Abstract
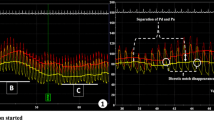
Objective: By applying a clinical decision system, the Noninvasive Hemodynamic Analyzer (NHA), demonstrates its capability to compute the Myocardial Hemodynamic status of exercising patients. Design: Retrospective study to use the average vital signs and anthropological data of a large clinical trial of Exercise Treadmill Test. The NHA system computes Stroke Volume and various hemodynamic parameters. With the assistance of the NHA computer-aided clinical decision system; the Epicardial and Endocardial Blood Pressure/Blood Flow relationships, as well as components or determinants of Myocardial Oxygen Supply during exercise treadmill test were calculated. Patients: Four groups of the clinical study (1) Healthy, (2) Hypertensive, (3) Angina Pectoris, and (4) Post-Myocardial Infarction and Angina Pectoris were used in this study which comprised the average data of several hundred patients. Each group had three subgroups according to the Exercise Treadmill Test, upright and two exercise periods. Validity: We previously conducted a comparative study of Stroke Volume computed by the NHA with the Thermodilution technique which proved to be clinically acceptable concerning Bias, Accuracy, and Precision. In this particular study, the statistical evaluation was not available because the average values did not allow for such computation. Instead, we have chosen to compute the Myocardial Hemodynamic Parameters parallel with their Ideal values. Altogether 18 hemodynamic parameters were included and the normal values were expressed in ± 20%. Conclusion: The NHA clinical decision system can differentiate among the reported clinical conditions of the “Seattle Heart Watch” report. We were able to comparatively evaluate physiological and pathophysiological principles, such as, coronary flow reserve, endocardial autoregulation, and remodeling. Further medical trials will reveal the practical clinical importance and applicability of our NHA system.
Similar content being viewed by others
References
Abboud FM, and Smid PG. Regulation of peripheral and coronary circulation. In Levine HJ, Ed, Clinical Cardiovascular Physiology. New York: Grune & Stratton, 1976, pp. 143–205.
Andersen FR, llebekk A, and Kill F. Variations in left ventricular volume after myocardial oxygen consumption more at low then at high inotropy. Acta Physiol Scand 193(1): 95–102, 1990.
Bai XJ, Iwamoto T, William AG, Fan WL, and Downey HFI. Coronary pressure-flow autoregulation protects myocardium from pressure-induced changes in oxygen consumption. Am J Physiol 266(6Pt 2): H2359–H2368, 1994.
Bianco JA, and Alpert JS. Physiologic and clinical significance of myocardial blood flow quantitation: What is expected from these measurements in the clinical ward and in the physiology laboratory? Cardiology 88(1): 116–126, 1997.
Bourdarias JP. Coronary reserve: Concept and physiological variations. Eur Heart J 16(Suppl 1): 2–6, 1955.
Britten MB, Zeiher AN, and Schaechinger V. Effects of cardiovascular risk factors on coronary remodeling in patients with mild atherosclerosis. Coron Artery Dis 14(6): 415–422, Sep 2003.
Bruce RA, Gey GO, Cooper MN, Fischer LD, and Peterson DR. Seattle Heart Watch: Initial clinical, circulatory and electrocardiographic responses to maximal exercise. Am J Cardiol 33: 459–469, 1974.
Bruce RA and Hornstein TR. Exercise stress testing in evaluation of patients with ischemic heart disease. Prog Cardiovasc Dis 11: 371–390, 1979.
Chilian WM. Coronary microcirculation in health and disease: Summary of an NHLBI workshop. Circulation 95: 522–528, 1997.
De Boer RA, Pinto YM, and Van Veidhuisen DJ. The imbalance between oxygen demand and supply as a potential mechanism in the pathophysiology of heart failure: The role of microvascular growth and abnormalities. Microcircuiation 10(2): 113–126, Apr 2003.
Deedwania PC. Hemodynamic variability and myocardial ischemia. Cardiol Clin 13(3): 491–500, Nov 1995.
DeFily DV, and Chilian WM. Coronary microcircuiation: autoregulation and metabolic control. Basic Res Cardiol 90(2): 112–118, 1995.
Di Giantomasso D, May CN, and Bellomo R. Norepinephrine and vital organ blood flow. Intensive Care Med 28(12): 1804–1809, 2002.
Edwards WD. Applied anatomy of the heart. In Brandenburg RO, Fuster V, Giuliani ER, et al., Eds, Cardiology: Fundamentals and Practice. Chicago Yearbook Medical Publishers, 1987, Vol 47, p. 112.
Factor SM, and Bache RJ. Pathophysiology of myocardial ischemia. Chapter 7. In Schlant RC and Alexander RW, Eds, Hurst's The Heart, Arteries and Veins, 8th ed. New York: McGraw-Hill, 1994, pp. 1033–1053.
Falls HB (Ed). The cardiovascular system in exercise. In Exercise Physiology, Modified by Anderson KL. New York: Academic Press, 1968.
Froelicher VF, Fearon WF, Ferguson CM, et al. Lesson learned from studies of the standard exercise EGG test. Chest 116: 1442–1451, 1999.
Fuster V, Badimon L, Badimon JJ, and Chesebro JH. The pathogenesis of coronary artery disease and the acute coronary syndromes. N Engl J Med 326: 242–247, 1992.
Gosse P, and Clementy J. Coronary reserve in experimental myocardial hypertrophy. Eur Heart J 16(Suppl): 22–25, 1995.
Gutgesell HP, and Rembold CM. Growth of the human heart relative to body surface area. Am J Cardiol 65(9): 662–668, 1990.
Harrison DG, Treasure CB, Mugge A, Dellsperger KC, Lamping KG. Hypertension and the coronary circulation. With special attention to endothelial regulation. Am J Hypertens, 4(7 Pt 2): 454S-459S, July 19XX .
Hoffman E, and Sclafani R. The coronary circulation and myocardial ischemia. Ital Heart J 1(Suppl 2): 7–12, June 2000.
Hoffman JIE, and Buckberg GD. Transmural variations in myocardial perfusion. In: Yu PN, Goodwin JF, Eds, Progress in Cardiology Philadelphia, Pennsylvania: Lea & Febiger, 1976, pp 37– 38.
Kabal J, and Lagerman BK. A novel approach to measure cardiac output noninvasively. A comparison with the thermodilution method on critical care patients. J Clin Monit 18(3): 1–9, 2004a.
Kabal J, and Lagerman BK. Hemodynamic evaluation of Exercise Treadmill Test by a computer aided clinical decision system. Cardiovasc Eng: Int J 4(3): 245–259, Sept 2004b.
Kabal J, and Lagerman BK. Computer-aided clinical decision system: Differential diagnosis and treatment of essential hypertension by a novel noninvasive hemodynamic analyzer. Cardiovasc Eng: Int J 5(2): 83–96, June 2005.
Kannel WB. Left ventricular hypertrophy as a risk factor: The Framingham experience. J Hypertens 9(Suppl 2): S3–S9, 1991.
Maruyama Y, Hory M, and Janicky JS. Cardiac-vascular remodeling and functional interaction. Springer Verlag New York 1997.
Mosher P, Ross J, McFate PA, and Shaw RF. Control of coronary blood flow by an autoregulatory mechanism. Circ Res 14: 250–259, 1964.
Mundhenke M, Schwarzkopff B, and Strauer BE. Structural analysis of arteriolar and myocardial remodeling in the subendocardial region of patients with hypertensive heart disease and hypertrophic cardiomyopathy. Virchows Arch 431(4): 265–273, 1997.
Nitenberg A, and Antony I. Coronary vascular reserve in humans: A critical review of methods of evaluation and of interpretation of the results. Eur Heart J 16(Suppl 1): 7–21, Aug 1995.
Pagliaro P, Chiribiri A, Mancardi D, Rastaldi R, Gattulo D, and Losano G. Coronary endothelial dysfunction after ischemia and reperfusion and its prevention by ischemic preconditioning. Ital Heart J 4(6): 383–394, August 6, 2003.
Schremmer B, and Dhainaut JF. Regulation of myocardial oxygen delivery. Intensive Care Med 16(Suppl 2): 157–163, 1990.
Schaefer S, Kelm M, Mingers S, and Strauer BE. Left ventricular remodeling impairs coronary flow reserve in hypertensive patients. J Hypertens 20(7): 1431–1437, July 2002.
Smith TW. Heart failure. In Wyngaarden JB, Smith LH, and Bennett JC, Eds, Cecil Textbook of Medicine, 19th ed. Philadelphia, PA: Saunders, 1992, p 192.
Strauer BE. The significance of coronary reserve in clinical heart disease. J Am Coll Cardiol 15: 775–783, 1990.
Upton MT, Rerich SK, Roeback JR, Newman GE, Douglas JM, Wallace AG, and Jones RH. Effect of brief and prolonged exercise on left ventricular function. Am J Cardiol 45: 1154–1160, 1980.
Wallbridge DR, and Cobbe SM. Coronary hemodynamics in left ventricular hypertrophy. Heart 75(4): 369–376, 1996.
Weber KT, Anversa P, Armstrong PW, Brilla CG, Burnett JC, Crickshank JM, and Devereux RB. Remodeling and reparation of the cardiovascular system. J Am Coll Cardiol 20: 3–16, 1992.
Willenheimer R. Left ventricular remodeling and dysfunction. Can the process be prevented? Int J Cardiol 72(2): 143–150, Jan 15, 2000.
Wolters-Geldof MJ, Cats VM, and Bruschke AV. Clinical methods to determine coronary flow and myocardial perfusion. Int J Card Imaging 13(2): 79–94; discussion 95–97, 1997.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kabal, J., Lagerman, B.K. Myocardial Hemodynamics During Exercise Treadmill Test By a Computer-Aided Clinical Decision System. Cardiovasc Eng 5, 171–185 (2005). https://doi.org/10.1007/s10558-005-9071-0
Issue Date:
DOI: https://doi.org/10.1007/s10558-005-9071-0