Abstract
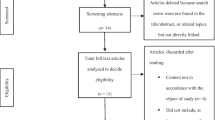
Inconsistent results of the association between severe psychiatric disorders (SPD) in parents and the risk of disruptive behavioral disorders (DBD) including conduct disorders (CD) and oppositional defiant disorders (ODD) in the offspring have been found by previous epidemiologic studies. PubMed, EMBASE, PsycINFO, and Scopus were searched for relevant studies. Fourteen studies met the predefined criteria for inclusion. A meta-analysis of the included studies revealed an elevated risk of DBD in the offspring of parents with SPD, bipolar, and depressive disorders. Our further analysis considering the specific DBD as an outcome showed that parents with SPD are at an increased risk of having a child with ODD as well as CD. Moreover, the current meta-analysis found that the children of parents with bipolar disorder were also at increased risk of ODD and CD. Parental schizophrenia and depressive disorders were not associated with higher risks of ODD and CD in the offspring.





Similar content being viewed by others
Abbreviations
- BD:
-
Bipolar disorder
- CES-D:
-
Center for epidemiologic studies depression scale
- CD:
-
Conduct disorder
- DBD:
-
Disruptive behavioural disorder
- DSM-III:
-
Diagnostic and statistical manual of mental disorders (DSM), third edition
- DSM-IV:
-
Diagnostic and statistical manual of mental disorders (DSM), fourth edition
- FEM:
-
Fixed effect model
- ICD:
-
International classification of disease
- K-SADS:
-
Kiddie schedule for affective disorders
- MDD:
-
Major depressive disorders
- ODD:
-
Oppositional defiant disorder
- OR:
-
Odds ratio
- RR:
-
Relative RISK
- SPD:
-
Severe psychiatric disorder
- REM:
-
Random effect model
- UK:
-
United Kingdom
- USA:
-
United States of America
References
Diagnostic and statistical manual of mental disorders-IV-TR (2000) Washington American Psychiatric Association American Psychiatric Association DC
Diagnostic Stastistical Manual of Mental Disorder (5th edition). Wahington, DC: American Psychiatric Association; American Psychiatric Association, (2013)
Ogundele MO (2018) Behavioural and emotional disorders in childhood: a brief overview for paediatricians. World J Clin Pediatr 7(1):9–26
Biederman J, Petty CR, Dolan C, Hughes S, Mick E, Monuteaux MC, Faraone SV (2008) The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychol Med 38(7):1027–1036
Carr EG, Taylor JC, Robinson S (1991) The effects of severe behavior problems in children on the teaching behavior of adults. J Appl Behav Anal 24(3):523–535
Ayano G, Yohannes K, Abraha M (2020) Epidemiology of attention-deficit/hyperactivity disorder (ADHD) in children and adolescents in Africa: a systematic review and meta-analysis. Ann Gen Psychiatry 19(1):21
Nock MK, Kazdin AE, Hiripi E, Kessler RC (2007) Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: results from the National Comorbidity Survey Replication. J Child Psychol Psychiatry 48:703–713
Erskine HE, Ferrari AJ, Nelson P, Polanczyk GV, Flaxman AD, Vos T, Whiteford HA, Scott JG (2013) Epidemiological modelling of attention-deficit/hyperactivity disorder and conduct disorder for the Global Burden of Disease Study 2010. J Child Psychol Psychiatry 54(12):1263–1274
Rowe R, Maughan B, Pickles A, Costello EJ, Angold A (2002) Psychiatry: the relationship between DSM-IV oppositional defiant disorder and conduct disorder: findings from the Great Smoky Mountains Study. J Child Psychol Psychiatry 43(3):365–373
Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, Faraone SV (2002) Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am J Psychiatry 159(7):1214–1224
Nordstrom T, Ebeling H, Hurtig T, Rodriguez A, Savolainen J, Moilanen I, Taanila A (2013) Comorbidity of disruptive behavioral disorders and attention-deficit hyperactivity disorder–indicator of severity in problematic behavior? Nord J Psychiatry 67(4):240–248
Linker J, Gillespie NA, Maes H, Eaves L, Silberg JL (2012) Suicidal ideation, depression, and conduct disorder in a sample of adolescent and young adult twins. Suicide Life Threat Behav 42(4):426–436
Teubert D, Pinquart M (2011) A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. J Anxiety Disord 25(8):1046–1059
Morgan AJ, Rapee RM, Bayer JK (2016) Prevention and early intervention of anxiety problems in young children: a pilot evaluation of Cool Little Kids Online. Internet Interv 4:105–112
Rasic D, Hajek T, Alda M, Uher R (2014) Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk studies. Schizophr Bull 40(1):28–38
Reupert AE (2013) D JM, Kowalenko NM: Children whose parents have a mental illness: prevalence, need and treatment. Med J Aust 199(3 Suppl):S7–9
Lau P, Hawes DJ, Hunt C, Frankland A, Roberts G, Mitchell PB (2018) Prevalence of psychopathology in bipolar high-risk offspring and siblings: a meta-analysis. Eur Child Adolesc Psychiatry 27(7):823–837
Ayano G, Maravilla JC, Alati R (2019) Risk of autistic spectrum disorder in offspring with parental mood disorders: a systematic review and meta-analysis. J Affect Disord 248:185–197
Perich T, Lau P, Hadzi-Pavlovic D, Roberts G, Frankland A, Wright A, Green M, Breakspear M, Corry J, Radlinska B et al (2015) What clinical features precede the onset of bipolar disorder? J Psychiatr Res 62:71–77
Lee SH, Ripke S, Neale BM, Faraone SV, Purcell SM, Perlis RH, Mowry BJ, Thapar A, Goddard ME, Witte JS (2013) Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat Genet 45(9):984
Coleman PK, Karraker KH (1998) (1998) Self-efficacy and parenting quality: findings and future applications. Dev Rev 18(1):47–85
Darling N, Steinberg L (1993) Parenting style as context: An integrative model. Psychol Bull 113(3):487–496
Hammen C (1997) Children of depressed parents. In: Handbook of children’s coping. Springer, 131–157.
Oyserman D, Mowbray CT, Meares PA, Firminger KB (2000) Parenting among mothers with a serious mental illness. Am J Orthopsychiatry 70(3):296–315
McLoyd VC, Jayaratne TE, Ceballo R, Borquez J (1994) Unemployment and work interruption among African American single mothers: effects on parenting and adolescent socioemotional functioning. Child Dev 65(2):562–589
Henin A, Biederman J, Mick E, Sachs GS, Hirshfeld-Becker DR, Siegel RS, McMurrich S, Grandin L, Nierenberg AA (2005) Psychopathology in the offspring of parents with bipolar disorder: a controlled study. Biol Psychiatry 58(7):554–561
Mars B, Collishaw S, Smith D, Thapar A, Potter R, Sellers R, Harold GT, Craddock N, Rice F, Thapar A (2012) Offspring of parents with recurrent depression: which features of parent depression index risk for offspring psychopathology? J Affect Disord 136(1–2):44–53
Nurnberger JI, Mcinnis M, Reich W, Kastelic E, Wilcox HC, Glowinski A, Mitchell P, Fisher C, Erpe M, Gershon ES, Berrettini W, Laite G, Schweitzer R, Rhoadarmer K, Coleman VV, Cai X, Azzouz F, Liu H, Kamali M, Brucksch C, Monahan PO (2011) A high-risk study of bipolar disorder: childhood clinical phenotypes as precursors of major mood disorders. Arch Gen Psychiatry 68(10):1012–1020
Hans SL, Auerbach JG, Styr B, Marcus J (2004) Offspring of parents with schizophrenia: mental disorders during childhood and adolescence. Schizophr Bull 30(2):303–315
Reviews UoYCf, Dissemination: Systematic reviews: CRD's guidance for undertaking reviews in health care: University of York, Centre for Reviews & Dissemination; 2009.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):1–6
Wells G: Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. (2011) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Samuel B. Guze (1995) diagnostic and statistical manual of mental disorders, 4th ed. (DSM-IV), 152(8):1228–1228
Pichot P (1986) [DSM-III: the 3d edition of the Diagnostic and Statistical Manual of Mental Disorders from the American Psychiatric Association]. Revue neurologique, 142(5):489–499.
Borenstein M, Hedges L, Higgins J, Rothstein H (2005) Comprehensive meta-analysis version 2. Biostat, Englewood, NJ, p 104
Borenstein M, Hedges LV, Higgins J, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1(2):97–111
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ Br Med J 327(7414):557
Patsopoulos NA, Evangelou E, Ioannidis JP (2008) Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol 37(5):1148–1157
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Glasheen C, Richardson GA, Kim KH, Larkby CA, Swartz HA, Day NL (2013) Exposure to maternal pre- and postnatal depression and anxiety symptoms: risk for major depression, anxiety disorders, and conduct disorder in adolescent offspring. Dev Psychopathol 25(4 Pt 1):1045–1063
Nurnberger JI, McInnis M, Reich W, Kastelic E, Wilcox HC, Glowinski A, Mitchell P, Fisher C, Erpe M, Gershon ES et al (2011) A high-risk study of bipolar disorder: childhood clinical phenotypes as precursors of major mood disorders. Arch Gen Psychiatry 68(10):1012–1020
Halligan SL, Murray L, Martins C, Cooper PJ (2007) Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. J Affect Disord 97(1–3):145–154
Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, Obreja M, Ehmann M, Iyengar S, Shamseddeen W et al (2009) Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: the pittsburgh bipolar offspring study. Arch Gen Psychiatry 66(3):287–296
Goetz M, Sebela A, Mohaplova M, Ceresnakova S, Ptacek R, Novak T (2017) Psychiatric disorders and quality of life in the offspring of parents with bipolar disorder. J Child Adolesc Psychopharmacol 27(6):483–493
Maoz H, Goldstein T, Axelson DA, Goldstein BI, Fan J, Hickey MB, Monk K, Sakolsky D, Diler RS, Brent D et al (2014) Dimensional psychopathology in preschool offspring of parents with bipolar disorder. J Child Psychol Psychiatry 55(2):144–153
Hirshfeld-Becker DR, Biederman J, Henin A, Faraone SV, Dowd ST, De Petrillo LA, Markowitz SM, Rosenbaum JF (2006) Psychopathology in the young offspring of parents with bipolar disorder: a controlled pilot study. Psychiatry Res 145(2–3):155–167
Goldstein BI, Shamseddeen W, Axelson DA, Kalas C, Monk K, Brent DA, Kupfer DJ, Birmaher B (2010) Clinical, demographic, and familial correlates of bipolar spectrum disorders among offspring of parents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 49(4):388–396
Sanchez-Gistau V, Romero S, Moreno D, de la Serna E, Baeza I, Sugranyes G, Moreno C, Sanchez-Gutierrez T, Rodriguez-Toscano E, Castro-Fornieles J (2015) Psychiatric disorders in child and adolescent offspring of patients with schizophrenia and bipolar disorder: a controlled study. Schizophr Res 168(1–2):197–203
Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, Cooper P (2011) Maternal postnatal depression and the development of depression in offspring up to 16 years of age. J Am Acad Child Adolesc Psychiatry 50(5):460–470
Vandeleur C, Rothen S, Gholam-Rezaee M, Castelao E, Vidal S, Favre S, Ferrero F, Halfon O, Fumeaux P, Merikangas KR et al (2012) Mental disorders in offspring of parents with bipolar and major depressive disorders. Bipolar Disord 14(6):641–653
Grigoroiu-Serbanescu M, Christodorescu D, Magureanu S, Jipescu I, Totoescu A, Marinescu E, Ardelean V, Popa S (1991) Adolescent offspring of endogenous unipolar depressive parents and of normal parents. J Affect Disord 21(3):185–198
Ferrari A, Somerville A, Baxter A, Norman R, Patten S, Vos T, Whiteford HA (2013) Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol Med 43(3):471–481
Jirtle RL, Skinner MK (2007) Environmental epigenomics and disease susceptibility. Nat Rev Genet 8(4):253–262
Prickett AR, Oakey RJ (2012) genomics: a survey of tissue-specific genomic imprinting in mammals. Mol Genet Genomics 287(8):621–630
Kundakovic M, Jaric I (2017) The epigenetic link between prenatal adverse environments and neurodevelopmental disorders. Genes (Basel) 8(3):104
Ptak C, Petronis A (2010) Epigenetic approaches to psychiatric disorders. Dialogues Clin Neurosci 12(1):25–35
Nestler EJ, Pena CJ, Kundakovic M, Mitchell A, Akbarian S (2016) Epigenetic basis of mental illness. The Neuroscientist 22(5):447–463
Knudsen AK, Ystrom E, Skogen JC, Torgersen L (2015) Maternal heavy alcohol use and toddler behavior problems: a fixed effects regression analysis. Eur Child Adolesc Psychiatry 24(10):1269–1277
Edwards EP, Eiden RD, Colder C, Leonard KE (2006) The development of aggression in 18 to 48 month old children of alcoholic parents. J Abnorm Child Psychol 34(3):393–407
Parvaresh N, Ziaaddini H, Kheradmand A, Bayati H (2010) Attention deficit hyperactivity disorder (ADHD) and conduct disorder in children of drug dependent parents. Addict Health 2(3–4):89–94
Mayes SD, Waxmonsky JD, Calhoun SL, Bixler EO (2016) Disruptive mood dysregulation disorder symptoms and association with oppositional defiant and other disorders in a general population child sample. J Child Adolesc Psychopharmacol 26(2):101–106
Cerdá M, Sagdeo A, Johnson J, Galea S (2010) Genetic and environmental influences on psychiatric comorbidity: a systematic review. J Affect Disord 126(1):14–38
Gjone H, Stevenson J (1997) The association between internalizing and externalizing behavior in childhood and early adolescence: genetic or environmental common influences? J Abnorm Child Psychol 25(4):277–286
McCoy BM, Rickert ME, Class QA, Larsson H, Lichtenstein P, Donofrio BM (2014) Mediators of the association between parental severe mental illness and offspring neurodevelopmental problems. Ann Epidemiol 24(9):629–634
MacCabe JH, Martinsson L, Lichtenstein P, Nilsson E, Cnattingius S, Murray RM, Hultman CM (2007) Adverse pregnancy outcomes in mothers with affective psychosis. Bipolar Disord 9(3):305–309
Nilsson E, Hultman CM, Cnattingius S, Olausson PO, Björk C, Lichtenstein P (2018) Schizophrenia and offspring's risk for adverse pregnancy outcomes and infant death. Br J Psychiatry 193(4):311–315
Nilsson E, Lichtenstein P, Cnattingius S, Murray RM, Hultman CM (2002) Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 58(2):221–229
Mattejat F, Remschmidt H (2008) The children of mentally ill parents. Dtsch Arztebl Int 105(23):413–418
Hasin D, Kilcoyne B (2012) Comorbidity of psychiatric and substance use disorders in the United States: current issues and findings from the NESARC. Curr Opin Psychiatry 25(3):165–171
Bountress K, Chassin L (2015) Risk for behavior problems in children of parents with substance use disorders. Am J Orthopsychiatry 85(3):275–286
Fu Q, Heath AC, Bucholz KK, Nelson E, Goldberg J, Lyons MJ, True WR, Jacob T, Tsuang MT, Eisen SA (2002) Shared genetic risk of major depression, alcohol dependence, and marijuana dependence: contribution of antisocial personality disorder in men. Arch Gen Psychiatry 59(12):1125–1132
Acknowledgements
We are grateful to the University of Queensland and Curtin University for providing us a wide range of available online databases.
Funding
No external funding obtained for this systematic review and meta-analysis.
Author information
Authors and Affiliations
Contributions
GA conceptualized the study, developed the methodology, identified all potential studies, abstracted the data, evaluated the quality of the studies, performed the analysis, and developed the first draft of the manuscript. JCM abstracted the data and evaluated quality. KB reviewed the draft of the manuscript and the analysis. RA reviewed the designed protocol, reviewed data abstraction, and analysis and contributed to the development of the subsequent manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ayano, G., Betts, K., Maravilla, J.C. et al. A Systematic Review and Meta-Analysis of the Risk of Disruptive Behavioral Disorders in the Offspring of Parents with Severe Psychiatric Disorders. Child Psychiatry Hum Dev 52, 77–95 (2021). https://doi.org/10.1007/s10578-020-00989-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-020-00989-4