev Neurosci. https://doi.org/10.1016/S0736-5748(98)00028-8
Lemaire V, Lamarque S, Le Moal M, Piazza PV, Abrous DN (2006) Postnatal stimulation of the pups counteracts prenatal stress-induced deficits in hippocampal neurogenesis. Biol Psychiat. https://doi.org/10.1016/j.biopsych.2005.11.009
Petit B et al (2015) Stress during pregnancy alters dendritic spine density and gene expression in the brain of new-born lambs. Behav Brain Res. https://doi.org/10.1016/j.bbr.2015.05.025
Coe CL, Lulbach GR, Schneider ML (2002) Prenatal disturbance alters the size of the corpus callosum in young monkeys. Dev Psychobiol. https://doi.org/10.1002/dev.10063
Coe CL et al (2003) Prenatal stress diminishes neurogenesis in the dentate gyrus of juvenile Rhesus monkeys. Biol Psychiat. https://doi.org/10.1016/S0006-3223(03)00698-X
McQuaid GA, Darcey VL, Avalos MF, Fishbein DH, VanMeter JW (2019) Altered cortical structure and psychiatric symptom risk in adolescents exposed to maternal stress in utero: a retrospective investigation. Behav Brain Res. https://doi.org/10.1016/j.bbr.2019.112145
Vallée M, Maccari S, Dellu F, Simon H, Le Moal M, Mayo W (1999) Long-term effects of prenatal stress and postnatal handling on age-related glucocorticoid secretion and cognitive performance: a longitudinal study in the rat. Eur J Neurosci 11:2906–2916
Van den Bergh BRH et al (2020) Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev 117:26–64. https://doi.org/10.1016/j.neubiorev.2017.07.003
Krzeczkowski JE, Van Lieshout RJ (2019) Prenatal influences on the development and stability of personality. New Ideas Psychol 53:22–31. https://doi.org/10.1016/j.newideapsych.2018.01.003
Beversdorf DQ et al (2005) Timing of prenatal stressors and autism. J Autism Dev Disord. https://doi.org/10.1007/s10803-005-5037-8
Buss C, Davis EP, Muftuler LT, Head K, Sandman CA (2010) High pregnancy anxiety during mid-gestation is associated with decreased gray matter density in 6–9-year-old children. Psychoneuroendocrinology 35(1):141–153. https://doi.org/10.1016/j.psyneuen.2009.07.010
Sandman CA, Buss C, Head K, Davis EP (2015) Fetal exposure to maternal depressive symptoms is associated with cortical thickness in late childhood. Biol Psychiat 77(4):324–334. https://doi.org/10.1016/j.biopsych.2014.06.025
Kraszpulski M, Dickerson PA, Salm AK (2006) Prenatal stress affects the developmental trajectory of the rat amygdala. Int J Biol Stress 9(2):85–95
Monk C, Lugo-Candelas C, Trumpff C (2019) Prenatal developmental origins of future psychopathology: mechanisms and pathways. Annu Rev Clin Psychol 15:317–344
Lautarescu A, Craig MC, Glover V (2020) Prenatal stress: effects on fetal and child brain development. Int Rev Neurobiol 150:17–40. https://doi.org/10.1016/bs.irn.2019.11.002
McNaughton N, Corr PJ (2004) A two-dimensional neuropsychology of defense: fear/anxiety and defensive distance. Neurosci Biobehav Rev 28(3):285–305. https://doi.org/10.1016/j.neubiorev.2004.03.005
Malenka RC, Nestler EJ, Hyman SE (2009) Neural and neuroendocrine control of the internal milieu. In: Nestler EJ, Hyman SE, Malenka RC (eds) Molecular neuropharmacology: a foundation for clinical neuroscience. McGraw-Hill, New York, pp 248–259
Lester BM, Marsit CJ, Conradt E, Bromer C, Padbury JF (2012) Behavioral epigenetics and the developmental origins of child mental health disorders. J Dev Orig Health Dis 3(6):395–408. https://doi.org/10.1017/S2040174412000426
O’Donnell KJ, Bugge Jensen A, Freeman L, Khalife N, O’Connor TG, Glover V (2012) Maternal prenatal anxiety and downregulation of placental 11β-HSD2. Psychoneuroendocrinology 37(6):818–826. https://doi.org/10.1016/j.psyneuen.2011.09.014
Bowers ME, Yehuda R (2016) Intergenerational transmission of stress in humans. Neuropsychopharmacology 41:232–244
Emack J, Matthews SG (2011) Effects of chronic maternal stress on hypothalamo-pituitary-adrenal (HPA) function and behavior: no reversal by environmental enrichment. Horm Behav 60(5):589–598. https://doi.org/10.1016/j.yhbeh.2011.08.008
Gray JA, Mcnaughton N (2000) Jeffrey A. Gray Neil McNaughton, p 443
McNaughton N, Gray JA (2000) Anxiolytic action on the behavioural inhibition system implies multiple types of arousal contribute to anxiety. J Affect Disord 61(3):161–176. https://doi.org/10.1016/S0165-0327(00)00344-X
Bunford N, Roberts J, Kennedy AEEAE, Klumpp H (2017) Neurofunctional correlates of behavioral inhibition system sensitivity during attentional control are modulated by perceptual load. Biol Psychol 127(10–17):10–17. https://doi.org/10.1016/j.biopsycho.2017.04.015
Corr PJ, McNaughton N (2012) Neuroscience and approach/avoidance personality traits: a two stage (valuation-motivation) approach. Neurosci Biobehav Rev 36(10):2339–2354. https://doi.org/10.1016/j.neubiorev.2012.09.013
Martel MM (2016) Dispositional trait types of ADHD in young children. J Atten Disord 20(1):43–52. https://doi.org/10.1177/1087054712466915
Hamilton JL et al (2017) Trait affect, emotion regulation, and the generation of negative and positive interpersonal events. Behav Ther. https://doi.org/10.1016/j.beth.2017.01.006
Fuhrmann D, Knoll LJ, Blakemore SJ (2015) Adolescence as a sensitive period of brain development. Trends Cogn Sci. https://doi.org/10.1016/j.tics.2015.07.008
Zimmermann KS, Richardson R, Baker KD (2019) Maturational changes in prefrontal and amygdala circuits in adolescence: implications for understanding fear inhibition during a vulnerable period of development. Brain Sci. https://doi.org/10.3390/brainsci9030065
Weinberger DR (1987) Implications of normal brain development for the pathogenesis of Schizophrenia. Arch Gen Psychiatry. https://doi.org/10.1001/archpsyc.1987.01800190080012
Paus T, Keshavan M, Giedd JNJNJN, Keshavan M, Paus T (2008) Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci 9(12):947–957. https://doi.org/10.1038/nrn2513
Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM (2003) The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev. https://doi.org/10.1016/S0149-7634(03)00007-1
Andersen SL, Teicher MH (2008) Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. https://doi.org/10.1016/j.tins.2008.01.004
Andersen SL (2016) Commentary on the special issue on the adolescent brain: adolescence, trajectories, and the importance of prevention. Neurosci Biobehav Rev. https://doi.org/10.1016/j.neubiorev.2016.07.012
Andersen SL (2003) Trajectories of brain development: point of vulnerability or window of opportunity? Neurosci Biobehav Rev. https://doi.org/10.1016/S0149-7634(03)00005-8
Andersen SL, Tomada A, Vincow ES, Valente E, Polcari A, Teicher MH (2008) Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. J Neuropsychiatry Clin Neurosci. https://doi.org/10.1176/jnp.2008.20.3.292
Marečková K, Klasnja A, Bencurova P, Andrýsková L, Brázdil M, Paus T (2019) Prenatal stress, mood, and gray matter volume in young adulthood. Cereb Cortex 29(3):1244–1250. https://doi.org/10.1093/cercor/bhy030
Mennes M, den Bergh BV, Lagae L, Stiers P (2009) Developmental brain alterations in 17 year old boys are related to antenatal maternal anxiety. Clin Neurophysiol 120(6):1116–1122. https://doi.org/10.1016/j.clinph.2009.04.003
Favaro A, Tenconi E, Degortes D, Manara R, Santonastaso P (2015) Neural correlates of prenatal stress in young women. Psychol Med 45(12):2533–2543. https://doi.org/10.1017/S003329171500046X
O’Donnell KJ, Glover V, Barker ED, O’Connor TG (2014) The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev Psychopathol 26(2):393–403. https://doi.org/10.1017/S0954579414000029
Glasheen C, Richardson GA, Kim KH, Larkby CA, Swartz HA, Day NL (2013) Exposure to maternal pre- and postnatal depression and anxiety symptoms: risk for major depression, anxiety disorders, and conduct disorder in adolescent offspring. Dev Psychopathol 25(4):1045–1063. https://doi.org/10.1017/S0954579413000369
Betts KS, Williams GM, Najman JM, Alati R (2014) Maternal depressive, anxious, and stress symptoms during pregnancy predict internalizing problems in adolescence. Depress Anxiety 31(1):9–18. https://doi.org/10.1002/da.22210
Betts KS, Williams GM, Najman JM, Alati R (2015) The relationship between maternal depressive, anxious, and stress symptoms during pregnancy and adult offspring behavioral and emotional problems. Depress Anxiety 32(2):82–90. https://doi.org/10.1002/da.22272
O’Donnell KJ, Glover V, Holbrook JD, O’Connor TG (2014) Maternal prenatal anxiety and child brain-derived neurotrophic factor (BDNF) genotype: effects on internalizing symptoms from 4 to 15 years of age. Dev Psychopathol 26(November):1255–1266. https://doi.org/10.1017/S095457941400100X
Van Den Bergh BRH et al (2006) ADHD deficit as measured in adolescent boys with a continuous performance task is related to antenatal maternal anxiety. Pediatr Res 59(1):78–82. https://doi.org/10.1203/01.pdr.0000191143.75673.52
Van Den Bergh BRH, Mulder EJH, Mennes M, Glover V (2005) Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: Links and possible mechanisms. A review. Neurosci Biobehav Rev 29(2):237–258. https://doi.org/10.1016/j.neubiorev.2004.10.007
O’Donnell KJ et al (2017) Maternal prenatal anxiety and child COMT genotype predict working memory and symptoms of ADHD. PLoS ONE. https://doi.org/10.1371/journal.pone.0177506
Mennes M, Stiers P, Lagae L, Van den Bergh BRH (2019) Antenatal maternal anxiety modulates the BOLD response in 20-year-old men during endogenous cognitive control. Brain Imaging Behav. https://doi.org/10.1007/s11682-018-0027-6
Mennes M, Stiers P, Lagae L, Van den Bergh B (2006) Long-term cognitive sequelae of antenatal maternal anxiety: involvement of the orbitofrontal cortex. Neurosci Biobehav Rev 30(8):1078–1086. https://doi.org/10.1016/j.neubiorev.2006.04.003
Van Den Bergh BRH et al (2005) High antenatal maternal anxiety is related to impulsivity during performance on cognitive tasks in 14- and 15-year-olds. Neurosci Biobehav Rev. https://doi.org/10.1016/j.neubiorev.2004.10.010
Braithwaite EC et al (2013) No moderating effect of 5-HTTLPR on associations between antenatal anxiety and infant behavior. J Am Acad Child Adolesc Psychiatry. https://doi.org/10.1016/j.jaac.2013.02.010
Cao-Lei L, Veru F, Elgbeili G, Szyf M, Laplante DP, King S (2016) DNA methylation mediates the effect of exposure to prenatal maternal stress on cytokine production in children at age 13½ years: project ice storm. Clin Epigenetics. https://doi.org/10.1186/s13148-016-0219-0
Cao-Lei L et al (2015) DNA methylation mediates the impact of exposure to prenatal maternal stress on BMI and central adiposity in children at age 13 1/2 years: project ice storm. Epigenetics. https://doi.org/10.1080/15592294.2015.1063771
Cao-Lei L, Dancause KN, Elgbeili G, Laplante DP, Szyf M, King S (2018) DNA methylation mediates the effect of maternal cognitive appraisal of a disaster in pregnancy on the child’s C-peptide secretion in adolescence: project ice storm. PLoS ONE. https://doi.org/10.1371/journal.pone.0192199
Krontira AC, Cruceanu C, Binder EB (2020) Glucocorticoids as mediators of adverse outcomes of prenatal stress. Trends Neurosci 43:394–405. https://doi.org/10.1016/j.tins.2020.03.008
Henrichs J, van den Heuvel MI, Witteveen AB, Wilschut J, Van den Bergh BRH (2021) Does mindful parenting mediate the association between maternal anxiety during pregnancy and child behavioral/emotional problems? Mindfulness. https://doi.org/10.1007/s12671-019-01115-9
Murphy SK et al (2017) Maternal infection and stress during pregnancy and depressive symptoms in adolescent offspring. Psychiatry Res. https://doi.org/10.1016/j.psychres.2017.07.025
Plant DT, Pariante CM, Sharp D, Pawlby S (2015) Maternal depression during pregnancy and offspring depression in adulthood: role of child maltreatment. Br J Psychiatry 207(3):213–220. https://doi.org/10.1192/bjp.bp.114.156620
Plant DT, Barker ED, Waters CS, Pawlby S, Pariante CM (2013) Intergenerational transmission of maltreatment and psychopathology: the role of antenatal depression. Psychol Med. https://doi.org/10.1017/S0033291712001298
Pearson RM et al (2016) Maternal perinatal mental health and offspring academic achievement at age 16: the mediating role of childhood executive function. J Child Psychol Psychiatry. https://doi.org/10.1111/jcpp.12483
Van Den Bergh BRH, Van Calster B, Smits T, Van Huffel S, Lagae L (2008) Antenatal maternal anxiety is related to HPA-axis dysregulation and self-reported depressive symptoms in adolescence: a prospective study on the fetal origins of depressed mood. Neuropsychopharmacology. https://doi.org/10.1038/sj.npp.1301450
Thomas JC et al (2017) Developmental origins of infant emotion regulation: Mediation by temperamental negativity and moderation by maternal sensitivity. Dev Psychol. https://doi.org/10.1037/dev0000279
Bailey NA, Irwin JL, Poggi Davis E, Sandman CA, Glynn LM (2021) Patterns of maternal distress from pregnancy through childhood predict psychopathology during early adoelscence. Child Psychiatry Human Dev. https://doi.org/10.1007/s10578-021-01259-7
Broerman R (2018) Diathesis-stress model. In: Zeigler-Hill V, Shackelford T (eds) Encyclopedia of personality and individual differences. Springer
Hartman S, Belsky J (2018) Prenatal stress and enhanced developmental plasticity. J Neural Transm 125(12):1759–1779. https://doi.org/10.1007/s00702-018-1926-9
Belsky J (1997) Variation in susceptibility to environmental influence: an evolutionary argument. Psychol Inq. https://doi.org/10.1207/s15327965pli0803_3
Clayborne ZM et al (2021) Prenatal maternal stress, child internalizing and externalizing symptoms, and the moderating role of parenting: findings from the Norwegian mother, father, and child cohort study. Psychol Med. https://doi.org/10.1017/S0033291721004311
Pickles A, Sharp H, Hellier J, Hill J (2017) Prenatal anxiety, maternal stroking in infancy, and symptoms of emotional and behavioral disorders at 3.5 years. Eur Child Adolesc Psychiatry 26(3):325–334. https://doi.org/10.1007/s00787-016-0886-6
Sharp H, Hill J, Hellier J, Pickles A (2015) Maternal antenatal anxiety, postnatal stroking and emotional problems in children: outcomes predicted from pre- and postnatal programming hypotheses. Psychol Med 45(2):269–283. https://doi.org/10.1017/S0033291714001342
Zhu P et al (2015) Sex-specific and time-dependent effects of prenatal stress on the early behavioral symptoms of ADHD: a longitudinal study in China. Eur Child Adolesc Psychiatry 24(9):1139–1147. https://doi.org/10.1007/s00787-015-0701-9
Thompson KL, Hannan SM, Miron LR (2014) Fight, flight, and freeze: Threat sensitivity and emotion dysregulation in survivors of chronic childhood maltreatment. Pers Individ Differ 69:28–32
Miu AC, Bîlc MI, Bunea I, Szentágotai-Tătar A (2017) Childhood trauma and sensitivity to reward and punishment: implications for depressive and anxiety symptoms. Personality Individ Differ 119:134–140. https://doi.org/10.1016/j.paid.2017.07.015
Vostanis P, Graves A, Meltzer H, Goodman R, Jenkins R, Brugha T (2006) Relationship between parental psychopathology, parenting strategies and child mental health: findings from the GB national study. Soc Psychiatry Psychiatr Epidemiol 41:509–514. https://doi.org/10.1007/s00127-006-0061-3
Thapar A, Sterhiakouli E (2008) Genetic influences on the development of childhood psychiatricdisorders. Psychiatry 7:7277–7281
Stoet G (2017) PsyToolkit: a novel web-based method for running online questionnaires and reaction-time experiments. Teach Psychol 44(1):24–31. https://doi.org/10.1177/0098628316677643
Stoet G (2010) PsyToolkit: a software package for programming psychological experiments using Linux. Behav Res Methods 42(4):1096–1104. https://doi.org/10.3758/BRM.42.4.1096
Duncan L et al (2018) Psychometric evaluation of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). Psychol Assess. https://doi.org/10.1037/pas0000541
First MB, Williams JBW, Karg RS, Spitzer RL (2016) SCID-5-CV: structured clinical interview for DSM-5 disorders, clinician version. American Psychiatric Publishing Inc
DuPaul GJ, Power TJ, Anastopoulos AD, Reid R (2016) ADHD rating scale-5 for children and adolescents. The Guilford Press, New York
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th Edition (DSM-5). American Psychiatric Publishing Inc, p 280
Központi Statisztikai Hivatal, “435 200 forint volt a bruttó átlagkereset,” GYORSTÁJÉKOZTATÓ. Keresetek, 2021. március, 2021.
Wechsler D (2008) Wechsler adult intelligence scale–Fourth Edition (WAIS–IV). APA PsycTests
Wechsler D (2003) Wechsler intelligence scale for children–Fourth Edition (WISC-IV). The Psychological Corporation, San Antonio
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress source. J Health Soc Behav 24(4):385–396
Lobel M, DeVincent CJCJ, Kaminer A, Meyer BABA (2000) The impact of prenatal maternal stress and optimistic disposition on birth outcomes in medically high-risk women. Health Psychol. https://doi.org/10.1037/0278-6133.19.6.544
Watson D, Clark LALALA, Tellegen A, Tellegan A, Tellegen A, Tellegan A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54:1063–1070. https://doi.org/10.1037/0022-3514.54.6.1063
Gratz KL, Roemer L (2004) Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 26:41–54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94
Buss AH, Perry M (1992) The aggression questionnaire. J Pers Soc Psychol 63(3):452–459
Sanders B, Becker-Lausen E (1995) The measurement of psychological maltreatment: early data on the child abuse and trauma scale. Child Abuse Negl 19(3):315–323. https://doi.org/10.1016/S0145-2134(94)00131-6
Corr PJ, Cooper AJ (2016) The reinforcement sensitivity theory of personality questionnaire (RST-PQ): development and validation. Psychol Assess 28(11):1427–1440
Rescorla LA, Achenbach TM, Rescorla LA (2004) The achenbach system of empirically based assessment (ASEBA) for ages 18 to 90 years. Routledge
Hayes AF (2018) Introduction to mediation, moderation, and conditional process analysis, second edition: a regression-based approach. The Guilford Press, New York
Sutherland S, Brunwasser SM (2018) Sex differences in vulnerability to prenatal stress: a review of the recent literature. Curr Psychiatry Rep. https://doi.org/10.1007/s11920-018-0961-4
Breslau J, Gilman SE, Stein BD, Ruder T, Gmelin T, Miller E (2017) Sex differences in recent first-onset depression in an epidemiological sample of adolescents. Transl Psychiatry. https://doi.org/10.1038/TP.2017.105
Dalsgaard S et al (2020) Incidence rates and cumulative incidences of the full spectrum of diagnosed mental disorders in childhood and adolescence. JAMA Psychiat. https://doi.org/10.1001/jamapsychiatry.2019.3523
Cerin E, MacKinnon DP (2009) A commentary on current practice in mediating variable analyses in behavioural nutrition and physical activity. Public Health Nutr. https://doi.org/10.1017/S1368980008003649
McLean MA, Cobham VE, Simcock G, Kildea S, King S (2019) Toddler temperament mediates the effect of prenatal maternal stress on childhood anxiety symptomatology: the QF2011 queensland flood study. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph16111998
Bosquet Enlow M, Devick KL, Brunst KJ, Lipton LR, Coull BA, Wright RJ (2017) Maternal lifetime trauma exposure, prenatal cortisol, and infant negative affectivity. Infancy. https://doi.org/10.1111/infa.12176
Otsuka A et al (2017) Interpersonal sensitivity mediates the effects of child abuse and affective temperaments on depressive symptoms in the general adult population. Neuropsychiatr Dis Treat. https://doi.org/10.2147/NDT.S144788
Levita L, Mayberry E, Mehmood A, Reuber M (2020) Evaluation of LiNES: a new measure of trauma, negative affect, and relationship insecurity over the life span in persons with FND. J Neuropsychiatry Clin Neurosci. https://doi.org/10.1176/appi.neuropsych.19050121
Allen B (2011) Childhood psychological abuse and adult aggression: the mediating role of self-capacities. J Interpers Violence. https://doi.org/10.1177/0886260510383035
Browne A, Finkelhor D (1986) Impact of child sexual abuse. A review of the research. Psychol Bull. https://doi.org/10.1037/0033-2909.99.1.66
Tull MT, Gratz KL, Latzman RD, Kimbrel NA, Lejuez CW (2010) Reinforcement sensitivity theory and emotion regulation difficulties: a multimodal investigation. Personality Individ Differ. https://doi.org/10.1016/j.paid.2010.08.010
Rádosi A et al (2021) The association between reinforcement sensitivity and substance use is mediated by individual differences in dispositional affectivity in adolescents. Addict Behav. https://doi.org/10.1016/j.addbeh.2020.106719
Vervoort L, Wolters LH, Hogendoorn SM, de Haan E, Boer F, Prins PJM (2010) Sensitivity of Gray’s behavioral inhibition system in clinically anxious and non-anxious children and adolescents. Personality Individ Differ. https://doi.org/10.1016/j.paid.2009.12.021
Lindeman M, Harakka T, Keltikangas-Järvinen L (1997) Age and gender differences in adolescents’ reactions to conflict situations: aggression, prosociality, and withdrawal. J Youth Adolesc. https://doi.org/10.1007/s10964-005-0006-2
Toldos MP (2005) Sex and age differences in self-estimated physical, verbal and indirect aggression in Spanish adolescents. Aggressive Behav. https://doi.org/10.1002/ab.20034
Kobulsky JM, Yoon S, Bright CL, Lee G, Nam B (2018) Gender-moderated pathways from childhood abuse and neglect to late-adolescent substance use. J Trauma Stress. https://doi.org/10.1002/jts.22326
Hentges RF, Graham SA, Plamondon A, Tough S, Madigan S (2019) A developmental cascade from prenatal stress to child internalizing and externalizing problems. J Pediatr Psychol. https://doi.org/10.1093/jpepsy/jsz044
Hayes AF (2013) Introduction to mediation, moderation, and conditional process analysis. Guilford Press, New York
Carver CS, White TL (1994) Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J Pers Soc Psychol 67(2):319. https://doi.org/10.1037/0022-3514.67.2.319
Bunford N, Kujawa A, Dyson M, Olino T, Klein DN (2021) Developmental pathways from preschool temperament to early adolescent ADHD symptoms through initial responsiveness to reward. Dev Psychopathol 16:1–13. https://doi.org/10.1017/S0954579420002199
Tully EC, Iacono WG (2016) An integrative common liabilities model for the comorbidity of substance use disorders with externalizing and internalizing disorders. The oxford handbook of substance use and substance use disorders. Oxford University Press
Dugré JR et al (2020) Developmental joint trajectories of anxiety-depressive trait and trait-aggression: implications for co-occurrence of internalizing and externalizing problems. Psychol Med. https://doi.org/10.1017/S0033291719001272
Lahey BB (2009) Public health significance of neuroticism. Am Psychol. https://doi.org/10.1037/a0015309
Li X, Laplante DP, Paquin V, Lafortune S, Elgbeili G, King S (2022) Effectiveness of cognitive behavioral therapy for perinatal maternal depression, anxiety and stress: a systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev 92:102–129. https://doi.org/10.1016/j.cpr.2022.102129
Hong K et al (2021) Perspectives on antenatal education associated with pregnancy outcomes: systematic review and meta-analysis. Women Birth 34(3):219–230. https://doi.org/10.1016/j.wombi.2020.04.002
Missler M et al (2021) Universal prevention of distress aimed at pregnant women: a systematic review and meta-analysis of psychological interventions. BMC Pregnancy Childbirth. https://doi.org/10.1186/s12884-021-03752-2
Thomas M et al (2014) Potential for a stress reduction intervention to promote healthy gestational weight gain: focus groups with low-income pregnant women. Women’s Health Issues. https://doi.org/10.1016/j.whi.2014.02.004
Fontein-Kuipers YJ, Nieuwenhuijze MJ, Ausems M, Budé L, De Vries R (2014) Antenatal interventions to reduce maternal distress: a systematic review and meta-analysis of randomised trials. BJOG Int J Obstet Gynaecol 121(4):389–394. https://doi.org/10.1111/1471-0528.12500
Kwon R, Kasper K, London S, Haas DM (2020) A systematic review: the effects of yoga on pregnancy. Eur J Obstet Gynecol Reprod Biol 250:171–177. https://doi.org/10.1016/j.ejogrb.2020.03.044
Hajesmaeel-Gohari S, Sarpourian F, Shafiei E (2021) Virtual reality applications to assist pregnant women: a scoping review. BMC Pregnancy Childbirth 21(1):249. https://doi.org/10.1186/s12884-021-03725-5
Nicholson JM et al (2016) Enhancing the early home learning environment through a brief group parenting intervention: study protocol for a cluster randomised controlled trial. BMC Pediatr. https://doi.org/10.1186/s12887-016-0610-1
Barnes J et al (2017) Randomized controlled trial and economic evaluation of nurse-led group support for young mothers during pregnancy and the first year postpartum versus usual care. Trials 18(1):1–15. https://doi.org/10.1186/s13063-017-2259-y
Ashburn K, Kerner B, Ojamuge D, Lundgren R (2017) Evaluation of the responsible, engaged, and loving (REAL) Fathers initiative on physical child punishment and intimate partner violence in Northern Uganda. Prev Sci 18(7):854–864. https://doi.org/10.1007/s11121-016-0713-9
Khowaja Y, Karmaliani R, Hirani S, Khowaja AR, Rafique G, McFarlane J (2016) A pilot study of a 6-week parenting program for mothers of pre-school children attending family health centers in Karachi, Pakistan. Int J Health Policy Manag 5(2):91–97. https://doi.org/10.15171/ijhpm.2015.181
Takahashi Y, Yamagata S, Kijima N, Shigemasu K, Ono Y, Ando J (2007) Continuity and change in behavioral inhibition and activation systems: a longitudinal behavioral genetic study. Personality Individ Differ. https://doi.org/10.1016/j.paid.2007.04.030
Cella M, Bishara AJ, Medin E, Swan S, Reeder C, Wykes T (2014) Identifying cognitive remediation change through computational modelling–effects on reinforcement learning in schizophrenia. Schizophr Bull 40(6):1422–1432. https://doi.org/10.1093/schbul/sbt152
Ryan J, Pouliot JJ, Hajcak G, Nee DE (2022) Manipulating reward sensitivity using reward circuit-targeted transcranial magnetic stimulation. Biol Psychiatry Cognitive Neurosci Neuroimaging 7(8):833–840. https://doi.org/10.1016/j.bpsc.2022.02.011
Karimpour-Vazifehkhorani A, Bakhshipour Rudsari A, Rezvanizadeh A, Kehtary-Harzang L, Hasanzadeh K (2020) Behavioral activation therapy on reward seeking behaviors in depressed people: an experimental study. J Caring Sci 9(4):195–202. https://doi.org/10.34172/jcs.2020.030
Karl JA, Fischer R, Jose PE (2021) The development of mindfulness in young adults: the relationship of personality, reinforcement sensitivity, and mindfulness. Mindfulness 12(5):1103–1114
Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MH, Van Ijzendoorn MJ (2007) Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull 133(1):1
Gidron Y (2013) Trait anxiety. In: Gellman MD, Turner JR (eds) Encyclopedia of behavioral medicine. Springer, New York, p 1989
Bell DC, Bell LG (2018) Accuracy of retrospective reports of family environment. J Child Fam Stud 27:1029–1040. https://doi.org/10.1007/s10826-017-0948-5
Kark JD, Troya G, Friedlander Y, Slater PE, Stein Y (1984) Validity of maternal reporting of breast feeding history and the association with blood lipids in 17 year olds in Jerusalem. J Epidemiol Community Health. https://doi.org/10.1136/jech.38.3.218
Rice F et al (2007) Agreement between maternal report and antenatal records for a range of pre and peri-natal factors: the influence of maternal and child characteristics. Early Human Dev. https://doi.org/10.1016/j.earlhumdev.2006.09.015
Ramos AM, Marceau K, Neiderhiser JM, De Araujo-Greecher M, Natsuaki MN, Leve LD (2020) Maternal consistency in recalling prenatal experiences at 6 months and 8 years postnatal. J Dev Behav Pediatr. https://doi.org/10.1097/DBP.0000000000000841
DiLalla LF, Trask MMC, Casher GA, Long SS (2020) Evidence for reliability and validity of parent reports of twin children’s birth information. Early Childhood Res Q. https://doi.org/10.1016/j.ecresq.2019.10.011
Gatzke-Kopp LM (2011) The canary in the coalmine: the sensitivity of mesolimbic dopamine to environmental adversity during development. Neurosci Biobehav Rev. https://doi.org/10.1016/j.neubiorev.2010.09.013
Parylak SL, Koob GF, Zorrilla EP (2011) The dark side of food addiction. Physiol Behav 104(1):149–156. https://doi.org/10.1016/j.physbeh.2011.04.063
Winer ES, Cervone D, Bryant J, McKinney C, Liu RT, Nadorff MR (2016) Distinguishing mediational models and analyses in clinical psychology: atemporal associations do not imply causation. J Clin Psychol. https://doi.org/10.1002/jclp.22298
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Personal Soc Psychol. https://doi.org/10.1037//0022-3514.51.6.1173
MacKinnon DP, Fairchild AJ, Fritz MS (2007) Mediation analysis. Annu Rev Psychol. https://doi.org/10.1146/annurev.psych.58.110405.085542
Mackinnon DP, Dwyer JH (1993) Estimating mediated effects in prevention studies. Eval Rev. https://doi.org/10.1177/0193841X9301700202
Hayes AF, Scharkow M (2013) The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis: does method really matter? Psychol Sci. https://doi.org/10.1177/0956797613480187
Bunford N, Brandt NE, Golden C, Dykstra JB, Suhr JA, Owens JS (2015) Attention-deficit/hyperactivity disorder symptoms mediate the association between deficits in executive functioning and social impairment in children. J Abnorm Child Psychol 43(1):133–147. https://doi.org/10.1007/s10802-014-9902-9
Rinsky JR, Hinshaw SP (2011) Linkages between childhood executive functioning and adolescent social functioning and psychopathology in girls with ADHD. Child Neuropsychol. https://doi.org/10.1080/09297049.2010.544649
Bunford N, Kujawa A, Fitzgerald KDKD, Monk CSCS, Phan KLL (2018) Convergence of BOLD and ERP measures of neural reactivity to emotional faces in children and adolescents with and without anxiety disorders. Biol Psychol 134:9–19. https://doi.org/10.1016/j.biopsycho.2018.02.006
Agler R, De Boeck P (2017) On the interpretation and use of mediation: multiple perspectives on mediation analysis. Front Psychol. https://doi.org/10.3389/fpsyg.2017.01984
Danner D, Hagemann D, Fiedler K (2015) Mediation analysis with structural equation models: combining theory, design, and statistics. Eur J Soc Psychol. https://doi.org/10.1002/ejsp.2106
Shadish WR, Cook TD, Campbell DT (2002) Experimental and quasi-experimental designs for generalized causal inference. Houghton Mifflin, Boston
Funding
Open access funding provided by ELKH Research Centre for Natural Sciences. This research was funded by a Hungarian Academy of Sciences Momentum (“MTA Lendület”) Grant awarded to NB (#LP2018-3/2018). During the preparation of this article, AR was supported by New National Excellence Programme (ÚNKP-21–3-II-SE-53) and SE250 + (EFOP-3.6.3-VEKOP-16–2017-00009) fellowships and JMR was supported by the Higher Education Institutional Excellence Programme of the Ministry of Human Capacities in Hungary, within the framework of the Neurology thematic programme of Semmelweis University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the Authors have any biomedical or financial conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sebők-Welker, T., Posta, E., Ágrez, K. et al. The Association Between Prenatal Maternal Stress and Adolescent Affective Outcomes is Mediated by Childhood Maltreatment and Adolescent Behavioral Inhibition System Sensitivity. Child Psychiatry Hum Dev 55, 1–21 (2024). https://doi.org/10.1007/s10578-023-01499-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-023-01499-9