Abstract
Purpose
The definitive impacts of intensive lipid-lowering therapy (LLT) on plaque stabilization and the relationship between the key markers during LLT and plaque stability remain unquestioned. Thus, these meta-analysis and meta-regression intend to holistically evaluate the influence exerted by rigorous LLT on the minimum fibrous cap thickness (FCT) and maximum lipid arc as discerned through optical coherence tomography (OCT). This study further scrutinizes the correlation of this impact with variations in high-sensitivity C-reactive protein (hs-CRP), low-density lipoprotein cholesterol (LDL-C), or additional parameters within patients diagnosed with coronary artery disease (CAD).
Methods
Comprehensive searches were conducted on platforms including PubMed, Embase, and the Cochrane Library for randomized controlled trials (RCTs) published until June 1, 2023. The search was language agnostic and targeted RCTs elaborating on the correlation between high-intensity statin therapy or statins used concomitantly with other lipid-lowering medications and the minimum FCT and maximum lipid arc as assessed by OCT. The meta-analyses were executed employing a standard mean difference (SMD) algorithm with random-effects on continuous variables. These methodologies align with the Preferred Reporting Items for Systematic and Meta-analysis (PRISMA) guidelines.
Results
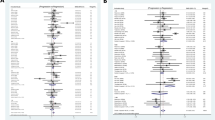
A spectrum of 12 RCTs engaging 972 patients were identified and mobilized for these analyses. Meta-analysis outcomes depicted a conspicuous correlation between intensive LLT and an enhanced minimum FCT (12 studies with 972 participants; SMD, 0.87; 95% CI, 0.54 to 1.21; P < 0.01), reduced maximum lipid arc (9 studies with 564 participants; SMD, −0.43; 95% CI, −0.58 to −0.29; P < 0.01). Meta-regression analysis has determined an association of elevated minimum FCT with decreased LDL-C (β, −0.0157; 95% CI, −0.0292 to −0.0023; P = 0.025), total cholesterol (TC) (β, −0.0154; 95% CI, −0.0303 to −0.0005; P = 0.044), and apolipoprotein B (ApoB) (β, −0.0209; 95% CI, −0.0361 to −0.0057; P = 0.022). However, no significant association was discerned relative to variations in hs-CRP/CRP (β, −0.1518; 95% CI, −1.3766 to −1.0730; P = 0.772), triglyceride (TG) (β, −0.0030; 95% CI, −0.0258 to −0.0318; P = 0.822), and high-density lipoprotein cholesterol (HDL-C) (β, 0.0313; 95% CI, −0.0965 to 0.1590; P = 0.608). Subsequent subgroup meta-analysis demonstrated that high-intensity statin therapy (5 studies with 204 participants; SMD, 1.03; 95% CI, 0.67 to 1.39; P < 0.01), as well as a combinative approach including PCSK9 antibodies and statins (3 studies with 522 participants; SMD, 1.17; 95% CI, 0.62 to 1.73; P < 0.01) contributed to an increase in minimum FCT. Parallelly, high-intensity statin therapy (4 studies with 183 participants; SMD, −0.42; 95% CI, −0.65 to −0.19; P < 0.01) or the combined application of PCSK9 antibodies and statins (2 studies with 222 participants; SMD, −0.98; 95% CI, −1.26 to −0.70; P < 0.01) was evidenced to decrease the maximum lipid arc.
Conclusions
Intensive LLT, mainly high-intensity statin therapy and combined PCSK9 antibody with statin, has a beneficial effect on coronary plaque stabilization derived from OCT in patients with CAD. Coronary plaque stabilization is primarily due to lipid-lowering effect, not anti-inflammatory effect. Moreover, the lipid-lowering effect has nothing to do with the changes in HDL-C and TG, but is mainly related to the reduction of LDL-C, TC, and ApoB.




Similar content being viewed by others
Data Availability
The data in the current meta-analysis are publicly available from the original literature and supplementary material.
Abbreviations
- LLT:
-
lipid-lowering therapy
- PCSK9:
-
proprotein convertase subtilisin/kexin type 9
- EPA:
-
eicosapentaenoic acid
- DHA:
-
docosahexaenoic acid
- IPE:
-
icosapent ethyl
- CAD:
-
coronary artery disease
- ASCVD:
-
atherosclerotic cardiovascular disease
- ACS:
-
acute coronary syndrome
- SMD:
-
standard mean difference
- RCTs:
-
randomized controlled trials
- OCT:
-
optical coherence tomography
- Minimum FCT:
-
Minimum fibrous cap thickness
- TCFA:
-
thin-cap fibroatheroma
- hs-CRP:
-
high-sensitivity C-reactive protein
- TC:
-
total cholesterol
- TG:
-
Triglyceride
- LDL-C:
-
low-density lipoprotein cholesterol
- HDL-C:
-
high-density lipoprotein cholesterol
- ApoB:
-
apolipoprotein B
- HTG:
-
hypertriglyceridemia
References
Jebari-Benslaiman S, Galicia-García U, Larrea-Sebal A, Olaetxea JR, Alloza I, Vandenbroeck K, Benito-Vicente A, Martín C. Pathophysiology of atherosclerosis. Int J Mol Sci. 2022;23:3346.
Johnson TW, Räber L, di Mario C, Bourantas C, Jia H, Mattesini A, Gonzalo N, de la Torre Hernandez JM, Prati F, Koskinas K, et al. Clinical use of intracoronary imaging. Part 2: acute coronary syndromes, ambiguous coronary angiography findings, and guiding interventional decision-making: an expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2019;40:2566–84.
Taron J, Foldyna B, Mayrhofer T, Osborne MT, Meyersohn N, Bittner DO, Puchner SB, Emami H, Lu MT, Ferencik M, et al. Risk stratification with the use of coronary computed tomographic angiography in patients with nonobstructive coronary artery disease. JACC Cardiovasc Imaging. 2021;14:2186–95.
Araki M, Park SJ, Dauerman HL, Uemura S, Kim JS, Di Mario C, Johnson TW, Guagliumi G, Kastrati A, Joner M, et al. Optical coherence tomography in coronary atherosclerosis assessment and intervention. Nat Rev Cardiol. 2022;19:684–703.
Biccirè FG, Budassi S, Ozaki Y, Boi A, Romagnoli E, Di Pietro R, Bourantas CV, Marco V, Paoletti G, Debelak C, et al. Optical coherence tomography-derived lipid core burden index and clinical outcomes: results from the CLIMA registry. Eur Heart J Cardiovasc Imaging. 2023;24:437–45.
Jiang S, Fang C, Xu X, Xing L, Sun S, Peng C, Yin Y, Lei F, Wang Y, Li L, et al. Identification of high-risk coronary lesions by 3-vessel optical coherence tomography. J Am Coll Cardiol. 2023;81:1217–30.
Räber L, Koskinas KC, Yamaji K, Taniwaki M, Roffi M, Holmvang L, Garcia Garcia HM, Zanchin T, Maldonado R, Moschovitis A, et al. Changes in coronary plaque composition in patients with acute myocardial infarction treated with high-intensity statin therapy (IBIS-4): a serial optical coherence tomography study. JACC Cardiovasc Imaging. 2019;12:1518–28.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, Chapman MJ, De Backer GG, Delgado V, Ference BA, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111–88.
Hu Y, Hu FB, Manson JE. Marine omega-3 supplementation and cardiovascular disease: an updated meta-analysis of 13 randomized controlled trials involving 127 477 participants. J Am Heart Assoc. 2019;8:e013543.
Bohula EA, Giugliano RP, Cannon CP, Zhou J, Murphy SA, White JA, Tershakovec AM, Blazing MA, Braunwald E. Achievement of dual low-density lipoprotein cholesterol and high-sensitivity C-reactive protein targets more frequent with the addition of ezetimibe to simvastatin and associated with better outcomes in IMPROVE-IT. Circulation. 2015;132:1224–33.
Koskinas KC, Gencer B, Nanchen D, Branca M, Carballo D, Klingenberg R, Blum MR, Carballo S, Muller O, Matter CM, et al. Eligibility for PCSK9 inhibitors based on the 2019 ESC/EAS and 2018 ACC/AHA guidelines. Eur J Prev Cardiol. 2021;28:59–65.
Gao F, Wang ZJ, Ma XT, Shen H, Yang LX, Zhou YJ. Effect of alirocumab on coronary plaque in patients with coronary artery disease assessed by optical coherence tomography. Lipids Health Dis. 2021;20:106.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng HY, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj. 2019;366:l4898.
Habara M, Nasu K, Terashima M, Ko E, Yokota D, Ito T, Kurita T, Teramoto T, Kimura M, Kinoshita Y, et al. Impact on optical coherence tomographic coronary findings of fluvastatin alone versus fluvastatin + ezetimibe. Am J Cardiol. 2014;113:580–7.
Komukai K, Kubo T, Kitabata H, Matsuo Y, Ozaki Y, Takarada S, Okumoto Y, Shiono Y, Orii M, Shimamura K, et al. Effect of atorvastatin therapy on fibrous cap thickness in coronary atherosclerotic plaque as assessed by optical coherence tomography: the EASY-FIT study. J Am Coll Cardiol. 2014;64:2207–17.
Nishio R, Shinke T, Otake H, Nakagawa M, Nagoshi R, Inoue T, Kozuki A, Hariki H, Osue T, Taniguchi Y, et al. Stabilizing effect of combined eicosapentaenoic acid and statin therapy on coronary thin-cap fibroatheroma. Atherosclerosis. 2014;234:114–9.
Hou J, Xing L, Jia H, Vergallo R, Soeda T, Minami Y, Hu S, Yang S, Zhang S, Lee H, et al. Comparison of intensive versus moderate lipid-lowering therapy on fibrous cap and atheroma volume of coronary lipid-rich plaque using serial optical coherence tomography and intravascular ultrasound imaging. Am J Cardiol. 2016;117:800–6.
Wang Z, Cho YS, Soeda T, Minami Y, Xing L, Jia H, Aguirre A, Vergallo R, Lee H, Fujimoto JG, et al. Three-dimensional morphological response of lipid-rich coronary plaques to statin therapy: a serial optical coherence tomography study. Coron Artery Dis. 2016;27:350–6.
Nishiguchi T, Kubo T, Tanimoto T, Ino Y, Matsuo Y, Yamano T, Terada K, Emori H, Katayama Y, Taruya A, et al. Effect of early pitavastatin therapy on coronary fibrous-cap thickness assessed by optical coherence tomography in patients with acute coronary syndrome: the ESCORT study. JACC Cardiovasc Imaging. 2018;11:829–38.
Ye H, Wang S, Hu Y, He F, Ju J, Cui H, Chen X. Therapeutic effects of different Atorvastatin doses on vulnerable plaques in coronary arteries assessed by intracoronary optical coherence tomography. Medicine (Baltimore). 2018;97:e11718.
Hougaard M, Hansen HS, Thayssen P, Maehara A, Antonsen L, Junker A, Mintz GS, Jensen LO. Influence of ezetimibe on plaque morphology in patients with ST elevation myocardial infarction assessed by optical coherence tomography: an OCTIVUS sub-study. Cardiovasc Revasc Med. 2020;21:1417–24.
Kita Y, Watanabe M, Kamon D, Ueda T, Soeda T, Okayama S, Ishigami K, Kawata H, Horii M, Inoue F, et al. Effects of fatty acid therapy in addition to strong statin on coronary plaques in acute coronary syndrome: an optical coherence tomography study. J Am Heart Assoc. 2020;9:e015593.
Nicholls SJ, Kataoka Y, Nissen SE, Prati F, Windecker S, Puri R, Hucko T, Aradi D, Herrman JR, Hermanides RS, et al. Effect of evolocumab on coronary plaque phenotype and burden in statin-treated patients following myocardial infarction. JACC Cardiovasc Imaging. 2022;15:1308–21.
Räber L, Ueki Y, Otsuka T, Losdat S, Häner JD, Lonborg J, Fahrni G, Iglesias JF, van Geuns RJ, Ondracek AS, et al. Effect of alirocumab added to high-intensity statin therapy on coronary atherosclerosis in patients with acute myocardial infarction: the PACMAN-AMI randomized clinical trial. Jama. 2022;327:1771–81.
Ozaki Y, Garcia-Garcia HM, Beyene SS, Hideo-Kajita A, Kuku KO, Kolm P, Waksman R. Effect of statin therapy on fibrous cap thickness in coronary plaque on optical coherence tomography - review and meta-analysis. Circ J. 2019;83:1480–8.
Budoff MJ, Bhatt DL, Kinninger A, Lakshmanan S, Muhlestein JB, Le VT, May HT, Shaikh K, Shekar C, Roy SK, et al. Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial. Eur Heart J. 2020;41:3925–32.
O'Donoghue ML, Giugliano RP, Wiviott SD, Atar D, Keech A, Kuder JF, Im K, Murphy SA, Flores-Arredondo JH, López JAG, et al. Long-term evolocumab in patients with established atherosclerotic cardiovascular disease. Circulation. 2022;146:1109–19.
Ridker PM, Howard CP, Walter V, Everett B, Libby P, Hensen J, Thuren T. Effects of interleukin-1β inhibition with canakinumab on hemoglobin A1c, lipids, C-reactive protein, interleukin-6, and fibrinogen: a phase IIb randomized, placebo-controlled trial. Circulation. 2012;126:2739–48.
Gao D, Hua R, Jiesisibieke D, Ma Y, Li C, Wu S, Ma Q, Xie W. C-reactive protein and coronary atheroma regression following statin therapy: a meta-regression of randomized controlled trials. Front Cardiovasc Med. 2022;9:989527.
Ginsberg HN, Packard CJ, Chapman MJ, Borén J, Aguilar-Salinas CA, Averna M, Ference BA, Gaudet D, Hegele RA, Kersten S, et al. Triglyceride-rich lipoproteins and their remnants: metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies-a consensus statement from the European Atherosclerosis Society. Eur Heart J. 2021;42:4791–806.
Peterson BE, Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, Juliano RA, Jiao L, Doyle RT Jr, et al. Treatment with icosapent ethyl to reduce ischemic events in patients with prior percutaneous coronary intervention: insights from REDUCE-IT PCI. J Am Heart Assoc. 2022;11:e022937.
Nicholls SJ, Lincoff AM, Garcia M, Bash D, Ballantyne CM, Barter PJ, Davidson MH, Kastelein JJP, Koenig W, McGuire DK, et al. Effect of high-dose omega-3 fatty acids vs corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: the STRENGTH randomized clinical trial. Jama. 2020;324:2268–80.
Feig JE, Hewing B, Smith JD, Hazen SL, Fisher EA. High-density lipoprotein and atherosclerosis regression: evidence from preclinical and clinical studies. Circ Res. 2014;114:205–13.
Kim HJ, Jeong S, Oh YH, Park SJ, Cho Y, Park SM. Changes in high-density lipoprotein cholesterol with risk of cardiovascular disease among initially high-density lipoprotein-high participants. Cardiovasc Diabetol. 2023;22:71.
Navarese EP, Robinson JG, Kowalewski M, Kolodziejczak M, Andreotti F, Bliden K, Tantry U, Kubica J, Raggi P, Gurbel PA. Association between baseline LDL-C level and total and cardiovascular mortality after LDL-C Lowering: a systematic review and meta-analysis. Jama. 2018;319:1566–79.
Masson W, Lobo M, Siniawski D, Molinero G, Masson G, Huerín M, Nogueira JP. Role of non-statin lipid-lowering therapy in coronary atherosclerosis regression: a meta-analysis and meta-regression. Lipids Health Dis. 2020;19:111.
Acknowledgements
We would like to thank all participants and all peer reviewers for their opinions and suggestions.
Funding
This research was supported by grant from the National Natural Science Foundation of China (81970262 to PJW).
Author information
Authors and Affiliations
Contributions
SL and PW conceived and designed this study. SL and JH drafted the first version of the manuscript. PZ and PW provided critical revision of the manuscript for important intellectual content. SL, JH, JW, YY, DW, DL, and XW carried out acquisition, statistical analysis, or interpretation of data. PW provided the funding support.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Research Involving Human Participants and/or Animals
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 229 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, S., Hou, J., Wan, J. et al. Effect of Intensive Lipid-Lowering Therapy on Coronary Plaque Stabilization Derived from Optical Coherence Tomography: a Meta-analysis and Meta-regression. Cardiovasc Drugs Ther (2023). https://doi.org/10.1007/s10557-023-07511-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-023-07511-7